-
Welcome to Celiac.com!
You have found your celiac tribe! Join us and ask questions in our forum, share your story, and connect with others.
-
Celiac.com Sponsor (A1):
Celiac.com Sponsor (A1-M):
-
Get Celiac.com Updates:Support Celiac.com!
Search the Community
Showing results for tags 'dermatitis'.
-
Celiac.com 12/21/2017 - After a lot of trial and error we celiacs learn, often the hard way, to eliminate foods that are poisonous to our bodies. Sadly, we often forget about what "goes onto" our skin. Since the skin is the living outer layer of our bodies it absorbs not only water and oils, it also absorbs cosmetics that can be poisonous to our celiac bodies, most specifically those of us afflicted with dermatitis herpetiformis (often called celiac disease of the Skin). Men, before you set this article aside, thinking it's only for women and you are exempt, please read on. One of 133 Americans has a wheat-related allergy according to CNN.com. We have a tendency not to group toothpaste and lip-glosses with cosmetics, and we usually ignore vitamins and medications when researching celiac disease and dermatitis herpetiformis. We forget to ask our hairdresser what products they are using and whether they contain wheat or gluten, and glibly apply night creams (to absorb into our skin as we sleep) and mud packs that promise similar benefits. Inquiring into the gluten content of cosmetics, I contacted more than twenty leading companies, then I waited. I was discouraged, particularly by the blatant rudeness of some of the responses I received. Meanwhile, I had to learn whether gluten could be absorbed through the skin. Some websites answered that question with a direct "no". Even some physicians responded saying "no". However, since the skin is the largest living organ in the body and it does absorb various oils and emollients, listing gluten-containing components of medicinal and non-medicinal ingredients allows consumers with celiac disease (celiac disease) or wheat allergies to make informed choices when purchasing and/or consuming natural health products. It enables them to avoid gluten in quantities that may trigger adverse reactions. There are numerous articles on dermatitis herpetiformis and celiac disease making claims so contradictory that it is no wonder we are confused. And I'm not talking about accidental ingestion of gluten. Some such articles claim that trace amounts of gluten One article insists that the skin is not going to absorb gluten, even though our skin is a living organism that can absorb suntan lotions, trans-dermal drugs, etc. It is so susceptible to absorption that when you place a slice of onion in your sock you will taste it in your mouth the following day. How can these websites make such contrary claims? The skin absorbs flavors as well as creams containing gluten. On the other hand, "Glutino" had an article on record, written on September 14, 2010, regarding "Hidden Gluten in Health and Beauty Products". It states that if you apply hand lotion that contains gluten and then prepare food you are exposing yourself to accidental ingestion and your food to cross contamination. They suggest a site called: naturallydahling.com, a site that lists gluten-containing ingredients commonly used in cosmetics. Research proving the full extent of how much your skin absorbs is still unavailable, but to those who believe that "what goes on, goes in", the cosmetic industry is full of unknowns. The size of gluten molecules suggests that they may not be able to pass through the skin, but chemicals and technology designed to enhance skin absorption are already present, if not prevalent, in the cosmetic industry. These chemicals are potentially dangerous and often go untested for negative health effects, yet are widespread in lotions, antiperspirants, perfumes and the "Great Mother Market" anti-wrinkle cosmetics. Since the cosmetic industry is self-regulated it is more important than ever to carefully read labels and use natural or organic products whenever possible. If you find yourself reacting to a particular cosmetic, it is possible that you may have an increased sensitivity to gluten, an allergy or even dermatitis herpetiformis. But wait a minute! Aren't we told that gluten cannot pass through the skin? I suffered terribly from the use of an "Anti-Frizz" product for my hair that caused a massive outbreak of dermatitis herpetiformis. I should have read the label all the way down to the end. I would have found, in very small print, "wheat germ oil". When researching for this article, I wrote to the company and mentioned my problems with their product. I received an apology and a sample of their "new and improved" "Frizz-Ease" product. They obviously do not know their own products and the fancy names they use are as confusing to them as they are to me. The "new and improved" product contained Avena Sativa, the Latin name for OAT. I was also told that I likely just had "hives" on the back of my scalp, as oats are still somewhat controversial. Some research suggests that oats in themselves are gluten free, but that they are virtually always contaminated with other grains during cultivation, harvest, distribution or processing. Recent research indicates that a protein naturally found in oats (avenin) contains peptide sequences closely resembling some peptides from wheat gluten. The oat peptides caused mucosal inflammation in significant numbers of celiac disease sufferers. Some examination results show that even oats that are not contaminated with wheat particles may be dangerous. Again, I was told not to introduce oats into my diet, or use oatmeal as a facial mask until I had been free of a dermatitis herpetaformis outbreak for at least a year. Thus far I have not been able to get relief for that long. It seems the celiac or those who suffer from dermatitis herpetiformis {and let's face it, most people suffering from dermatitis herpetaformis have celiac disease} have to apply the rule of "caveat emptor" - Let the buyer beware. Tolerance to gluten varies among individuals with celiac disease and there are limited clinical scientific data on a threshold for the amount of gluten required to initiate or maintain an immunological reaction in celiac disease patients. "Therefore there is no clear consensus on a safe gluten threshold level." The Dermatologist I see at The University of British Columbia Hospital has told me to tell people in restaurants that gluten is poison to my system and I can become very ill from ingesting gluten. They are a little more careful before telling me a dish is gluten free, and hopefully through education the cosmetic industry is going to improve its testing and cease glibly stating things as "fact" when they simply do not know. Industries that produce over-the-counter medications and vitamin supplement, especially those that may contain gluten as a binding agent, should also be scrutinized. We have come a long way, but large challenges are still ahead. One of our biggest challenges is reading the labels on these products. One almost needs to carry a magnifying glass when shopping. Cosmetics, which include hair products, soaps, perfumes and toothpastes also run us into problems, often big, "itchy" problems. The male celiac/dermatitis herpetaformis experience can also include outbreaks from any product that comes into contact with the skin and particularly those that "stay" on the hair or skin. Who would have known that sun tan lotions could contain wheat germ oil? It is difficult enough to eliminate words such as "triticum vulgare" the Latin name of wheat or "wheat germ" containing ingredients! In preparation for this article, I contacted the following companies: Avon, Clairol, Clarins, Clinique, Coty, Covergirl, Estee Lauder, Garnier, John Frieda, John Paul Mitchell, L'Oreal, Mabelline, Marcelle, Neutrogena, Olay, Pantene, Revlon, and companies that go under general all-encompassing headings such as "Life Brand". This can be a daunting task, and "gluten free" and "wheat free" are not the same thing. Some of the things that I learned in this rather massive undertaking include the rule of "Pac Man". Companies are sometimes taken over by bigger companies and when this occurs their rules change. A company that at one time did not test on animals or use machines that were cleaned prior to using products claiming to be gluten free are now glibly adopting the "new bigger and better". I was shocked to find out that some of the containers from the smaller company were still being used after these PAC MAN take-overs, to save on manufacturing costs. And, remember, once several ingredients are combined the "organic" ingredient probably ceases to be "organic". Some women (and men, you are not exempt here) expect to pay a higher price for a luxury brand assuming that the gorgeous bottle of eye cream sold at Saks for $60.00 is going to work better than the $1.99 tube on the clearance rack of a local store. Just ensure the product has not reached its "sell by" date because it may all be psychological. What you have to concern yourself about, as a celiac patient or a person with dermatitis herpetiformis, is whether there is gluten or wheat in that product. Before you splurge on an expensive product take the time to compare it to a similar product from one of their sister brands. Usually an online store (like Drugstore.com) will list the ingredients. Or you can check on a site like "Makeup Alley" which is a great resource, offering numerous reviews and you can ask questions of the extremely knowledgeable posters on this message board. Another great resource is a large paperback book, titled "Do not go to the Drugstore Without Me" written by Paula Begoin. When I purchased the books in 2001 it was in its 5th Edition. NB: This is not a book specifically for celiac disease or dermatitis herpetiformis, but it was in this book that I found out about "Glutamic Acid". It is derived from wheat gluten and is an amino acid that can have water binding properties for the skin. It also explains glycerylesters that form a vast group of ingredients that are a mixture of fatty acids, sugars, and non-volatile alcohols. These fats and oils are used in cosmetics as emollients and lubricants as well as binding and thickening agents. At the back of this book is a list of the companies that do not test on animals and those that do, but again, the PAC MAN Rule applies. I purchased the book for myself, my daughter, and daughter-in-law, specifically because when my daughter was in her twenties she seemed to think she simply must buy her shampoo from the hairdresser because only $45.00 shampoo was good enough for her hair. It was a big eye opener when she moved out of home and had to purchase it herself! I believe that the more we know about beauty products and the beauty industry the wiser our purchases will be. Consider, for instance, the cost of research and development for say, L'Oreal who develop formulas that can be used in Garnier Shampoos ($3.99) and Kerastase shampoo ($29.99) It doesn't take long to realize that it is a good idea to compare products at different ends of the price scale. Sometimes, two products from two different brands will have the same patent number. The difference is in the non-active ingredients, which give it a unique texture, scent and/or color. Also, it is wise to photo-copy, and even apply plastic covering to lists of "safe" beauty products, just as it is wise to keep a copy of "safe" and "unsafe" foods on hand when you go shopping. When you cannot even pronounce some of the words used in foods and beauty products how can you be expected to remember what is safe to apply to your hair and skin? I received a very nice letter from Teresa Menna, Manager at L'Oreal in Quebec who told me that L'Oreal has abolished gluten in the composition of L'Oreal products. However, on reading more literature I find that Garnier is a mass market cosmetic brand of L'Oreal, and L'Oreal is part of the Group P&G. P&G stands for Proctor and Gamble and P&G Beauty brands can be found on the site:_ http://pgbeautygroomingscience.com/product.php {The Company Garnier Laboratories was started in 1906 and acquired by L'Oreal in the 1970's}. I was unaware prior to researching this article that L'Oreal owned Kerastase, or that L'Oreal had purchased the MAC Cosmetic line, or that the KAO Brands Company owns Ban, Biore, Jergens and John Frieda. Here are some of the ingredients you might find in cosmetics that could indicate wheat or gluten: Avena Sativa {Latin name of oat, or "oat" term containing ingredients Hordeum distichon {Latin name of barley, or "barley" term containing ingredients} Hydrolyzed malt extract Hydrolyzed wheat protein Hydrolyzed vegetable protein Wheat germ Vitamin E Cyclodextrin Barley extract Fermented grain extract Oat (Avena sativa) Samino peptide complex Secale Cereale (Latin name of rye, or "rye" term containing ingredients) Stearyldimoniumhydroxypropyl Phytosphingosine extract Triticum vulgare {Latin name of wheat, or "wheat" term containing ingredients} Dextrin Dextrin palmitate Maltodextrin Sodium C8-16 Isoalkylsuccinyl Wheat Protein Sulfonate Yeast extract Anything with wheat in the name Thoughts: Some cute person gave the warning to ensure your lipstick is gluten free even if you don't have any skin issues. You could swallow some lipstick and get gluten in your system! Another person adds at the bottom of their e-mail to be sure to check guidelines regularly because company policies can change yearly and the list is only to be considered as "guidelines" and make-up ingredients can change each time a company changes or the scientists within that company decide to add to or delete certain products. {Makes you feel very safe as a celiac/dermatitis herpetaformis person doesn't it?} Another e-mailer suggested that mascara labeled as a "thickening agent" should be fearfully evaluated by the celiac/dermatitis herpetaformis person because the thickening agent is often "flour" and can sometimes cause eyelashes to fall out! Who knew? Noted on one e-mail, ‘So-called luxury brands can be laden with synthetic ingredients that do not cost more than their not so luxurious counterparts. True natural products that do perform, and there are a few such brands on the market, are authentic natural products that actually deliver what they promise and they truly do cost more to make because raw ingredients are much higher in cost. In fact, the cost is significantly higher when pure high grade ingredients are used. Letter received: " We have compiled a list of gluten free beauty products available on sephora.com. These products do not contain any wheat, rye or barley derivatives, and they were made in gluten-free laboratories so there is no chance of cross-contamination. But since you cannot be too careful, discontinue use of any product that triggers an attack." Letter received from Clairol:- "Gluten is a protein found in wheat, rye and barley. Although it is not added directly to our product, it may be present in fragrances. Due to the difficulty of tracing the source ingredients for the variety of fragrances used in manufacturing our products, we cannot provide specific levels of gluten content for any of our fragrance blends. Be aware that even products labeled "unscented" will still contain masking scent, therefore they may potentially contain gluten." Advertisement: World's Top Ten Cosmetic Companies : "Beauty begins on the inside, check out our post on ‘The Top Five Foods for Amazing Skin'" - Posted by The Greenster Team "I finally got up the nerve to go through my own (their) personal care products and look them up on "SKIN DEEP" and was very disappointed. The Company that makes my mascara (L'Oreal) tests on animals as does the company that makes my eyeliner (Covergirl) and my under eye concealer (Made by Physician's Formula) contains parabens" THE GREENSTER TEAM creates great articles, list the top ten cosmetic companies, what portion of the world's market they share and their hazard range. Letter received from Mabelline:- "Please find below most ingredients containing gluten (wheat and other grains). We invite you to take this list and compare it to our ingredient listings every time you buy a new product. When in doubt, do not hesitate to do your own research or contact your doctor." {Caveat Emptor} REMEMBER:- The truth is that there is no such thing as gluten free. The FDA has proposed a less than 20 ppm gluten -free standard in 2006. That was its first attempt to define the term gluten free, but the agency has yet to finalize it. The USDA is awaiting the FDA's decision before moving ahead. STILL WAITING. With the number of products making unregulated gluten free claims on the rise, the marketplace can be scary for consumers with gluten sensitivity and wheat allergies. Why hasn't the FDA finalized its 2006 definition of gluten free? As part of sweeping legislation known s FALCPA the Food Allergen Labelling and Consumer Protection Act of 2004, Congress ordered the FDA to define and permit the voluntary use of the term gluten free on the labeling of foods by August 2008. As directed, the FDA issued proposed gluten-free regulations on schedule but seems to have failed to follow through with a final ruling. There has been no explanation for the delay. Since the Cosmetic Industry is a self-regulating body it seems {appears, is assumed} that we the consumers are on our own as far as researching what goes on our skin and in our hair, because some of the letters I have received leave it to the celiac or dermatitis herpetiformis sufferer to research their own products. Even a letter from Avon states:- "Although Avon sells quality products, there is always possibility of contamination during manufacturing or changes/substitutions of ingredients. As with everything related to celiac disease, dermatitis herpetiformis and gluten Intolerance, products, ingredients and preparation may change over time. Your reactions to a specific product, ingredient may be different from the reactions of others. Like eating at a restaurant, you have to make a choice whether to consume/use a product. The list is meant to be a "guide" and does not guarantee that a product is 100% free of gluten. Dacia Lehman, Avon and GIG assume no responsibility for its use and any resulting liability or consequential damages is denied." LETTER: - Proctor and Gamble "The WHMIS rating is designed to rate raw materials and not formulated products such as ours. Nor are our consumer products required to be labeled under the Occupational Safety and Health Administration (OSHA) Hazard Communication Standard. Thus labelling of our products with WHMIS ratings or any other hazard rating should not be required by any state health and safety regulatory agencies." That letter is signed by Asela for the Pantene Team. LETTER:- May 2, 2012 - xyz@ca.loreal.com - "We have received your message and we will get back to you as soon as possible. Web Sites: Gluten-free Lifestyle: glutenfree-lifestyle.com (Gives gluten free products by type and by company) i.e.: deodorants, face & body wash, make-up, suntan lotion, toothpaste, moisturizer, lotion, shampoo & conditioner, shave cream, gels, after shave, laundry products, cleaners, soap, etc. Beauty Industry: Who Owns What? Glutino - Hidden Gluten in Health Products - Glutino & Gluten Free Pantry Blogs: www.gluten-free-cosmetic-counter.org Beauty Blogging Junkie Ebates Shopping Blog In The Makeup Lipstick Powder n'Paint Shop With a Vengeance Smarter Beauty Blog The Beauty Brains Sephora Sephora's iGoogle Beauty Portal References: Codex Standard for Foods for Special Dietary Use for Persons Intolerant to Gluten. Codex STAN 118 - 1979 ROME Government of Canada 2008 - Regulations Amending the Food and Drug Regulations (1220- Enhanced Labeling for Food Allergen and Gluten Sources and Added Sulphites) Health Canada 2007 - celiac disease and the Safety of Oats Labeling of Natural Health Products Containing Gluten - Health Canada Notice 2010
-
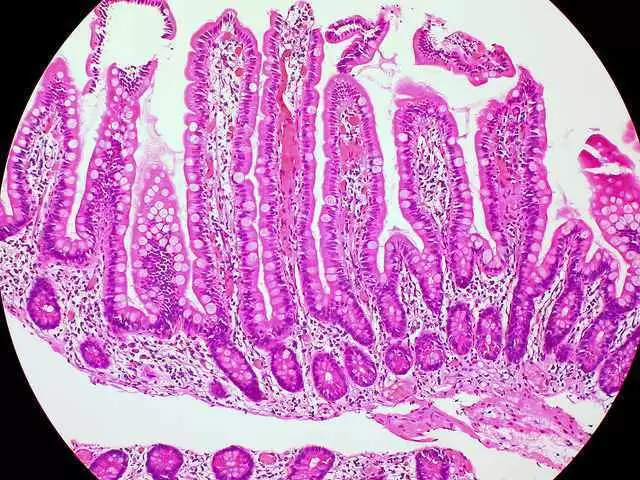
Celiac.com 10/21/2023 - Celiac disease, an autoimmune disorder triggered by gluten consumption, has long been associated with a range of digestive symptoms. However, the story doesn't end in the digestive tract. For some individuals, celiac disease unveils itself through an unexpected medium: their skin. This presentation is known as dermatitis herpetiformis, and it's a vital but often overlooked facet of celiac disease. Dermatitis herpetiformis, affectionately referred to as "DH" by some, is a chronic skin condition characterized by intensely itchy, blistering rashes. It might sound like a mere irritation, but DH is, in fact, the skin's way of echoing an underlying immune response to gluten ingestion. Just as celiac disease affects the small intestine, DH is its external manifestation, giving voice to the body's immunological revolt. In our in-depth exploration of dermatitis herpetiformis, we delve into the intricacies of this unique condition. We'll unravel its connection to celiac disease, exploring why it appears and how it's diagnosed. We'll discuss the unmistakable and sometimes bewildering symptoms, along with the challenges of managing this skin condition. Moreover, we'll guide you through treatment options and offer practical advice for living a gluten-free life to keep DH at bay. Despite its undeniable role in the larger celiac disease narrative, dermatitis herpetiformis remains an enigma for many. It's time to shed light on this aspect of celiac disease that affects the skin and, in doing so, empower those who face this condition to navigate its complexities with confidence and knowledge. So, let's embark on this enlightening journey, demystifying the link between celiac disease and the unexpected language of the skin: dermatitis herpetiformis. Unraveling the Connection Between Dermatitis Herpetiformis and Celiac Disease For those who have encountered dermatitis herpetiformis, the initial onset can be perplexing. Unexplained rashes and relentless itching lead many on a quest to uncover the root cause of their skin woes. This is where the intricate connection between dermatitis herpetiformis and celiac disease comes into play. Celiac disease is a well-known autoimmune disorder, triggered by the consumption of gluten—a protein found in wheat, barley, and rye. When someone with celiac disease ingests gluten, it initiates an immune response in the small intestine. This response damages the intestinal lining, impeding the absorption of nutrients and leading to a host of gastrointestinal symptoms. So, what's the connection between celiac disease's internal battleground and the itchy rashes of dermatitis herpetiformis? The answer lies in the immune system's memory. Individuals with celiac disease have a particular genetic predisposition. When they consume gluten, their immune system recognizes it as an invader and produces antibodies, mainly tissue transglutaminase 2 (tTG-2). These antibodies don't limit their activity to the digestive tract; they circulate throughout the body. Here's where dermatitis herpetiformis makes its grand entrance. The same antibodies that target the small intestine are drawn to the skin. When they reach the skin's surface, they provoke an inflammatory response. This reaction results in the characteristic blistering and intense itching of DH. In essence, DH is the skin's way of expressing the body's rejection of gluten—manifesting on the exterior what celiac disease inflicts internally. But this dual-action response, where gluten triggers a reaction in both the intestines and the skin, also means that those with dermatitis herpetiformis often have underlying celiac disease. While not all celiacs experience DH, a substantial number do. As a result, diagnosing DH often leads to a celiac disease diagnosis, making it crucial to recognize the symptoms and understand the connection between these two conditions. The Symptoms of Dermatitis Herpetiformis Dermatitis herpetiformis is a skin condition known for its distinct and uncomfortable symptoms. Understanding these symptoms is crucial for timely diagnosis and management. Here, we delve into the key indicators of DH and how they affect those who experience this unique skin disorder. Intensely Itchy Skin: The hallmark symptom of DH is intense itching. Affected individuals often describe the itch as deep and unrelenting. This itchiness typically precedes the appearance of the rash and can be so severe that it significantly impacts a person's quality of life. Scratching the itchy areas can further exacerbate the condition. Blistering Rash: The most recognizable feature of DH is the appearance of a blistering rash. The rash typically consists of red, raised bumps or blisters filled with clear fluid. These eruptions often cluster together and create symmetrical patterns on the skin, appearing on both sides of the body. The rash's appearance can vary from person to person but is characterized by its tendency to group in clusters. Elbows, Knees, and Buttocks: DH often affects specific areas of the body, with a predilection for the extensor surfaces. This means that it frequently appears on the elbows, knees, and buttocks. However, the rash can also emerge on other body parts, including the scalp, back, and shoulders. Burning Sensation: In addition to itching, some individuals report a burning sensation or discomfort in the affected areas. This burning sensation can add to the overall discomfort and distress associated with the condition. Skin Lesions and Scarring: If left untreated, DH can lead to skin lesions, erosions, and secondary bacterial infections. Prolonged scratching or friction can result in scarring, which, in severe cases, may be permanent. Recurrence and Chronic Nature: DH tends to be a chronic condition with a relapsing-remitting pattern. Symptoms may improve and reappear over time, making it essential for individuals to have a long-term management plan. Understanding the symptoms of dermatitis herpetiformis is vital for early recognition and proper management. It is essential for affected individuals to seek medical attention for a definitive diagnosis and to initiate appropriate treatment, often in conjunction with managing the underlying condition, celiac disease. How To Diagnose Dermatitis Herpetiformis Diagnosing dermatitis herpetiformis can be challenging due to its resemblance to other skin conditions. However, a correct and timely diagnosis is crucial as it often points to an underlying condition, celiac disease. Here, we'll explore the key steps involved in diagnosing DH. Clinical Assessment: The diagnostic journey typically begins with a visit to a dermatologist. DH's hallmark symptom is its distinct blistering rash, but it can resemble other dermatological conditions like eczema, contact dermatitis, or even herpes. An experienced dermatologist will conduct a thorough clinical assessment, taking into account the specific characteristics of the rash, its distribution, and the accompanying symptoms such as itching and burning. The presence of the rash's unique pattern, which typically forms in clusters and symmetrical groups, can be a telling sign. Skin Biopsy: In many cases, a definitive diagnosis of DH requires a skin biopsy. A small sample of the affected skin is taken and examined under a microscope. The biopsy typically reveals specific markers such as granular immunoglobulin A (IgA) deposits in the skin layers, a key indicator of DH. These IgA deposits, also found in the small intestine of those with celiac disease, provide a crucial link between DH and the underlying autoimmune condition. Blood Tests: Alongside a skin biopsy, blood tests can be conducted to detect elevated levels of antibodies associated with celiac disease, particularly IgA-tissue transglutaminase (tTG) and IgA-endomysial antibodies (EMA). Finding high levels of these antibodies in the bloodstream adds another layer of evidence linking DH to celiac disease. Response to a Gluten-Free Diet: Perhaps the most compelling diagnostic tool for DH is the patient's response to a gluten-free diet. If the rash and other symptoms improve or disappear with the elimination of gluten from the diet, it strongly suggests dermatitis herpetiformis in the context of celiac disease. The diagnosis of DH can be complex, requiring a combination of clinical expertise, laboratory tests, and a dietary evaluation. Once confirmed, patients can begin effective management of both the skin condition and their underlying celiac disease, often with significant improvements in their overall health and well-being. In the following section, we'll explore strategies for managing dermatitis herpetiformis. Home and Over the Counter Remedies for Symptoms of Dermatitis Herpetiformis While home remedies can provide some relief from itching, it's important to note that DH typically requires medical treatment, including a gluten-free diet. Be sure to consult a healthcare professional for proper diagnosis and treatment. Here are some home remedies that may help alleviate itching associated with dermatitis herpetiformis: Gluten-Free Diet: While not a prescription medication, adherence to a strict gluten-free diet is the cornerstone of DH treatment. Eliminating gluten from the diet can prevent the formation of new skin lesions and reduce the need for medications over time. Benadryl (consult a doctor before use in young children): First try the over the counter cream, but if that does work a member of Celiac.com's forum reports that the very best thing to stop DH itching is to grind up a 25mg pill of Benadryl (or perhaps get capsules and just open one) into two teaspoons of water, and then spread it over the rash and itchy areas with your finger. Just be careful not to use too much too often, as you can absorb the drug through the skin. Allegra (Fexofenadine): Those with DH report that taking Allegra, which, in the USA, is an over the counter allergy medication, provides relief. Be sure to read all package warnings before giving it to children. Kroger's Full Prescription Strength Athletes Foot Cream: Users have reported that this helped stop their itching. Cold Compress: Apply a cold, damp cloth or an ice pack to the affected area. This can help reduce inflammation and numb the itching sensation temporarily. Gluten-Free Oatmeal Bath: Adding colloidal oatmeal (available in drugstores) to your bathwater can soothe irritated skin. Soak in the oatmeal bath for 15-20 minutes and be sure the oatmeal is certified gluten-free. Baking Soda Bath: A baking soda bath may help relieve itching. Add a cup of baking soda to a lukewarm bath and soak in it for relief. Aloe Vera: Apply aloe vera gel directly to the affected area. Aloe vera has anti-inflammatory properties and can provide soothing relief. Calamine Lotion: Calamine lotion can help relieve itching and soothe the skin. Apply a thin layer to the affected area and allow it to dry. Topical Hydrocortisone Cream: Over-the-counter hydrocortisone creams can provide temporary relief from itching and inflammation. Follow the instructions on the product label. Keep Skin Moisturized: Apply a fragrance-free, hypoallergenic moisturizer to your skin regularly. Dry skin can worsen itching. Ben-Gay Cream: Some people with DH have reported that using Ben-Gay cream on the affected areas relieved the itchiness. Chiggerex cream: Some people with DH have reported that using Chiggerex cream on the affected areas relieved the itchiness. Avoid Irritants: Avoid foods high in iodine like seafoods and dairy products as iodine may exacerbate symptoms in some people with DH. Also avoid harsh soaps, fragranced products, and hot water, as they can exacerbate itching. Opt for gentle, hypoallergenic products. Wear Loose-Fitting Clothing: Tight clothing can irritate the skin. Choose loose-fitting, breathable fabrics to minimize friction. Antihistamines: Over-the-counter antihistamines may help reduce itching. Consult your doctor or pharmacist for the appropriate dosage and type. Niacin and Niacinamide (Vitamin B3): There is some evidence that niacin and niacinamide may offer some relief from DH symptoms. Stress Reduction: Stress can exacerbate itching. Engage in relaxation techniques such as deep breathing, meditation, or yoga to manage stress. Dietary Modifications: While not a home remedy, it's crucial to address the root cause of DH by following a strict gluten-free diet. Consult with a registered dietitian to ensure you are avoiding gluten-containing foods. Remember that these home remedies are not a substitute for medical treatment. If you suspect you have dermatitis herpetiformis or are experiencing severe itching, consult a dermatologist or healthcare provider for proper diagnosis and guidance on managing the condition, which typically includes a gluten-free diet and medication to control symptoms. Prescription Treatments for Symptoms of Dermatitis Herpetiformis Dermatitis herpetiformis is typically treated with prescription medications aimed at controlling the symptoms and underlying condition, which is celiac disease. The primary treatment for DH is a strict gluten-free diet, as DH is closely associated with gluten intolerance. Additionally, medications are often prescribed to manage the skin symptoms. Common prescription treatments for DH include: Dapsone: Dapsone is the most commonly prescribed medication for DH. It is an oral medication that belongs to the sulfone class of drugs. Dapsone helps reduce skin inflammation, itching, and the formation of new blisters. It is usually started at a low dose and gradually increased as needed. Regular blood tests are necessary to monitor potential side effects, such as changes in blood cell counts. Topical Steroids: In addition to oral medications, topical corticosteroid creams or ointments may be prescribed to reduce itching and inflammation. These are applied directly to the affected skin and should be used as directed by a healthcare provider. Oral Corticosteroids: In cases of severe flare-ups or when Dapsone is not well-tolerated, oral corticosteroids like prednisone may be prescribed for short periods to quickly control symptoms. Long-term use of oral corticosteroids is generally avoided due to potential side effects. Sulfapyridine: Sulfapyridine is sometimes used as an alternative to Dapsone. It is also an oral medication that can help control DH symptoms. Like Dapsone, regular blood tests are necessary to monitor for side effects. Immunosuppressants: In some cases, immunosuppressive medications such as azathioprine or methotrexate may be prescribed to control DH symptoms. These medications work by suppressing the immune system's response that leads to skin inflammation. They are typically considered when other treatments are ineffective or not well-tolerated. It's crucial to work closely with a healthcare provider, preferably a dermatologist and a gastroenterologist, if you have dermatitis herpetiformis. They can properly diagnose the condition, monitor your progress, and adjust your treatment plan as needed. Additionally, regular follow-up appointments are important to assess the effectiveness of treatment and manage any potential side effects of medications. Remember that self-diagnosis and self-treatment are not recommended for DH, and medical guidance is essential for effective management.
- 9 comments
-
- blisters
- celiac disease
-
(and 8 more)
Tagged with:
-
Celiac.com 09/21/2023 - Gluten sensitivity is a chronic intolerance to gluten in people who have a genetic predisposition. It is thought to involve the immune system and can lead to various skin conditions. Celiac disease is one common form of gluten intolerance and can affect not only the digestive system but also the skin, endocrine system, nervous system, and blood. We know that a number of skin disorders are associated with celiac disease. Psoriasis, a chronic inflammatory skin condition, has shown improvement when individuals adopt a gluten-free diet. Specifically, palmoplantar pustulosis, a variant of psoriasis, and aphthous stomatitis, which causes recurring mouth ulcers, have responded positively to gluten elimination. Dermatitis herpetiformis, another skin disorder related to celiac disease genetically, has also seen significant improvement with a gluten-free diet. However, atopic dermatitis, another prevalent long-term skin condition, has produced inconsistent results with gluten removal. Further research is needed to draw more definitive conclusions. Hereditary angioedema has shown an association with gluten intolerance in some cases, with symptomatic benefits observed after adopting a gluten-free diet. Vitiligo and linear IgA bullous dermatosis have also shown clinical evidence of improvement with a gluten-free diet. On the contrary, rosacea, a skin condition causing facial redness, has been linked to an increased risk of developing celiac disease. The Research Team A team of researchers recently set out to examine the association between gluten intolerance and skin disorders. The research team included Vaibhav Vats, Pallavi Makineni, Sarah Hemaida, Anum Haider, Sachin Subramani, Navjot Kaur, Amna Naveed Butt, Renee Scott-Emuakpor, Mohammad Zahir, Midhun Mathew, and Javed Iqbal. They include one Physician, Istanbul Okan University, Istanbul, TUR; and are otherwise variously affiliated with the department of Internal Medicine, Smt. Kashibai Navale Medical College & General Hospital, Mumbai, IND; the department of Neurosurgery, Mayo Hospital, Lahore, Pakistan; the department of Medicine/internal medicine, Allama Iqbal Medical College, Lahore, PAK; the Department of Internal Medicine, Pennsylvania Hospital, Philadelphia, USA; the department of Medicine, Ayub Medical College, Abottabad, Pakistan, Abottabad , PAK; the department Dermatology, University of Miami Miller School of Medicine, Miami, USA; the department of Medicine, Government Medical College, Amritsar, Amritsar, IND; the department of Internal medicine, ESIC medical college and hospital, Gulbarga, IND; the department of Internal medicine, Img helping hand, Karachi, PAK; and the department of Medicine, All India Institute of Medical Sciences, Bhubaneswar, Bhubaneswar, IND. Their review highlights the potential impact of gluten intolerance on various skin conditions and the potential therapeutic benefits of a gluten-free diet for managing symptoms. However, more clinical trials and observational studies are needed to fully understand the underlying mechanisms and provide definitive dietary recommendations for these conditions. Read more in Cureus.com
- 1 comment
-
- associations
- celiac
- (and 8 more)
-
Celiac.com 09/13/2016 - Six times from 2003 – 2005, I had a mysterious full-bodied, itchy, blistery rash that landed me in the emergency room the first time, where seven doctors shook their heads. The ER physicians agreed that it was a "systemic chemical reaction" and tried to identify what I could have been exposed to. A dairy allergy was ruled out immediately since I have been completely dairy-free for twenty years. For the next three years, between hiding from the world for the ten days of intense itching and for the six weeks it took my skin to heal after an outbreak, I saw numerous dermatologists, internists, gastroenterologists, allergists and chiropractors. No one could figure out what was causing this miserable rash. I finally met the "best diagnostician" according to Denver's 5280 Magazine who told me he would figure out what was causing my plight, but that it wouldn't be fun. At that point, I was willing to take any test to identify what my enemy was. I endured ninety-eight needle sticks (who's counting?) eight skin biopsies, invasive scopes and tests for allergies, rheumatoid arthritis, diabetes, thyroid disease and a host of other procedures. The skin biopsies erroneously concluded that I had scabies. Scabies are biting mites that leave bumps on the skin. It couldn't have been mites, because my husband, who lives in the same environment, didn't have a bump on his body. There was only one test that I did not pass – elevated levels of IgG antibodies in my blood. My doctor suggested that the rash could be correlated with gluten consumption and recommended that I try a gluten free diet. After being vigilant for several months, five out of seven long-term chronic complaints, including the rash, gradually went away. Here's my understanding of the DH lifecycle. An intestine that cannot break down the protein gluten leaks it out of the intestine and into the bloodstream. The blood sees this as a foreign protein and over-produces the immunoglobulin G to attack it. The antibodies build up, and purge out through the skin causing the rash. Completely avoiding gluten eliminates the antibody buildup, and the rash. One clue that might have streamlined my diagnosis is the knowledge that the DH rash is symmetrical. If it appears on one elbow, it will appear on the other, etc. In my case, it appeared on both sides of my entire body from the neck down. Please understand, I am not a doctor and the following is not to be considered medical advice. I am sharing this to pass along a few things I've learned from personal experience, research and lectures on the subject with the hope of helping others who suffer from a chronic, pervasive, itchy rash. Initial Testing Since I had the eight skin biopsies, I've learned that immunofluroescent biopsies should have been taken of the healthy skin near the rash rather than of the actual bumps. I was never given this test. After all those tests, the elevated IgG was the only indication that gluten is the culprit. I endured what was considered the "gold standard" for diagnosing celiac disease, the upper GI scoping, and my gastroenterologist did not find any damage. I have since learned that the upper GI scoping is no longer thought to be the "gold standard" diagnostic process by many celiac experts because it is too random. If the doctor doesn't biopsy the intestines in exactly the right place, you may be deemed to be celiac-free when you actually have considerable intestinal damage several inches away from the biopsy site. Furthermore, people with DH may or may not experience damage to their small intestine. A study done in 2010 found that 67 percent of the time people with DH only have elevated IgG-TGA levels (1). My doctor divulged that there simply are not yet 100 percent conclusive tests for celiac disease. He said that the best way to be sure of the diagnosis is to observe that the chronic symptoms disappear over time by vigilantly following a gluten free diet. Residual Rashes Residual rashes can reappear for up to five years even though the person is following a gluten free diet. The accumulated antibodies purge in a histamine response (the rash) periodically through the skin. Horrible as an outbreak is, the rash is actually how the body cleanses itself of the antibodies. The good news is, rashes diminish in time with strict adherence to a gluten free diet. Ongoing Testing I've learned that the best way to monitor the healing process is to have the IgG antibodies tested once a year until they are in the normal range. The number should decline each year, which implies compliance to the gluten free diet and that residual rashes will diminish. Mine took several years to finally reach the normal range. Having IgGs in the normal range does not mean that I can ever go back to eating gluten. DH is a life-long condition controlled by a gluten-free, and often, a dairy-free diet. Some studies talk about a spontaneous remission. This is very rare. Other Triggers People who have a propensity to develop rashes need to be aware of other triggers. Iodine triggers the rash in people with DH. Seaweed, shellfish, especially shrimp and lobster should be avoided. Sushi wrapped in Nori seaweed has caused me to have an outbreak before. Watch out for thyroid medicine and water filters because both can contain iodine. Sunburns can cause rashes. If your skin is sensitive enough to get a rash, chances are, sun will irritate it and could trigger an outbreak. Stay in the shade, wear translucent zinc oxide sunscreen and avoid too much exposure. An overgrowth of Candida (yeast) can cause an outbreak. Candida is naturally present in the body. To avert an overgrowth, eliminate simple sugars from the diet. According to a study done at Rice University, 70 percent of the population have an overgrowth of Candida somewhere in their body(2) due to over-exposure to antibiotics, steroids and hormones. Women who are "estrogen dominant" may not be producing progesterone. This can happen during perimenopause and in menopause. According to the book What Your Doctor May Not Tell You About Menopause by John R. Lee and Virginia Hawkins(3), estrogen dominance causes autoimmune and histamine reactions in some people. This could be the reason that women who have eaten gluten for years without symptoms are suddenly are plagued when they are in their 40's or 50's. Pharmaceuticals can trigger rashes in people with DH. If there is a choice of two drugs and one says a side effect may be a rash, and a similar drug doesn't, opt for the one that doesn't say "rash" for a side effect. Inadvertent gluten consumption can also cause the rash. Gluten is in nearly every processed food, and in many cosmetics and drugs. Some mushrooms are even grown on gluten! Transglutaminase enzymes are used to revive aging fish and meats – to extend their shelf life and to make them look appetizing. Grocers do not have to declare that they add these enzymes because they are naturally occurring in the human body. Dr. Peter Green mentioned at a Gluten Intolerance Group conference that people with celiac disease develop antibodies to tissue transglutaminase, and that the addition of those enzymes may be causing people who are already sensitive to get sicker. The point is that even foods that are supposedly gluten free can contain small amounts of it. To be safe, test products with ELISA test strips. ELISA test strips are available at Open Original Shared Link. Since these strips are so expensive, this is also a website for everyone who uses them to post their results. I have learned a lot by reading this forum. Day-to-Day Life The longer I have been gluten free, the less tolerant my body has become. I've heard this anecdotally from others following the gluten-free diet. My DH is so severe, I react to even the most minor infractions. It makes eating out very difficult because cross-contamination is common and waiters are not always aware. I have a little test for waiters to decide whether to trust them to bring me a ‘safe' meal. I order a club soda with lemon before I order food. If the soda comes with lime, I know this waiter is not listening, and will be more likely to bring me something that could contain gluten. In restaurants that flunk my club soda test, I play it safe and order salad, a fruit plate or steamed vegetables. I've been to restaurants that tout a gluten free menu, only to be presented with a laminated disclaimer saying they are not liable for cross-contamination or inadvertent gluten after I order. How can anyone enjoy a meal with that kind of disclaimer? Not to mention the disruption of the conversation with your meal-mate when presented with a disclaimer card. It can be a little embarrassing! The most frustrating aspect of living with this is when accidental infractions occur. In November 2011, I wasn't feeling very well, so I took an aspirin and went to bed. Ten days later, the rash started appearing. It was a very bad rash, and I had to wear gloves to cover my hands that had doubled in size. I could not figure out what I had consumed that had gluten in it. My home is gluten free! I thought perhaps a product that I habitually used changed ingredients, so I read all the ingredients of everything in my house. Using the ELISA test strips, I tested 44 different products – foods, pharmaceuticals, over-the-counter drugs, cosmetics – everything that came in contact with my skin, or that I ate. Nothing I tested contained gluten. Then I remembered taking the aspirin. I tested it, and it contained gluten! I read the ingredients, the label said "Inactive ingredient: starch." It did not say what kind of starch. This happens in binders in pharmaceuticals too. The ingredients of pharmaceuticals will say "starch #3," and further investigation reveals this can alternate between wheat, tapioca, corn or potato. This means every time a prescription is refilled, it must be tested to be sure that particular batch wasn't made with wheat starch. I was in a car wreck and had to be taken to the emergency room. My sternum was broken, and I needed pain medication. The nurse offered me a pill and I asked if they would please make sure that it was gluten free. The nurse said, "pharmaceuticals are gluten free." (I've had pharmacists tell me this too – but as mentioned above, it is not true!) I said, "The reaction I get from consuming gluten is worse than the pain of this broken bone. Would you mind checking?" The nurse came back 30 minutes later and told me the pill did, indeed contain gluten. I went home in the middle of the night without any pain medication. I found a website the next morning that lists all gluten free pharmaceuticals, and asked my doctor to call in the specific brand of pain medication. The website is Open Original Shared Link. I have learned to keep a bottle on hand at home, and when I travel in case something like that ever happens again. I really wanted to eat the gluten free oats, so in 2009, I decided to go completely grain free for three months to cleanse myself for the "oat challenge." Then I made some oatmeal cookies with the gluten free oats. I took one bite, and waited ten days. Sure enough, the rash appeared on my legs. Through this experiment, I learned that I am not tolerant of even some "gluten free" foods. Through my studies of alternative diets and trying to discover the optimal way to eat to improve health, I have learned that a diet centered on eating vegetables, fruits, beans and some nuts and seeds improve the autoimmune system. Once the immune system is restored, (after strict adherence for several years), I've been told that it may be possible to undergo gluten desensitization under doctor's supervision. Locating a credible doctor to do this may be tricky, and deliberately exposing myself to gluten would take a lot of courage. However, I am considering this down the road with the hope that if I am inadvertently exposed to tiny amounts of gluten, I won't suffer through another rash. Since my reaction is so severe, I asked my doctor to write an undated letter on his letterhead "To Whom It May Concern" that states my reaction to gluten. I take this with me whenever I travel, just in case I was ever hospitalized, I could show the staff a letter from a bona fide medical doctor stating the severity of my situation. Without a letter, I am not sure if anyone would adhere to the strict gluten free guidelines I need to follow. Rash Remedies In those dismal three years before I was diagnosed, I was given mega doses of steroids, antibiotics, antihistamines, countless prescription creams, gels, histamine blocks, anti-viral drugs, anti-fungals and offered Dapsone. Since it took years to diagnose, well-meaning doctors offered a smattering of drugs to see what might work. Most of the drugs listed above were not the right medicine for DH. Steroids proved ineffective. Antivirals and antifungals did not work either. Dapsone is commonly given to people with DH who are not able to adhere to a gluten free diet. It is a strong drug originally given to lepers and has severe side effects. I'd rather live the gluten free lifestyle than take Dapsone. Once diagnosed, the two drugs that worked for me to ease symptoms for outbreaks were Zantac and liquid Hydroxizine. I am told that Zantac is a histamine block. It helped to reduce the number of itching days from ten to eight. I was also told to take it as precaution, if I felt I had inadvertently eaten gluten to thwart off an outbreak. I took the liquid hydroxizine around 4:00 o'clock in the afternoon when the histamines are highest, to ease the itching through the night. An un-exotic over-the-counter remedy that works is the clear calamine lotion from Walgreen's. There were days that I dreamed of taking a bath in that wonderful stuff! Another remedy recommended by a DH friend is a product made by Bayer called Domeboro Astringent Solution. It is a powder that is mixed with water and applied with a cloth to the affected area. It is said to give relief from the itching for several hours. Fluocinonide gel .05 percent is another remedy I have heard helps with the extreme itching. Fortunately, I have not had an outbreak since I learned about this remedy. Ever Onward Though my doctor recommended the gluten free diet, he didn't tell me how to do it, and I found there was a lot to learn! Luckily, during that time in the midst of outbreaks, I was attending cooking school. The school was not gluten free, but I took all of the methods and lessons home and converted everything I learned to be allergy free. The diagnosis and certification from the school launched me on an epicurean adventure and changed the course of my life. I started the Alternative Cook to help others who want to eat safe, delicious foods. If you are suffering with an incredibly itchy, pervasive rash, or know someone who is, consider that gluten could be the offender. Celiac disease is much more prevalent in this country than once thought. If you need moral support with DH, I'd love to hear from you. Sources: Dahlbom, Ingrid, Korponay-Szabo, Ilma R, Kovacs, Judit B, Szalai, Zsuzsana, Maki, Markku, Hansson, Tony. "Prediction of Clinical and Mucosal Severity of Coeliac Disease and Dermatitis Herpetiformus by Quantification of IgA/IgG Serum Antibodies to Tissue Transglutaminase." Journal of Pediatric Gastroenterology and Nutrition. Vol. 50(2), February 2010, P 140-146. "Biologists ID Defense Mechanism of Leading Fungal Pathogen. Psych Central. June 25, 2004. psychcentral.com. Lee, John R., Hawkins, Virginia. What Your Doctor May Not Tell You About Menopause. Mass Market Paperback. September, 2004.
- 13 comments
-
- dermatitis
- dermatitis herpetiformis
-
(and 2 more)
Tagged with:
-
TLDR: I have had dermatitis herpetiformis for several years now, but just recently it started becoming a lot worse. Despite going hyper militant on eating gluten free, removing virtually ALL cross reactors to gluten, replacing all of our pots/pans/utensils/etc. and replacing all of our detergents and bathroom products (AGAIN..) my gut is still inflamed from gluten and my gluten spots on my skin are getting worse and worse. I also fear that I may be developing depression, fibromyalgia and possibly other conditions BECAUSE of my gluten condition. Looking for advice on what I can try next, and any help would be much appreciated. So about 7 years ago (at the age of 22) I was diagnosed with dermatitis herpetiformis, and then sometime later after getting some additional bloodwork done, I was officially deemed to be Celiac (more on the “sometime later” below). Now for quite some time (up until fairly recently) I ate gluten free, BUT I will confess that I never really bothered to be militant about it. I always consumed gluten free foods only, but I didn’t care much about cross-contamination from eating out. I was still decently cognizant of sharing utensils, pots and pans, etc. and I though my bathroom products and laundry detergent were in the clear. For most of those years, I was overall completely fine, things were good, I wasn’t really all that itchy for the most part and my gluten spots didn’t bother me all that much. Until recently… Over the past 5 months or so, it feels like my body and my mind are just slowly deteriorating... I feel weak/fatigued all the time, despite getting the same amount of sleep as normal, if not more. My energy levels are shot and I often have a bit of a depressed mood overall throughout the day. My muscles have felt like they’ve atrophied too. And of course, my gluten spots and gut inflammation have been getting worse. All of my problems started occurring about 5 months ago when I had gotten bloodwork done for my gastro. Now I should also confess at this point that I had not gotten official bloodwork done to confirm that I was Celiac, because I just assumed that I was with my dermatitis herpetiformis diagnosis, but, my gastro recommended that I get the bloodwork done just to be sure. However, apparently this requires me to go on a gluten-filled diet for at least a week before they can be certain of the results (btw has anyone else been told this?! It seems f**king insane looking back at it now). So, I did so for about a week, got the bloodwork done and it was 100% confirmed at that point that I was Celiac. For anyone that has my condition, as you could imagine my life was a living hell for several weeks after that. So now that I’ve explained what has transpired up until this point, below I have listed everything my wife and I have tried to resolve this issue: 1) Foods/Drinks with known gluten in them had been absent from our house for several months at this point (just for reference) 2) We started with an elimination diet (carnivore/keto specifically), with the idea of getting totally better first (by basically eating the exact same stuff), and then reintroducing foods later to see what I react to. We are still on this diet to this day. Also, worth noting that we keep very careful track of our vitamins and minerals, and make sure our bodies get what is required. 3) For quite a while during this period, I had virtually removed ALL known cross reactors to gluten. This included eggs, ALL dairy, coffee, soy, virtually ALL gluten free grains, even a lot of foods with iodine in them (we replaced our salt with one that wouldn’t be iodized) 4) Alcohol use was cut down significantly. There has only been a day or two here and there where I had a few drinks, and when I did, it was either pure vodka or gin on the rocks with no additional ingredients. No other types of drink were consumed other than water. 5) Laundry detergent and all bathroom products were replaced with brands that were certified gluten free (a lot of stuff from Vanicream) 6) Our cast iron skillet, kitchen utensils (cooking and silverware), backing sheets, etc. were all replaced. Sponges and other equipment we use to clean dishes were also replaced. 7) Started a Food Journal to keep track of every single thing that I ate and how my gluten spots felt each day. This journal has not helped me much at all yet though, as my spots would be perfectly fine one day, but then really bad the next, and I literally ate the same exact thing for the past several days straight… No break in my routine whatsoever and it just feels random… 8) We have basically stopped eating out completely. All of our food is cooked at home, using the same pots/pans and utensils. So, with all of that being said… I’m here looking for any advice that anyone could offer. Any help or ideas or insight would be extremely helpful and much appreciated. I don’t know what to do from here, I just feel lost. I get the same bloodwork done every few months to see how I’m progressing, and each time my doctor tells me that I haven’t improved even slightly… He just keeps telling me that I’m still getting “glutened” somehow, but I just don’t see how that’s possible with everything that I’ve done. If you made it this far, thank you for taking the time to read my story.
- 6 replies
-
- dermatitis
- herpetiformis
-
(and 1 more)
Tagged with:
-
Celiac.com 04/25/2012 - In my experience growing up with undiagnosed celiac disease, I had to deal with several symptoms that my doctors had no answers for. One of the most frustrating of these was my skin troubles—dermatitis herpetiformis. After my experiences with misdiagnoses, and finally more recently, learning how to effectively get rid of dermatitis herpetiformis, I encourage parents to be particularly watchful for signs of dermatitis herpetiformis in their children, and I have some useful advice for those—children and adults—who have already been diagnosed with this annoying and sometimes quite troublesome rash. Since dermatitis herpetiformis occurs in 15 to 20% of celiacs, it’s worth any celiac’s time to learn more about this condition. By definition, dermatitis herpetiformis is a blistering and extremely itchy skin rash. It’s usually symmetrical in shape and is most commonly located on the elbows, knees, buttocks, and upper back. It’s common for people with dermatitis herpetiformis to have rashes appear in the same spot, and they can either be consistent or come and go. People can experience the rash on other parts of the body, and severity of symptoms can vary. Dermatitis herpetiformis is sometimes called the “gluten rash” or “celiac disease rash” because it occurs in people with a gluten intolerance or celiac disease. It is commonly misdiagnosed as eczema. Gluten is a protein found in wheat, barley, and rye. In people who have celiac disease, gluten causes an autoimmune response which results in the immune system attacking the lining of the small intestine—specifically the villi, the absorptive hair-like structures of the lining. With dermatitis herpetiformis, outbreaks are also triggered by gluten. Interestingly, unlike celiac disease which appears more in women than men, dermatitis herpetiformis is more commonly found in men by a ratio of about two-to-one. It is rarely seen in children under ten and first appears in the teenage years or even in one’s twenties or thirties. It may come and go, even if you’re eating a gluten-containing diet. Diagnosis is done with a skin biopsy. In most cases, a dermatitis herpetiformis diagnosis means celiac disease as well, even if you’re not obviously suffering from the characteristic intestinal symptoms of this disease. No matter what, the treatment is the same: a strict gluten-free diet. Dermatitis herpetiformis rashes are treated in two main ways--the gluten-free diet, of course, and antibiotics such as dapsone or sulfapyridine for those who aren’t able to tolerate dapsone. A truly gluten-free diet can eliminate dermatitis herpetiformis, but in my experience and according to the National Institutes of Health, a dermatitis herpetiformis rash responds dramatically to dapsone, within 48 to 72 hours. To treat the underlying cause of dermatitis herpetiformis, which is celiac disease, a strict gluten-free diet must be followed, but according to the National Institutes of Health, “Even with a gluten-free diet, dapsone or sulfapyridine therapy may need to be continued for 1–2 years to prevent further dermatitis herpetiformis outbreaks.” As a celiac with dermatitis herpetiformis, completely eliminating gluten from my diet has been the only lasting solution for dermatitis herpetiformis, but unfortunately I can accidentally ingest gluten from time to time, especially when I travel. In my most recent outbreak, I decided to get a prescription for dapsone. Although dapsone is a very strong drug with side effects and should be used sparingly, I was in need of something fast-acting. I followed the instructions exactly, and not only did it relieve the pain but within three days, I could see a remarkable change in the appearance of the dermatitis herpetiformis. After reexperiencing the painful and frustrating symptoms of dermatitis herpetiformis and the relief that came with proper treatment, I knew I had to address this topic to help others. I encourage everyone to get the word out about dermatitis herpetiformis so more and more people dealing with this misdiagnosed condition can get help just as I did. Resources: About.com: Dermatitis Herpetiformis, The ‘Gluten Rash’. Celiac Disease Awareness Campaign: Dermatitis Herpetiformis. eMedecine.Medscape.com: Dermatitis herpetiformis.
- 35 comments
-
- dermatitis
- dermatitis herpetiformis
- (and 5 more)
-
Celiac.com 08/05/2017 - I was told that I had irritable bowel disease about thirty years before being diagnosed with celiac disease. I avoided hard to digest foods such as corn, broccoli, beef and other foods difficult to digest, and instead I would, for instance, eat the bun of a hamburger, avoid steaks but eat the buttered buns and the gravy with a main meal and wondered why I was still having the gut and bowel reactions! Did you know that even in the absence of fully developed celiac disease, gluten can induce symptoms similar to FBD (Functional Bowel Disorder)? Doctors such as Elena F. Verdu, David Armstrong and Joseph Murray describe celiac disease and irritable bowel syndrome (IBS) as the "no man's land of gluten sensitivity.” Celiac disease is a condition traditionally characterized by chronic inflammation of the proximal small intestine resulting in villus atrophy and malabsorption. Irritable bowel disease is a clinical syndrome defined in the most recent Rome III consensus by the presence of abdominal pain or discomfort, at least three days per month in the last three months, and two or more other symptom features: 1) Improvement in defecation, 2) Association with a change in stool frequency, and 3) Association with a change in stool form or appearance. Other GI symptoms, such as bloating and distension are also considered to be consistent with a diagnosis of FBD (Functional Bowel Disorder) such as IBS. Did you know IBS has a prevalence of about 10% and is the most common GI disorder in our society, imposing a very high economic burden in North America? Did you know that there is an overlap between IBS and celiac disease? It has been reported that testing for celiac disease in patients with diarrhea-predominant IBS is cost effective if the prevalence of celiac disease is above 1%. Not only do the symptoms of IBS and celiac disease overlap, but epidemiological studies also suggest a greater than by chance association (4 - 5 fold increased risk). By convention, a patient with confirmed celiac disease is no longer considered to have IBS. It has never been determined whether celiac disease and IBS cannot co-exist, and there is no reason to think that a diagnosis of celiac disease necessarily precludes a diagnosis of IBS. Dr. Fasano has concluded that about 3% of patients with a "clinical" presentation of IBS were subsequently diagnosed with celiac disease. I would wager that many of you with confirmed celiac disease may also have the symptoms of irritable bowel disease. I cannot be alone in this! I can check off the symptoms of IBS on many occasions and yet I have diagnosed celiac disease and dermatitis herpetiformis. In Dr. Fasano's report: "they have concluded that gluten induced Patho-physiology may constitute an underlying factor in symptom generation in a proportion of patients with IBS like symptoms." A lot of this wording may seem like Greek or a "little over ones head" so to speak, but I believe what they are saying is though we define gluten sensitivity as a condition of some morphological, immunological, or functional disorder that responds to gluten exclusion and NOT a true disease. Gluten sensitivity changes that occur with IBS because of exposure to gluten are eventually going to show up positive for celiac disease. Why would a person who has been diagnosed and KNOWS that they have irritable bowel disease continue to ingest gluten when Fasano et. al., have concluded that about 3% of patients with a "clinical" presentation of IBS were subsequently diagnosed with celiac disease? Did you know that in July of 2016 teams of researchers at Columbia University published a study confirming that wheat exposure response is, in fact triggering a systemic immune reaction and accompanying intestinal cell damage. "It is estimated that the impacted population is equal to or even exceeds the number of individuals with celiac disease, the vast majority of whom remain undiagnosed" Dr. Armin Alaedin confirmed. Finally they are reporting that a person with irritable bowel disease may have gotten that way from ingesting gluten. Celiac Disease and Dermatitis Herpetiformis – Did You Know? 15 - 25% of individuals with celiac disease experience dermatitis herpetiformis? Dermatitis herpetiformis is a skin manifestation of celiac disease and is part of the abnormal immune response to gluten; Affects more men than women? Dermatitis herpetiformis generally starts in adulthood. It is not common to see dermatitis herpetiformis in children, but it can occur; Only about 20 percent of people with dermatitis herpetiformis have intestinal symptoms of celiac disease, however, biopsies show that 80 percent have some degree of damage to the small intestine, especially if a high gluten diet is maintained; If you suspect dermatitis herpetiformis you may have celiac disease; Iodine is something that a person with dermatitis herpetiformis should definitely avoid; One of the oldest checks for dermatitis herpetiformis was putting some iodine on ones thigh; Dermatitis herpetiformis sores tend to run in a line, or stay in a cluster; Dermatitis herpetiformis treatment consists of a gluten-free diet for life, just like in celiac disease? The skin's response to the gluten-free diet is much slower compared to the healing of the intestines in those with celiac disease. It may take about six months to achieve improvement, though with my own dermatitis herpetiformis spots daily dapsone was miraculous. It did take up to a year for the sores in my scalp to heal. Dr. John Zone, M.D. Professor and Dermatology Chair at the University of Utah and CDF Medical Advisory Board member states "There is little question that ingestion of large amounts of iodine dramatically worsens dermatitis herpetiformis," he continues, "iodine does not cause dermatitis herpetiformis. It worsens dermatitis herpetiformis. Gluten causes dermatitis herpetiformis." Dr. Zone explains that through seeing hundreds of celiac disease patients over the years, he has found that some react to highly concentrated solutions of iodine in cough medicines, shellfish, and kelp, which is often found in Sushi. He also cautions that dietary supplements may contain large amounts of kelp or iodine (usually in the form of potassium iodide or sodium iodide) which can worsen dermatitis herpetiformis. I can share with you that I was incorrectly told over 25 years ago by an internist that I could take up to five dapsone, going 5- 4 - 3- 2 -1, and if the spots had not totally disappeared I could repeat the process. Taking too much cased a blood disorder called Methemaglobinemia, a rare but dangerous response to taking too much dapsone. It is a blood disorder in which an abnormal amount of methemoglobin is produced. Hemoglobin is the protein in red blood cells (RBCH's) that carries and distributes oxygen to the body. Methemoglobin is a form of hemoglobin, with it the hemoglobin can carry oxygen, but is not able to release it effectively to body tissues. It can either be passed down through families (inherited or congenital) or be caused by exposure to certain drugs, chemicals, or foods (acquired). My nephew was on dapsone, which is, according to the Head of Dermatology at the University of British Columbia, the true test of dermatitis herpetiformis. By taking Dapsone for three or four days the lesions (itchy/sore blisters that beg to be itched, and when you do you break open a lesion that appears to contain liquid...they burn, then they crust, and if you continue to pick off that crust they scar your skin.) almost disappear like magic. My nephew thought it was permissible to cheat once in a while and thought that he could get away with it. He used to eat hamburgers every time the craving for a "Big Mac" overcame him! He ate one, or maybe two, until he found out he had dermatitis herpetiformis sores on the soles of his feet and was limping from the pain. Who knows what damage he was doing to the villi in his bowel! It is a vast no man's land out there, but if you are a celiac and have dermatitis herpetiformis or are gluten sensitive you need to step into that “land” and learn more about the diseases and what is going on in your body!
- 2 comments
-
Celiac.com 01/04/2021 - Researchers have long known that the common chronic skin disorder atopic dermatitis is associated with other atopic conditions. A growing body of evidence supports a connection with non-atopic conditions, including autoimmune diseases, such as celiac disease, but data are limited with respect to autoimmune conditions. To remedy the situation, a research team recently examined the connection between atopic dermatitis and autoimmune diseases. The research team included L.U. Ivert, C.F. Wahlgren, B. Lindelöf, H. Dal, M. Bradley, and E.K. Johansson. They are variously affiliated with the Dermatology and Venereology Unit, Department of Medicine Solna, Karolinska Institutet, Stockholm, Sweden; the unit of Dermatology, Theme Inflammation and Infection, Karolinska University Hospital, Stockholm, Sweden; the Theme Cancer unit, Karolinska University Hospital, Stockholm, Sweden; and the Dermatological and Venereal Clinic, Södersjukhuset, Stockholm, Sweden. For their case–controlled study, the team looked at the Swedish national healthcare registers, and looked at data from the entire Swedish population, aged 15 years or younger, from 1968 to 2016. The researchers matched all atopic dermatitis cases by sex and age to healthy controls; including cases with an inpatient diagnosis of atopic dermatitis from 1968, and/or a specialist outpatient diagnosis of atopic dermatitis from 2001. In all, the team found 104,832 cases of atopic dermatitis, and matched them to 1,022,435 control subjects. Adults with multiple autoimmune diseases were more likely to develop atopic dermatitis than those with just one autoimmune disease. The associations were especially strong between atopic dermatitis and autoimmune dermatological, gastrointestinal and rheumatological diseases. The study was funded by the Swedish Asthma and Allergy Association Research Foundation, Hudfonden (The Welander‐Finsen Foundation), and The Swedish Society for Dermatology and Venereology. The authors declare no conflicts of interest. These results invite further study of the relationship between atopic dermatitis and autoimmune conditions, such as celiac disease. Read more in the British Journal of Dermatology
-
- adults
- atopic dermatitis
-
(and 4 more)
Tagged with:
-
Celiac.com 10/06/2020 - One question we get often is about celiac disease and rashes. Specifically, is it common for people with celiac disease to have a rash? Skin rash alone is not a specific symptom of celiac disease. However, people with celiac disease can have higher rates of certain skin conditions that can cause rashes. Rashes are also not commonly in the top ten complaints of people with celiac disease. However, these seven common skin conditions are associated with celiac disease: Acne; Canker Sores (Aphthous Stomatitis); Dermatitis Herpetiformis; Dry Skin; Eczema; Psoriasis; and Rosacea. Dermatitis Herpetiformis (DH) is Common Cause of Skin Rash in Celiac Patients Dermatitis herpetiformis (DH) is a common extraintestinal manifestation of celiac disease, marked by itchy papules and vesicles on the elbows, knees, and buttocks. Dermatitis herpetiformis is a common in people with celiac disease, and is one immediate suspect for anyone with celiac disease who develops a rash. About 1 out of 8, or about 12 percent of people with celiac disease will also have Dermatitis Herpetiformis (DH). In fact, DH is now regarded as external manifestation of celiac disease in the skin. It is also possible for people to have DH and not have celiac disease, but everyone with DH should be screened for celiac disease. The good news is that most people with DH see significant improvement on a gluten-free diet. Moreover, patients with refractory DH see major gut improvement on a gluten-free diet. Some patients with celiac disease have complained of hives, but hives are not common in celiac patients. There have also been studies to show that six out of sixty patients (10%) with Non-Celiac Wheat Sensitivity (NCWS) suffered from contact dermatitis and nickel allergy, double the 5% rate seen in the control group. DH, Eczema & Psoriasis Often Improve with Gluten-Free Diet Other conditions that can cause skin rashes in celiacs (and non-celiacs) include eczema and psoriasis. As with DH, a gluten-free diet is becoming a more common treatment for eczema. People who are gluten intolerant also tend to have more advanced psoriasis. Like eczema, many people with psoriasis improve when patients follow a gluten-free diet. Herpes Zoster or Shingles and Celiac Disease People with celiac disease have a slightly higher risk of developing shingles (herpes zoster), which could also be triggered by a COVID-19 infection. Again, a rash all by itself is not a sign of celiac disease. However, if you have a rash associated with one of the above conditions AND you have celiac symptoms, such as nausea, vomiting, stomach upset, then you might want to consult a doctor about celiac disease.
- 8 comments
-
- celiac
- celiac disease
-
(and 6 more)
Tagged with:
-
Hello, I wanted to share my personal experience of what cured my Perioral dermatitis. I hope this will help others find a solution to their Perioral dermatitis problems as well. I know how awful it is and how painful those blistering hives are, so my heart goes out to anyone dealing with it. The steps below are what cleared the devil rash off my face, in addition to cutting gluten completely out of my diet. My PD flared up and got so much worse each time I ate anything with gluten. *Disclaimer*: I am not a medical professional. I'm just a fellow victim of Perioral dermatitis trying to help! I do mention products/brands, but this is not a sponsored post in any way. This is just what has worked for me personally. I tried to make this as detailed as possible, but if anyone has any questions, please feel free to reply to this post or message me. 1). DO NOT PUT ACNE CLEARING PRODUCTS ANYWHERE NEAR IT!!! I had absolutely no clue what Perioral dermatitis even was when it first showed up. I just thought it was acne since it was on my face. I made the massive mistake of putting acne washes that contained alcohols, acne creams, toners, and then finally hydrocortisone all over the bumps. Which caused the rash to viciously spread like wildfire. This is why it is so important to see a dermatologist about your skin problems. 2). Doxycycline. My dermatologist prescribed me doxycycline 100 mg, 1 per day for 6 weeks (Currently still taking it because the 6 weeks aren't up yet.) But after 3 doses, I am not even kidding you, the PD rash/bumps began to disappear. And the inflamed, burning, blistering itch was no more!!! Talk to your dermatologist about the best option for you, but I give doxycycline the most credit for clearing my Perioral dermatitis so fast. The first dose did make me feel nauseous, so I just take it before bed. It also causes increased sun sensitivity, so be mindful of that. 3). Pimecrolimus Cream 1% (Again, must be prescribed. This is not an over the counter medication.) This cream treats dermatitis and eczema. This is NOT a steroid cream. I warn you all... stay FAR, FAR, FAR away from any steroid topical creams!!! Steroids will make the PD incredibly worse. 4). Spectro Jel Cleanser Frangrance Free. I read about this cleanser on a blog for curing Perioral dermatitis. You can buy this cleanser on Amazon. Read the reviews! You will see that almost every person mentions how great it has been for their PD. From my personal experience, this is the only face wash that hasn't felt like I'm rubbing acid onto my skin. It has seriously worked wonders for me! I wash with it twice a day. I don't use any sort of face washing tool, and no toners, scrubs, serums, etc. If you're suffering from PD or have sensitive skin, I highly suggest you do the same. My skin drastically cleared up once I stopped using unnecessary products. I know that doesn't seem glamorous and fun, but neither is the dermatitis... am i right?! --- Here's a link to the cleanser: https://www.amazon.com/Spectro-Cleanser-Fragrance-Free-200ml/dp/B00CUIKYJW/ref=sr_1_1?dchild=1&keywords=spectro&qid=1598559522&sr=8-1 5). Fluoride free toothpaste. My dermatologist told me to throw out my toothpaste if it contained fluoride. She said toothpaste containing fluoride can actually cause or irritate PD. The brand I like and recommend is 'Toms'. It's fluoride free and is made with natural ingredients. 6). Get a gluten free chapstick. I was so surprised to find out how many chapsticks or lip balms actually contain gluten. My lips have always been dry or irritated, regardless of how much water I drink or how much chapstick I use. After discovering my gluten allergy, I realize it's because my lips couldn't handle the ingredients. An amazing, super hydrating option is 'EOS: The Hero Extra Dry Lip Treatment' It is gluten free and hypoallergenic. (but always check labels for ingredients you may be sensitive to) 7). Gluten Free Shampoo and Conditioner. Now obviously, I know (or hope) that no one is ingesting their hair products. However, think about how close they get to your face! Duh it goes all over your scalp, but it also can come in direct contact with your face during a shower. I have been using 'Garnier Fructis Pure Clean' which is free of gluten. I believe it's also free of some other common allergens. Google it and check it out for yourself! 8). All Free Clear Detergent. Oh my gosh... ANYONE with sensitive skin, allergies, eczema, Perioral dermatitis, whatever!!! Please be careful of the detergent you are using to wash your clothes. Detergents have been one of the biggest irritants for my sensitive skin, especially my neck and face. 'All Free Clear' is great and is my go-to. It's the only one that doesn't turn my skin red and make me itch like crazy. 9). Makeup. When my Perioral Dermatitis first happened and was at it's absolute worst, I didn't put any makeup on my face for 2 weeks. Trust me, I know you want to cover it up any way you can. I did too, because I thought I looked like a horrifying monster. But the rash will heal so much faster if you aren't putting foundation or powder on your face. Putting makeup on also means taking it off, and using makeup wipes while I had the rash drove my skin absolutely nuts.
- 1 reply
-
- atopic dermatitis
- dermatitis
- (and 8 more)
-
Celiac.com 07/09/2020 - Celiac disease is an autoimmune disease that occurs in genetically predisposed individuals. It is estimated to affect 1 in 100 people worldwide, and is treated by a gluten-free diet. However, there’s also dermatitis herpetiformis (DH) to consider, which is basically celiac disease of the skin instead of the intestines. It’s a skin condition characterized by groups of itchy blisters that commonly occur on pressure points such as the elbows, the front of the knees, the buttocks, back, shoulders, face, and scalp. However, they can occur anywhere on the body. Dermatitis herpetiformis is eruptions can be very painful, and the itchy rashes may progress to red, raised patches of skin that can develop into small, watery blisters. To get a DH diagnosis you need to make an appointment with a gastrointestinal (GI) doctor and a dermatologist. Note that you need to continue to consume gluten until all tests for celiac disease and DH are concluded, and for DH a doctor will take a skin biopsy. (It should heal relatively quickly, with very little scarring.) Then, a lab will use dye to see if you have IgA in a particular type of pattern. This tells your doctor whether you have dermatitis herpetiformis or not. They can help you to get the inflamed reaction under control with cortisone (a steroid), while you simultaneously begin your lifestyle adjustment of not eating wheat, rye, barley, oats, and even dairy (specifically casein because the protein is very similar to that in gluten.) After diagnosis you will need to maintain a 100% gluten-free diet, and you’ll need to use topical products that are gluten-free as well. Be sure to double check your makeup (lipstick, mascara, eyeshadow, eyeliner, blush, etc.), hand lotions, facial wipes, detergents, soaps, sanitizers, perfumes, bug spray, sunblock, and much more. Basically, what it comes down to is reading all ingredients, checking FAQ sections on websites, and calling the manufacturer directly to question cross contamination procedures. Taking these extra precautions will help to keep your skin clear, smooth, and free from continuing outbreaks. However, even with doing all of the above the healing time can be different for everyone. Some individuals heal in a few months, while some take a couple of years. Even if you’re clear for years but accidentally get gluten from cross contamination, you could suffer another outbreak. This is why it’s very important to be extra focused on your nutrition and beauty products after a positive DH diagnosis. A picture of DH from one of our forum members "amine33". References: gluten.org celiac.org Forum discussions about dermatitis herpetiformis.
- 3 comments
-
- blisters
- celiac diease
-
(and 5 more)
Tagged with:
-
Hi all! I'd love your thoughts on this. I'm a 25 year old female and I've had a few different symptoms so I'm considering getting tested, but I have no family members with celiac or anything like that. I'm not sure if this actually looks like these could mean it or not! I've had these little bumps on my elbows, knuckles, and knees on and off for 5 years. They're like small blisters filled with clear liquid and are super itchy. Anti-itch cream and lotions don't do anything for them, they just sometimes disappear after a while. Wondering if it's dermatitis herpetiformis? I've been diagnosed with anxiety/panic attacks and depression and have been on and off medication for 4 years I had Mono and a Vitamin D deficiency 8 years ago and I haven't been checked for it since then...no idea if I'm still deficient or not, but I am definitely still always tired. I frequently feel sluggish physically, which is different from the mental sluggishness of my depression. I've had stomach/digestion issues for yearssss now and I've been unable to find any actual food allergies. My entire abdomen will feel incredibly bloated for 2 or 3 days at a time, but I'll also just get my stomach bloated frequently after I eat. My stomach also hurts a lot and I'm always paranoid I have appendicitis, but it never turns out to be that and goes away after a bit. I've tried being gluten free/diary free before but I wasn't incredibly strict about it and it seemed to help some? But not always. I'll often feel gross and nauseous in the morning if I eat right before going to bed. I also saw somewhere that sometimes vitiligo can be a symptom (although it's not listed on most sources) and I do have some on my face I feel like there are more things too, but they've slipped my mind at the moment. Thanks for taking the time to read this!
- 6 replies
-
- anxiety diagnosed
- depression
-
(and 2 more)
Tagged with:
-
Hello, this is my first post and to be honest I’m shocked I’m here. I have no stomach problems and felt generally healthy up until a few weeks ago. I am now broken. Ive had an itchy scalp for ages but recently it got infected. The doc treated the infection but since I have broken out in the most horrendous rash which I think is D.H which just stared on my scalp It started as small red spots, watery blisters that pop under the lightest touch. Now huge raised crusty lumps. All itching to my bones and sometimes burning. I have been docs 5 times in two weeks and today a&e as I feel completely desperate. I’m scared, anxious and a shell of the person I was last month. I keep mentioning the gluten rash to people and they’re brushing it off, saying it’s viral, a reaction etc. I feel crazy as I 100% tick every box for this. I’m also light headed and my eyes hurt. So my question would be,how do I get help. What do I say? Ive had a gluten blood test so waiting on the result. I’ve been referred to dermatologist but that could take 12 weeks. This is consuming me and I’m so scared it could take forever to get sorted. thanks in advance xx
- 3 replies
-
- dermatitis
- diagnose
-
(and 1 more)
Tagged with:
-
Celiac.com 11/20/2019 - Both atopic dermatitis and celiac disease are often accompanied by other immune-mediated disorders. A team of researchers recently set out to see if they could find a connection between atopic dermatitis and celiac disease in a broad community-based population. The research team included Guy Shalom, Khalaf Kridin, Keren-Or Raviv, Tamar Freud, Doron Comaneshter, Rivka Friedland, Arnon D. Cohen, and Dan Ben-Amitai. The team conducted a cross-sectional observational design, in which they collected demographic and clinical data for patients enrolled in a large health management organization who were diagnosed with atopic dermatitis by a dermatologist in 2002–17. They recorded presence of celiac disease and celiac-related morbidities for the entire group, for adults over 18 years old, and for adults with moderate-to-severe atopic dermatitis. They then compared the findings with a matched control group without atopic dermatitis. The study group included 116,816 patients, with a total of 45,157 adults, along with 1,909 adult adults with moderate-to-severe atopic dermatitis. Multivariate analysis showed that atopic dermatitis was associated with a significantly higher rates of celiac disease across the entire study population, and for each study group. The results showed a meaningful connection between atopic dermatitis and celiac disease, and demonstrate the need for timely screening of people with atopic dermatitis for gastrointestinal morbidities. Read more in the American Journal of Clinical Dermatology The researchers in this study are variously affiliated with the team of researchers recently set out to Clalit Health ServicesTel Aviv, Israel; the Division of Community Health, Faculty of Health Sciences, Siaal Research Center for Family Medicine and Primary Care Ben Gurion University of the Negev Beer-Sheva, Israel; the Department of Dermatology Rambam Health Care Campus, Haifa, Israel; the Pediatric Dermatology Unit Schneider Children’s Medical Center of Israel, Petach Tikva, Israel; the Chief Physician’s Office, Clalit Health Services Tel Aviv, Israel; and the Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel.
- 11 comments
-
- atopic dermatitis
- celiac
-
(and 3 more)
Tagged with:
-
Celiac.com 08/26/2013 - Celiac disease and its cutaneous manifestation, dermatitis herpetiformis are both disease marked by sensitivity to gluten. Metabolic bone disease is common among in people with celiac disease, but there isn't much data on rates of bone density in patients with dermatitis herpetiformis. A team of researchers recently set out to determine if dermatitis herpetiformis triggers bone loss, as does celiac disease. The research team included K. Lorinczy, M. Juhász, A. Csontos, B. Fekete, O. Terjék, P.L. Lakatos, P. Miheller, D. Kocsis, S. Kárpáti, Tulassay Z, Zágoni T. For their study, the team wanted to compare bone mineral density (BMD) of celiac and dermatitis herpetiformis patients. The study group included 34 celiac patients, 53 with dermatitis herpetiformis and 42 healthy controls. Average age for celiac patients was 38.0 +/- 12.1 years, for dermatitis herpetiformis it was 32.18 +/- 14.95 years, while it was 35.33 +/- 10.41 years for healthy control subjects. The team used dual-energy X-ray absorptiometry to measure bone mineral density of the lumbar spine, the left femoral neck and radius. They defined low bone density, osteopenia and osteoporosis as a body mass density (BMD) T-score between 0 and -1, between -1 and -2.5, and under -2.5, respectively. They found decreased BMD in the lumbar region, consisting of dominantly trabecular compartment, in 26 patients (49%) with dermatitis herpetiformis, 21 patients with celiac disease (62%), and in 12 of the healthy control subjects (29%). They also measured lower BMD at the lumbar region in dermatitis herpetiformis and celiac patients, compared to healthy subjects (0.993 +/- 0.136 g/cm2 and 0.880 +/- 0.155 g/cm2 vs. 1.056 +/- 0.126 g/cm2; p < 0.01). They found no difference in density of bones consisting of dominantly cortical compartment (femoral neck) between dermatitis herpetiformis patients and healthy control subjects. The results show that a low bone mass is also common in patients with dermatitis herpetiformis. Bone mineral content in these patients is significantly lower in those parts of the skeleton which contain more trabecular bone, and less reduced in areas with more cortical bone. Source: Rev Esp Enferm Dig. 2013 Apr;105(4):187-193.
- 3 comments
-
- celiac
- dermatitis
-
(and 4 more)
Tagged with:
-
Celiac.com 02/20/2017 - Nickel is the most common cause of contact allergy, and nickel exposure can result in systemic nickel allergy syndrome, which mimics irritable bowel syndrome (IBS). Nickel is also found in wheat, which invites questions about possible nickel exposure from wheat in some cases of contact dermatitis. However, nickel hasn't really been studied in relation to glutenâ€related diseases. A research team recently set out to evaluate the frequency of contact dermatitis due to nickel allergy in NCWS patients diagnosed by a doubleâ€blind placeboâ€controlled(DBPC) challenge, and to identify the characteristics of NCWS patients with nickel allergy. The research team included Alberto D'Alcamo, Pasquale Mansueto, Maurizio Soresi, Rosario Iacobucci, Francesco La Blasca, Girolamo Geraci, Francesca Cavataio, Francesca Fayer, Andrea Arini, Laura Di Stefano, Giuseppe Iacono, Liana Bosco, and Antonio Carroccio. The are variously affiliated with the Dipartimento di Biologia e Medicina Interna e Specialistica (DiBiMIS), Internal Medicine Unit, University Hospital, Palermo, Italy; the Surgery Department, University Hospital, Palermo, Italy; Pediatric Unit, "Giovanni Paolo II" Hospital, Sciacca (ASP Agrigento), Italy; DiBiMIS, Gastroenterology Unit, University Hospital, Palermo, Italy; Pediatric Gastroenterology Unit, "ARNAS Di Cristina" Hospital, Palermo, Italy; Dipartimento di Scienze e Tecnologie Biologiche Chimiche e Farmaceutiche (Ste.Bi.CeF), University of Palermo, Palermo, Italy. Their team conducted a prospective study of 54 women and 6 men, with an average age of 34.1 year, and diagnosed with NCWS from December 2014 to November 2016. They also included a control group of 80 age†and sexâ€matched subjects with functional gastrointestinal symptoms. Patients reporting contact dermatitis related to nickelâ€containing objects were given a nickel patch sensitivity test. The tests showed that six out of sixty patients (10%) with NCWS suffered from contact dermatitis and nickel allergy, and this frequency was statistically higher than observed in the 5 percent seen in the control group. Compared to NCWS patients who did not suffer from nickel allergy, NCWS patients with nickel allergy commonly showed a higher rates of skin symptoms after wheat consumption. Contact dermatitis and nickel allergy are more frequent in NCWS patients than in subjects with functional gastrointestinal disorders. Moreover, large numbers of these patients showed cutaneous manifestations after wheat ingestion. Nickel allergy should be evaluated in NCWS patients who have cutaneous manifestations after wheat ingestion. More study is needed to determine the relationship between nickel sensitivity and NCWS. Source: Nutrients 2017, 9(2), 103; doi:10.3390/nu9020103
- 3 comments
-
- contact
- dermatitis
-
(and 5 more)
Tagged with:
-
The following was written by Dr. Joseph Murray, one of the leading USA physicians in the diagnosis of celiac disease (celiac disease) and dermatitis herpetiformis (DH). Dr. Murray (murray.joseph@mayo.edu) of the Mayo Clinic Rochester, MN, is a gastroenterologist who specializes in treating Celiac disease: In response to your questions about DH, The following represents my views about this curious and very itchy condition. In general DH is a severely itchy skin condition that often starts abruptly, affecting the elbows knees buttocks and scalp and the back. It usually starts as little bumps that can become tiny blisters and then are usually scratched off. It can occur in one spot only but usually occurs in many different areas. The condition is related to the deposit under the skin of IgA deposits. These occur in response to the ingestion of gluten in the diet. However, once deposited there, they are only slowly cleared by the body even when the individual is gluten free. While most individuals with DH do not have obvious GI symptoms almost all have some damage in their intestine. They the potential for all of the nutritional complications of celiac disease. The diagnosis is made by taking a skin biopsy and performing immunoflorescence studies on it (a specialized type of stain in major laboratories) The test is usually reliable but it takes a significant dedication to detect early cases where there is a short history of rash rather than years or months of rash. It is unusual to develop DH after the start of a GFD for celiac disease. About 5 % of celiac disease patients will develop DH usually in the first 6-12 months. This probably reflects the long lasting nature of the deposits under the skin. Treatment for DH is twofold. (1) Remove the cause: gluten. (2) Suppress the skin response with drugs such as Dapsone or some other sulphones. The latter is the most common treatment used as it is rapidly relieves the itch. However there are some side effects associated with these medications and they need to be taken under medical monitoring with blood tests to detect side effects. It is my practice that DH should be treated with a gluten-free diet for life and use of drugs to get immediate relief in the short term. It is usually possible to get patient off the Dapsone after several months of a strict gluten-free diet. The most common complication of DH is scarring which usually fades with time. Occasionally there can be secondary infection from scratching. There is probably a slightly increased chance of malignancy in those with DH who are not on a gluten-free diet. Several physical triggers are known to set off an attack of DH, especially exposure to iodides and bromides which are contained in household cleaners. A very good reference for DH is available from the GIG in Washington.
- 2 comments
-
- celiac
- dermatitis
-
(and 5 more)
Tagged with:
-
J Allergy Clin Immunol 2004;113:1199-1203. Celiac.com 07/30/2004 - According to a study by Italian researchers published in the June edition of the Journal of Allergy and Clinical Immunology, the prevalence of atopic dermatitis is much more common in those with celiac disease. The researchers looked at 1,044 adults with untreated celiac disease at the point of their diagnoses, as well as 2,752 of their relatives, and 318 of their spouses. They also looked at the prevalence of allergies in celiacs after one year on a gluten-free diet. The subjects filled out a standardized questionnaire upon their diagnosis, and those who reported having an allergy were tested for it using a standard makeup of 20 antigens for serum specific IgE. The researchers found that one celiac in 173 (16.6%) had at least one additional allergy, compared with 523 of their relatives (19%), and 43 of their spouses (13.5%). Patients with celiac disease were also more likely (3.8%) to have atopic dermatitis than their relatives (2.3%) or their spouses (1.3%). The amount of time that the celiac patients went undiagnosed and therefore untreated did not seem to influence the presence of allergy or atopic dermatitis. It is possible that a longer period of time on a gluten-free diet could influence the prevalence of allergy in those with celiac disease, and more research needs to be done to determine if being gluten-free longer can decrease allergies in those with celiac disease.
- 3 comments
-
Hi fellow celiacs! I have been diagnosed with celiac disease when I was 19 years old, 13 years ago! I have always face my diagnosis with optimism and a positive mind but as I grew older I started to feel a little hopeless sometimes about all my health issues that may or may not be related to celiac disease. I have always consider that I had a good health overall but now, at 32 I have a diagnosed celiac disease, I take mild medication for anxiety/depression, two years ago I started to have a hormonal imbalance and digestive disorders like ibs (maybe ¿?) and I often suffer from brain fog. I have always have high myopia, runner's knee, seasonal allergies... I am very careful with my gluten free diet but with the years If I accidentally get some gluten I get itchy blisters and one month ago I got something similar to eczema. It is my first time in a forum since I have started wondering if there is something else that I should be taking care of. I don't want to get to obsessed with my health but the truth is that I feel that I am young to have all this little health concerns. I am exploring alternative medicine solutions, specially related to nutrition to ease my different issues and heal my gut. I don't know any professional in my country that can take a holistic look at my health so I have done most of the research by myself in the internet which can be a little confusing and overwhelming at times... Any word of encouragement or advise will be much appreciated : ) All the best to you,
- 8 replies
-
- dermatitis
- hormones
-
(and 2 more)
Tagged with:
-
Hi there! I hope anyone can help me... From a young age I have been diagnosed with atopic dermatitis. My mostly effected body parts are my hands, inner elbow(?) and the back of my knees. I've been using cortisone creams (weak and very strong ones) for as long as I can remember. I've never seen severe or any effect of using any of these.. My dermatitis do go away sometimes (usually goes away when I go on holidays to tropical countries). I would say I've had dermatitis for maybe 70-80% of my life. Two or three times I've had "flareups" on almost identical areas of my body. These flareups consist of dermatitis around my mouth (looks horrible and affects my self esteem a lot) and on my neck. I think the first time I had it was when I was 15 (it lasted for 1,5 years) then when I was 18 (lasted for 4-6 months) and I just got it again at age 21. I got extremely upset because I knew it would last for some time due to the past incidents. I searched for hours online, and tried thinking of correlations between the earlier flareups. I found an article about dermatitis herpetiformis which caught my eye. Because I was desperate to see improvement of the dermatitis I went gluten free the same day. At this time I'd had the rash for 3 weeks without ANY improvement, and it was especially bad in the mornings (maybe due to lack of lubrication during nighttime). The next morning I woke up and the dermatitis around my mouth was almost COMPLETELY gone. I was in shock!! I couldn't believe it was some sort of coincidence, so I continued eating gluten free and haven't seen the dermatitis around the mouth since then. Haven't been eating gluten for 2 weeks besides one time by mistake (I got signs of the mouthrash only an hour after eating). I also wanna add that I do get the typical liqiud-filled blisters that are characterized with dermatitis herpetiformis; in my moutharea and hands. Sadly I still have it on my hands, some on my neck and inner elbows, but I do feel it's less itching and irritated. I hope people can help me with my questions. 1) Could it be that I have both atopic dermatitis and dermatitis herpetiformis? Has anyone ever heard of that? Or is it possible that the areas that are still affected will get better by time? 2) I've read the only way to diagnose this disease is by skin biopsy; does this mean I have to be eating gluten in order to get a positive result? I really don't want to go around with the rash in my face when I know I can avoid it by eating gluten free.. 3) I couldn't find much about this online, but is it common to have other symptoms such as feeling tired and exhausted, migraine, anxiousness and depression etc... when having dermatitis herpetiformis?
- 7 replies
-
- atopic eczema
- dermatitis
- (and 8 more)
-
Celiac.com 03/06/2017 - Dermatitis herpetiformis is an autoimmune skin-blistering disease which is commonly associated with celiac disease. The most common treatments are a gluten-free diet along with the addition of dapsone. DH that does not respond to either a gluten-free diet, or to dapsone, is treated with other immune-suppressing medications, but results have been mixed. Now, for the first time, a patient treated with rituximab therapy had resolution of both his pruritus and skin rash. "In addition, the levels of both anti-tissue and anti-epidermal transglutaminase antibodies normalized," said Dr. Ron Feldman of Emory University School of Medicine. Writing in JAMA Dermatology, Dr. Feldman and colleagues describe a man in his 80's with a five-year history of worsening DH. He was put on a gluten-free diet along with dapsone 50 mg daily, but his pruritic rash persisted. Dapsone was discontinued because of worsening anemia. He began treatment with 3 g sulfasalazine daily, but this was discontinued due to gastrointestinal symptoms. His disease worsened, and he was put on a tapering course of prednisone from 40 mg to 10 mg daily along with azathioprine titrated up to 2.5 mg/kg daily. However, his disease continued to worsen over subsequent months. He was then treated with rituximab according to the protocol used to treat lymphoma: four weekly infusions of 375 mg/m2. "Rituximab," says Dr. Feldman, "has already shown efficacy in the treatment of other autoimmune blistering diseases such as pemphigus and pemphigoid and may have relevance with other B cell mediated diseases in dermatology." Thirteen months after treatment, the patient experienced complete resolution of pruritus and other symptoms of DH, as well as normalization of antibodies against both epidermal and tissue transglutaminases. Not only was there a normalization of antibodies against both epidermal and tissue transglutaminases, the patient went into remission and has remained symptom-free for up to a year and a half thus far, said Dr. Feldman. There is some cause for excitement here, since rituximab is well tolerated and can potentially provide long lasting remission with removal of pathogenic autoimmune B cells. Dr. Feldman concedes that their patient did not have serious gastrointestinal symptoms, but remains "hopeful that rituximab may provide similar benefits for patients with celiac disease, in which anti-tissue transglutaminase antibodies play a role, although further research will need to be done to confirm this." Source: JAMA Dermatology, online December 28, 2016
- 2 comments
-
- dermatitis
- dermatitis herpetiformis
- (and 4 more)
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8-M):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8-M):