-
Welcome to Celiac.com!
You have found your celiac tribe! Join us and ask questions in our forum, share your story, and connect with others.
-
Celiac.com Sponsor (A1):
Celiac.com Sponsor (A1-M):
-
Get Celiac.com Updates:Support Celiac.com!
Search the Community
Showing results for tags 'Celiac Disease'.
-
Celiac.com 08/30/2023 - We get a lot of questions from celiac community members wondering if certain products are gluten-free. One question we see a lot is about meat products. Specifically, is pepperoni gluten-free and safe for people with celiac disease? Traditionally prepared pepperoni consists of beef, pork, spices, and curing agents. These ingredients, on their own, are usually naturally gluten-free. So, Pepperoni is usually naturally gluten-free. However, some brands may use preservatives and grains, and some may have a risk of cross-contamination with wheat during the manufacturing process. Look for gluten-free labels and ingredients There are a number of top brands of pepperoni that are labeled gluten-free and are safe for people with celiac disease. When buying pepperoni, if you have celiac disease, it's good to look for products that have been labeled gluten-free, or certified gluten-free. In truth, though, if pepperoni is made in the USA without gluten ingredients, and does not have a wheat allergen warning, then it is likely safe. To be sure, it doesn't hurt to stick to brands that are labeled gluten-free, or are known by consumers to be safe. Brands of Pepperoni Labeled or Certified Gluten-Free, or Naturally Gluten-Free Without an Allergen Warning for Wheat: Armour Armour Pepperoni Boar's Head Boar's Head offers a wide variety of gluten-free deli meats, including pepperoni: Boar's Head Traditional Pepperoni - natural casing Boar's Head Pepperoni Dietz & Watson Dietz & Watson Legacy Sliced Pepperoni Dietz & Watson Pepperoni Twin Pack HEB HEB Sliced Pepperoni Hormel Hormel Pepperoni There are likely many other brands of pepperoni that are gluten-free and safe. If we missed a favorite of yours, then be sure to share it in the comments below. As always, read labels carefully and avoid any gluten ingredients.
- 1 comment
-
- brands
- celiac disease
-
(and 3 more)
Tagged with:
-
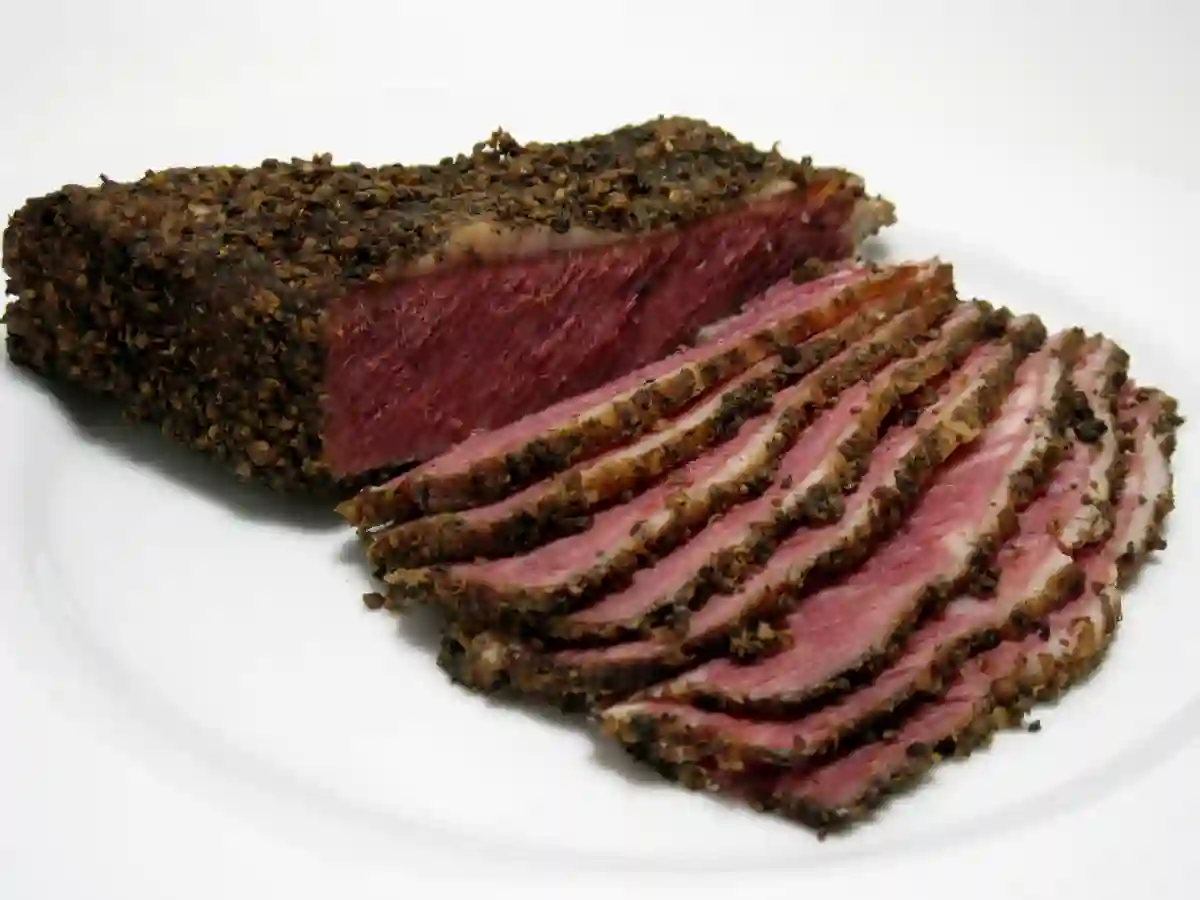
Celiac.com 08/25/2023 - We get a lot of questions from celiac community members wondering if certain products are gluten-free. One question we see a lot is about meat products. Specifically, is pastrami gluten-free and safe for people with celiac disease? Traditionally prepared pastrami consists of beef, spices, and curing agents. These ingredients, on their own, are usually gluten-free. However, cross-contamination can occur during the manufacturing process, which may introduce gluten into the final product. The main risk of gluten contamination comes from spices and seasonings. Some spice blends and seasonings may contain gluten. Also, some marinades and glazes used to make pastrami may contain gluten. Beware of any gluten ingredients in pastrami. Pastrami with Gluten-Free Labels There are a number of top brands of pastrami that are labeled gluten-free and are safe for people with celiac disease. When buying pastrami, if you have celiac disease, it's good to look for products that have been labeled gluten-free, or certified gluten-free. Brands of pastrami that are labeled gluten-free, or certified gluten-free include: A&H A&H Pastrami, Beef Aaron's Aaron's Best Smoked Beef Pastrami Aaron's Best Smoked Turkey Pastrami Bar-M Bar-M Pastrami, Beef, Sliced Boar's Head Boar's Head offers a wide variety of gluten-free deli meats, including pastrami: Boar's Head 1st Cut Pastrami Brisket Boar's Head Cap-Off Top Round Pastrami Boar's Head Pastrami Boar's Head Pastrami Seasoned Turkey Breast Buddig Buddig Original Pastrami Dietz & Watson Dietz & Watson Navel Pastrami Dietz & Watson Spiced Beef Pastrami Empire Empire Kosher Turkey Pastrami First Street First Street Navel Pastrami, Sliced New York Style First Street Premium Sliced Pastrami Jack's Gourmet Jack's Gourmet 1st Cut Pastrami (Kosher) Jennie-O Jennie-O 95% Fat Free Turkey Pastrami Meal Mart Meal Mart Beef 100% Premium Dry Rub Pastrami Wellshire Farms Wellshire Farms Cooked Pastrami
- 1 comment
-
- brands
- celiac disease
-
(and 3 more)
Tagged with:
-
Celiac.com 04/17/2024 - Maintaining optimal health involves ensuring that our bodies receive essential nutrients, including magnesium, a vital mineral crucial for various bodily functions. Magnesium deficiency can arise from various factors, including medical conditions like celiac disease, poor absorption, increased need, or excessive elimination. Understanding the signs, causes, and remedies for magnesium deficiency is essential for overall well-being. Identifying Magnesium Deficiency Symptoms Magnesium deficiency symptoms may initially manifest subtly, including muscle spasms, fatigue, decreased appetite, and nausea. However, if left unaddressed, more severe effects such as abnormal heart rhythm, seizures, anxiety, and personality changes may occur. As these symptoms overlap with those of other health conditions, a blood test from a medical provider is crucial to confirm magnesium deficiency accurately. Causes of Magnesium Deficiency Malabsorption due to gastrointestinal conditions like celiac disease or inflammatory bowel disease can hinder magnesium absorption. Additionally, certain medications and increased magnesium needs, such as during pregnancy or in athletes, can contribute to deficiency. Factors that affect magnesium elimination, like alcohol consumption or medical conditions such as kidney disease, also play a role. The Role of Magnesium in the Body Magnesium plays a vital role in numerous bodily processes, including muscle and nerve function, heart rhythm maintenance, blood sugar control, bone health, and blood pressure regulation. Furthermore, magnesium influences hormone balance related to sleep, circadian rhythm, and mood regulation, and can alleviate conditions like migraine headaches. Sources of Magnesium To address magnesium deficiency, both oral supplements and magnesium-rich foods can be beneficial. Supplements, such as magnesium glycinate or magnesium citrate, offer an easily accessible solution, although they may cause mild gastrointestinal side effects. Alternatively, incorporating magnesium-rich foods like pumpkin seeds, almonds, spinach, soy, and black beans into one's diet can help meet daily magnesium requirements. Frequently Asked Questions About Magnesium What is the best magnesium supplement? Magnesium glycinate and magnesium citrate are generally well-tolerated forms of magnesium supplements. Are there supplements best avoided when taking magnesium? Calcium supplements should be taken separately from magnesium to prevent competition for absorption. What medications interfere with magnesium: Certain medications, including proton pump inhibitors, antibiotics, diuretics, and chemotherapy drugs, can hinder magnesium absorption and should be managed accordingly. In conclusion, recognizing the signs of magnesium deficiency, understanding its causes, and knowing how to address it through supplementation or dietary adjustments are essential for maintaining optimal health. Consulting healthcare providers for accurate diagnosis and personalized treatment plans is vital in managing magnesium deficiency effectively. This article is not intended to offer medical advice, and is for informational purposes only. Please consult a medical professional for personal advice on celiac disease, magnesium deficiency, and/or any other medical concern.
-
- absorption
- causes
- (and 8 more)
-
Celiac.com 02/29/2020 - It has been a long and winding road, and around each curve something new has been discovered. I have learned more than I ever thought there was to know about celiac disease. I am forever grateful for having received a celiac diagnosis because it was on that day that I began my journey back to health. On my first day of diagnosis I set out to find out as much as possible about this seemingly rare, but obviously complicated disease. My diagnosis answered a lot of questions for me, yet I was also struck by how many new questions arose. What was the trigger for celiac disease, of course gluten played a part, but what in my past history put me over the edge? What had changed? Did the doctors know so little about the trigger for celiac disease that it was only now becoming clinically identifiable? My last article was an attempt to explain how genetics and environment intersect in celiac disease, but I may have gotten part of it wrong, in part because the International Journal of Celiac Disease (IJCD) got it wrong (at least in my case they did). After the IJCD cited Pellagra in celiacs at a 58% percent rate, I piled on the bandwagon. Quoting “The two diseases can be connected in two aspects. 58% of pellagra patients were shown to have malabsorption and many had intestinal pathology on biopsies.” But we were both wrong I now believe—hold onto that 58% thought, as it will come up later—and I think it's important in helping to confirm my new theory. So where did my pellagra position go wrong? I chose the capstone, pellagra, and not the cornerstone, which may actually be thiamine (B1), and this is easier to do than you might imagine. These diseases have diffuse symptom’s common in their pathogenesis, and only testing can confirm my high suspicion that I may have had undiagnosed, or misdiagnosed, beriberi. Beriberi is is caused by low thiamine (B1). I recently came across research that is 30+ years old that establishes, in mammal’s at least, a trigger for thinning villi titled “Effect of dietary thiamin deficiency on intestinal functions in rats.” To quote from the research “The activities of brush border sucrase, lactase, maltase, alkaline phosphatase, and leucine aminopeptidase were reduced by 42 to 66% in thiamine deficiency, compared to pair-fed controls. Kinetic studies with sucrase and alkaline phosphatase evinced that a decrease in Vmax (61 and 64%, respectively) with no change in Km (33.8 and 4.3 mM, respectively) was responsible for observed impairment in the enzyme activities in thiamine deficiency.” This research leads me to believe that the lactose intolerance so common in those with celiac disease may actually be triggered by thiamine deficiency. I had many of the symptom’s of beriberi, but since I was not in a concentration camp or was not an alcoholic the clinical suspicion was not high enough to have me tested for a thiamine deficiency, despite thiamine and other B vitamins deficiencies that are common in celiac disease. Unfortunately even going on a gluten-free diet does not always correct B vitamin deficiencies, and thiamine, niacin and riboflavin deficiencies have been excluded from most celiac disease studies. One study entitled “Evidence of poor vitamin status in Celiac patients on a gluten-free diet for 10 years" shows that such deficiencies can continue long after diagnosis. Another study entitled “Vitamin and Mineral Deficiencies Are Highly Prevalent in Newly Diagnosed Celiac Disease Patients” says: “Almost all celiac disease-patients (87%) had at least one value below the lower limit of reference.” Testing for certain vitamin deficiencies is standard care following a celiac disease diagnosis, however levels of thiamine (B1), niacin (B3) and riboflavin (B2) are not usually part of a standard screening. It is my hope from reading this that you are alerted to possible B vitamin deficiencies so that you can ask your doctor to have your levels checked, especially if you have been recently diagnosed, or are still struggling with diffuse symptoms years later, for example fatigue, muscle cramps, tingling in your feet and hands, burning feet syndrome, worse at night, etc. You may still be low in thiamine, riboflavin and/or niacin, and doctors often overlook screening for these deficiencies in celiac disease. Celiac Disease is a Genetic Disease with an Environmental Trigger This is where B vitamins come in, as they help us make energy and regulate our environment at the cellular level. It is a 50/50 equation of stress vs. environment combined with genetics, and this can be a hard concept to understand because many people believe that it's all due to DNA. Research from December 2019 entitled “DNA Has Relatively Little Say in Disease Risk (Usually)” says: “In fact, for such (most) diseases, the genetic contribution to disease risk is just 5–10%. There are diseases, however, for which the genetic contribution is about 40–50%. These diseases include Crohn’s disease, celiac disease, and macular degeneration.” B Vitamins, Especially Thiamine (B1), Could be the Missing Pieces to the Puzzle Via the Parasympathetic Nervous System (PNS) the neurotransmitter "acetylcholine" regulates our organ functions throughout the body, and could be why both undiagnosed celiac disease and beriberi affect so many organs in the body. Without enough thiamine our body can’t synthesize enough acetylcholine to regulate it’s organs, which may cause the body to go into high alert mode and trigger a runaway auto-immune reaction like celiac disease. Another study shows a connection with the microvilli that line organs and how they can trigger auto-immune reactions throughout the body. What about that 58% I mentioned earlier? It happens to be the same rate that Japanese sailors developed beriberi, which is what you would expect to find when someone relies on too many carbs, including too much rice or wheat in their diets. It's possible that when the carb happens to be wheat this deficiency could trigger celiac disease, a disease that was discovered by Willem-Karel Dicke in the post WWII Netherlands, or present itself as beriberi when one only eats rice. It took 20 years and countless deaths before the Japanese army discovered what the Japanese navy had learned 20 years earlier, and this article on the “Barley Baron” supports why there is a strong need to enrich gluten-free bread with B vitamins, exactly as regular wheat bread is enriched. According to this article, "(w)e now know that beriberi stems from a lack of vitamin B1, which the body requires for metabolizing carbohydrates and maintaining neurological functions. Without it, a person succumbs to nerve damage and eventually death." So, perhaps a thiamine deficiency is one of the overall environmental triggers of celiac disease in those who have the genetic disposition? Could beriberi trigger celiac disease in susceptible individuals? Hopefully more research will be done to determine this, but in the meantime, get your thiamine levels checked! Additional Resources: https://www.ncbi.nlm.nih.gov/pubmed/23379830 https://www.ncbi.nlm.nih.gov/pubmed/29982183 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4863043/
- 22 comments
-
- celiac disease
- niacin
-
(and 5 more)
Tagged with:
-
Celiac.com 04/13/2024 - In recent legal proceedings, a Biden-appointed judge made a significant decision that could impact the way prisoners receive medical care, particularly concerning dietary needs. The case in question, Phoenix v Amonette, shed light on the challenges faced by prisoners with specific medical conditions, such as celiac disease. Judge Toby Heytens, nominated to the Fourth Circuit court of appeals, rendered a decision that overturned a lower court ruling, providing prisoners with an opportunity to prove their claims of constitutional and statutory rights violations. The Phoenix case centers around Daniel Phoenix, a Virginia prisoner suffering from celiac disease, an autoimmune disorder triggered by gluten consumption that can lead to severe digestive issues and other health complications. Despite being diagnosed with celiac disease and receiving medical advice to adhere to a gluten-free diet, Phoenix's condition worsened while in prison. He experienced sharp abdominal pain and even vomited blood, necessitating hospitalization. Following hospital discharge, Phoenix was instructed to follow a strict gluten-free diet. Prison Doctor Discontinued Phoenix's Gluten-Free Diet However, complications arose when the prison doctor discontinued the diet order, citing reports that Phoenix had consumed gluten-containing food from the commissary. This decision persisted despite further medical tests confirming Phoenix's celiac disease diagnosis. Feeling neglected and facing deteriorating health, Phoenix resorted to legal action, accusing the prison and the doctor of disregarding his serious medical needs in violation of constitutional rights. Initially, the lower court ruled against Phoenix, citing missed deadlines and the absence of expert testimony. However, Judge Heytens' recent decision overturned this ruling, emphasizing the need to consider disputed factual issues and the doctor's potential indifference to Phoenix's medical condition. Importantly, Heytens highlighted that expert testimony might not be necessary to contest summary judgment, opening the door for Phoenix to present his case without additional expert witness reports. Lack of Gluten-Free Diets in Prisons is a Worldwide Issue While the legal battle in Phoenix v Amonette unfolds, it raises broader questions about medical care access for prisoners worldwide, especially those with specific dietary requirements like gluten-free diets. The lack of availability or acknowledgment of such specialized diets in prison settings can lead to severe health consequences for affected individuals. This issue is not unique to the United States but extends to prisons globally, highlighting the need for comprehensive policies and practices that prioritize prisoners' medical rights and accommodations. As discussions around prisoner rights and medical care continue, it's crucial to address the challenges faced by individuals like Daniel Phoenix and advocate for systems that ensure equitable access to necessary medical treatments, including specialized diets like gluten-free options. By recognizing and addressing these issues, we can work towards a more just and inclusive approach to healthcare within carceral environments. Read more at: pfaw.org
-
- celiac disease
- court
- (and 8 more)
-
Celiac.com 04/09/2024 - Speculation about the source or cause of Napoleon's famous itch is fun, but much of the speculation seems to ignore the facts that point to the most likely answer. Napoleon's autopsy revealed gastric cancer and dermatitis herpetiformis, a condition associated with celiac disease. This is a historical fact. Despite this, speculation persists among historians and others, including dermatologists at the American Academy of Dermatology, regarding the potential causes of Napoleon's chronic itch. While some theories, such as scabies or arsenic exposure, lack substantial supporting evidence, they continue to be discussed. Zachary Leibovit-Reiben and colleagues at the University of Arizona College of Medicine recently presented research on Napoleon's itch, aiming to raise awareness of the nature of his chronic itchiness. Chronic itch, while often underestimated, is gaining recognition in dermatological research, with numerous presentations and discussions dedicated to it at the American Academy of Dermatology meeting. Leibovit-Reiben's team explored various potential causes, including scabies, arsenic exposure, atopic dermatitis, and psychogenic pruritus. However, given the autopsy findings of gastric cancer and dermatitis herpetiformis, which is linked to celiac disease, these realities should be considered the most plausible explanations. As to why they do not focus their speculation upon these two facts, anyone's guess is as good as mine. By reconciling historical speculation with medical evidence, this research aims to provide a clearer understanding of Napoleon's mysterious itch and its possible impact on his life. However, speculation, absent hard evidence, is unlikely to produce a fruitful avenue for revelation. Further investigation into Napoleon's medical history may shed light on this intriguing aspect of his health, and contribute to broader discussions on the intersection of historical narratives and medical science. However, students of history, especially those with a foothold in medicine and science, should probably begin with the actual historical and medical facts established by the official autopsy, as it is the one solid historical piece of evidence that is thus far, uncontested. Napoleon Suffered from Dermatitis Herpetiformis and Gastric Cancer If Napoleon did in fact suffer from dermatitis herpetiformis, and if he did in fact suffer from gastric cancer, then the results of the autopsy would seem to point in the direction of those two conditions, and, potentially to celiac disease. So why all the wild speculation that seems to ignore the official autopsy results? Any why is this fact-free speculation being driven by medical students, and/or doctors at a medical conference? Arguing for celiac disease is certainly speculative, and unlikely to come with smoking gun evidence. But it's a lot closer to being supported by actual observational evidence than speculation based on anecdotal evidence, however historically supported. If doctors and others are going to speculated on the potential cause of Napoleon's famous itching, shouldn't they confine themselves as close as possible to the known facts? Without that as a baseline, this type of speculation seems wholly ungrounded in science or medicine, and more akin to gossip or fantasy. As such, it is neither informative, nor likely to be produce any strong conclusions. Read more at Managedhealthcareexecutive.com
-
Celiac.com 12/21/2017 - After a lot of trial and error we celiacs learn, often the hard way, to eliminate foods that are poisonous to our bodies. Sadly, we often forget about what "goes onto" our skin. Since the skin is the living outer layer of our bodies it absorbs not only water and oils, it also absorbs cosmetics that can be poisonous to our celiac bodies, most specifically those of us afflicted with dermatitis herpetiformis (often called celiac disease of the Skin). Men, before you set this article aside, thinking it's only for women and you are exempt, please read on. One of 133 Americans has a wheat-related allergy according to CNN.com. We have a tendency not to group toothpaste and lip-glosses with cosmetics, and we usually ignore vitamins and medications when researching celiac disease and dermatitis herpetiformis. We forget to ask our hairdresser what products they are using and whether they contain wheat or gluten, and glibly apply night creams (to absorb into our skin as we sleep) and mud packs that promise similar benefits. Inquiring into the gluten content of cosmetics, I contacted more than twenty leading companies, then I waited. I was discouraged, particularly by the blatant rudeness of some of the responses I received. Meanwhile, I had to learn whether gluten could be absorbed through the skin. Some websites answered that question with a direct "no". Even some physicians responded saying "no". However, since the skin is the largest living organ in the body and it does absorb various oils and emollients, listing gluten-containing components of medicinal and non-medicinal ingredients allows consumers with celiac disease (celiac disease) or wheat allergies to make informed choices when purchasing and/or consuming natural health products. It enables them to avoid gluten in quantities that may trigger adverse reactions. There are numerous articles on dermatitis herpetiformis and celiac disease making claims so contradictory that it is no wonder we are confused. And I'm not talking about accidental ingestion of gluten. Some such articles claim that trace amounts of gluten One article insists that the skin is not going to absorb gluten, even though our skin is a living organism that can absorb suntan lotions, trans-dermal drugs, etc. It is so susceptible to absorption that when you place a slice of onion in your sock you will taste it in your mouth the following day. How can these websites make such contrary claims? The skin absorbs flavors as well as creams containing gluten. On the other hand, "Glutino" had an article on record, written on September 14, 2010, regarding "Hidden Gluten in Health and Beauty Products". It states that if you apply hand lotion that contains gluten and then prepare food you are exposing yourself to accidental ingestion and your food to cross contamination. They suggest a site called: naturallydahling.com, a site that lists gluten-containing ingredients commonly used in cosmetics. Research proving the full extent of how much your skin absorbs is still unavailable, but to those who believe that "what goes on, goes in", the cosmetic industry is full of unknowns. The size of gluten molecules suggests that they may not be able to pass through the skin, but chemicals and technology designed to enhance skin absorption are already present, if not prevalent, in the cosmetic industry. These chemicals are potentially dangerous and often go untested for negative health effects, yet are widespread in lotions, antiperspirants, perfumes and the "Great Mother Market" anti-wrinkle cosmetics. Since the cosmetic industry is self-regulated it is more important than ever to carefully read labels and use natural or organic products whenever possible. If you find yourself reacting to a particular cosmetic, it is possible that you may have an increased sensitivity to gluten, an allergy or even dermatitis herpetiformis. But wait a minute! Aren't we told that gluten cannot pass through the skin? I suffered terribly from the use of an "Anti-Frizz" product for my hair that caused a massive outbreak of dermatitis herpetiformis. I should have read the label all the way down to the end. I would have found, in very small print, "wheat germ oil". When researching for this article, I wrote to the company and mentioned my problems with their product. I received an apology and a sample of their "new and improved" "Frizz-Ease" product. They obviously do not know their own products and the fancy names they use are as confusing to them as they are to me. The "new and improved" product contained Avena Sativa, the Latin name for OAT. I was also told that I likely just had "hives" on the back of my scalp, as oats are still somewhat controversial. Some research suggests that oats in themselves are gluten free, but that they are virtually always contaminated with other grains during cultivation, harvest, distribution or processing. Recent research indicates that a protein naturally found in oats (avenin) contains peptide sequences closely resembling some peptides from wheat gluten. The oat peptides caused mucosal inflammation in significant numbers of celiac disease sufferers. Some examination results show that even oats that are not contaminated with wheat particles may be dangerous. Again, I was told not to introduce oats into my diet, or use oatmeal as a facial mask until I had been free of a dermatitis herpetaformis outbreak for at least a year. Thus far I have not been able to get relief for that long. It seems the celiac or those who suffer from dermatitis herpetiformis {and let's face it, most people suffering from dermatitis herpetaformis have celiac disease} have to apply the rule of "caveat emptor" - Let the buyer beware. Tolerance to gluten varies among individuals with celiac disease and there are limited clinical scientific data on a threshold for the amount of gluten required to initiate or maintain an immunological reaction in celiac disease patients. "Therefore there is no clear consensus on a safe gluten threshold level." The Dermatologist I see at The University of British Columbia Hospital has told me to tell people in restaurants that gluten is poison to my system and I can become very ill from ingesting gluten. They are a little more careful before telling me a dish is gluten free, and hopefully through education the cosmetic industry is going to improve its testing and cease glibly stating things as "fact" when they simply do not know. Industries that produce over-the-counter medications and vitamin supplement, especially those that may contain gluten as a binding agent, should also be scrutinized. We have come a long way, but large challenges are still ahead. One of our biggest challenges is reading the labels on these products. One almost needs to carry a magnifying glass when shopping. Cosmetics, which include hair products, soaps, perfumes and toothpastes also run us into problems, often big, "itchy" problems. The male celiac/dermatitis herpetaformis experience can also include outbreaks from any product that comes into contact with the skin and particularly those that "stay" on the hair or skin. Who would have known that sun tan lotions could contain wheat germ oil? It is difficult enough to eliminate words such as "triticum vulgare" the Latin name of wheat or "wheat germ" containing ingredients! In preparation for this article, I contacted the following companies: Avon, Clairol, Clarins, Clinique, Coty, Covergirl, Estee Lauder, Garnier, John Frieda, John Paul Mitchell, L'Oreal, Mabelline, Marcelle, Neutrogena, Olay, Pantene, Revlon, and companies that go under general all-encompassing headings such as "Life Brand". This can be a daunting task, and "gluten free" and "wheat free" are not the same thing. Some of the things that I learned in this rather massive undertaking include the rule of "Pac Man". Companies are sometimes taken over by bigger companies and when this occurs their rules change. A company that at one time did not test on animals or use machines that were cleaned prior to using products claiming to be gluten free are now glibly adopting the "new bigger and better". I was shocked to find out that some of the containers from the smaller company were still being used after these PAC MAN take-overs, to save on manufacturing costs. And, remember, once several ingredients are combined the "organic" ingredient probably ceases to be "organic". Some women (and men, you are not exempt here) expect to pay a higher price for a luxury brand assuming that the gorgeous bottle of eye cream sold at Saks for $60.00 is going to work better than the $1.99 tube on the clearance rack of a local store. Just ensure the product has not reached its "sell by" date because it may all be psychological. What you have to concern yourself about, as a celiac patient or a person with dermatitis herpetiformis, is whether there is gluten or wheat in that product. Before you splurge on an expensive product take the time to compare it to a similar product from one of their sister brands. Usually an online store (like Drugstore.com) will list the ingredients. Or you can check on a site like "Makeup Alley" which is a great resource, offering numerous reviews and you can ask questions of the extremely knowledgeable posters on this message board. Another great resource is a large paperback book, titled "Do not go to the Drugstore Without Me" written by Paula Begoin. When I purchased the books in 2001 it was in its 5th Edition. NB: This is not a book specifically for celiac disease or dermatitis herpetiformis, but it was in this book that I found out about "Glutamic Acid". It is derived from wheat gluten and is an amino acid that can have water binding properties for the skin. It also explains glycerylesters that form a vast group of ingredients that are a mixture of fatty acids, sugars, and non-volatile alcohols. These fats and oils are used in cosmetics as emollients and lubricants as well as binding and thickening agents. At the back of this book is a list of the companies that do not test on animals and those that do, but again, the PAC MAN Rule applies. I purchased the book for myself, my daughter, and daughter-in-law, specifically because when my daughter was in her twenties she seemed to think she simply must buy her shampoo from the hairdresser because only $45.00 shampoo was good enough for her hair. It was a big eye opener when she moved out of home and had to purchase it herself! I believe that the more we know about beauty products and the beauty industry the wiser our purchases will be. Consider, for instance, the cost of research and development for say, L'Oreal who develop formulas that can be used in Garnier Shampoos ($3.99) and Kerastase shampoo ($29.99) It doesn't take long to realize that it is a good idea to compare products at different ends of the price scale. Sometimes, two products from two different brands will have the same patent number. The difference is in the non-active ingredients, which give it a unique texture, scent and/or color. Also, it is wise to photo-copy, and even apply plastic covering to lists of "safe" beauty products, just as it is wise to keep a copy of "safe" and "unsafe" foods on hand when you go shopping. When you cannot even pronounce some of the words used in foods and beauty products how can you be expected to remember what is safe to apply to your hair and skin? I received a very nice letter from Teresa Menna, Manager at L'Oreal in Quebec who told me that L'Oreal has abolished gluten in the composition of L'Oreal products. However, on reading more literature I find that Garnier is a mass market cosmetic brand of L'Oreal, and L'Oreal is part of the Group P&G. P&G stands for Proctor and Gamble and P&G Beauty brands can be found on the site:_ http://pgbeautygroomingscience.com/product.php {The Company Garnier Laboratories was started in 1906 and acquired by L'Oreal in the 1970's}. I was unaware prior to researching this article that L'Oreal owned Kerastase, or that L'Oreal had purchased the MAC Cosmetic line, or that the KAO Brands Company owns Ban, Biore, Jergens and John Frieda. Here are some of the ingredients you might find in cosmetics that could indicate wheat or gluten: Avena Sativa {Latin name of oat, or "oat" term containing ingredients Hordeum distichon {Latin name of barley, or "barley" term containing ingredients} Hydrolyzed malt extract Hydrolyzed wheat protein Hydrolyzed vegetable protein Wheat germ Vitamin E Cyclodextrin Barley extract Fermented grain extract Oat (Avena sativa) Samino peptide complex Secale Cereale (Latin name of rye, or "rye" term containing ingredients) Stearyldimoniumhydroxypropyl Phytosphingosine extract Triticum vulgare {Latin name of wheat, or "wheat" term containing ingredients} Dextrin Dextrin palmitate Maltodextrin Sodium C8-16 Isoalkylsuccinyl Wheat Protein Sulfonate Yeast extract Anything with wheat in the name Thoughts: Some cute person gave the warning to ensure your lipstick is gluten free even if you don't have any skin issues. You could swallow some lipstick and get gluten in your system! Another person adds at the bottom of their e-mail to be sure to check guidelines regularly because company policies can change yearly and the list is only to be considered as "guidelines" and make-up ingredients can change each time a company changes or the scientists within that company decide to add to or delete certain products. {Makes you feel very safe as a celiac/dermatitis herpetaformis person doesn't it?} Another e-mailer suggested that mascara labeled as a "thickening agent" should be fearfully evaluated by the celiac/dermatitis herpetaformis person because the thickening agent is often "flour" and can sometimes cause eyelashes to fall out! Who knew? Noted on one e-mail, ‘So-called luxury brands can be laden with synthetic ingredients that do not cost more than their not so luxurious counterparts. True natural products that do perform, and there are a few such brands on the market, are authentic natural products that actually deliver what they promise and they truly do cost more to make because raw ingredients are much higher in cost. In fact, the cost is significantly higher when pure high grade ingredients are used. Letter received: " We have compiled a list of gluten free beauty products available on sephora.com. These products do not contain any wheat, rye or barley derivatives, and they were made in gluten-free laboratories so there is no chance of cross-contamination. But since you cannot be too careful, discontinue use of any product that triggers an attack." Letter received from Clairol:- "Gluten is a protein found in wheat, rye and barley. Although it is not added directly to our product, it may be present in fragrances. Due to the difficulty of tracing the source ingredients for the variety of fragrances used in manufacturing our products, we cannot provide specific levels of gluten content for any of our fragrance blends. Be aware that even products labeled "unscented" will still contain masking scent, therefore they may potentially contain gluten." Advertisement: World's Top Ten Cosmetic Companies : "Beauty begins on the inside, check out our post on ‘The Top Five Foods for Amazing Skin'" - Posted by The Greenster Team "I finally got up the nerve to go through my own (their) personal care products and look them up on "SKIN DEEP" and was very disappointed. The Company that makes my mascara (L'Oreal) tests on animals as does the company that makes my eyeliner (Covergirl) and my under eye concealer (Made by Physician's Formula) contains parabens" THE GREENSTER TEAM creates great articles, list the top ten cosmetic companies, what portion of the world's market they share and their hazard range. Letter received from Mabelline:- "Please find below most ingredients containing gluten (wheat and other grains). We invite you to take this list and compare it to our ingredient listings every time you buy a new product. When in doubt, do not hesitate to do your own research or contact your doctor." {Caveat Emptor} REMEMBER:- The truth is that there is no such thing as gluten free. The FDA has proposed a less than 20 ppm gluten -free standard in 2006. That was its first attempt to define the term gluten free, but the agency has yet to finalize it. The USDA is awaiting the FDA's decision before moving ahead. STILL WAITING. With the number of products making unregulated gluten free claims on the rise, the marketplace can be scary for consumers with gluten sensitivity and wheat allergies. Why hasn't the FDA finalized its 2006 definition of gluten free? As part of sweeping legislation known s FALCPA the Food Allergen Labelling and Consumer Protection Act of 2004, Congress ordered the FDA to define and permit the voluntary use of the term gluten free on the labeling of foods by August 2008. As directed, the FDA issued proposed gluten-free regulations on schedule but seems to have failed to follow through with a final ruling. There has been no explanation for the delay. Since the Cosmetic Industry is a self-regulating body it seems {appears, is assumed} that we the consumers are on our own as far as researching what goes on our skin and in our hair, because some of the letters I have received leave it to the celiac or dermatitis herpetiformis sufferer to research their own products. Even a letter from Avon states:- "Although Avon sells quality products, there is always possibility of contamination during manufacturing or changes/substitutions of ingredients. As with everything related to celiac disease, dermatitis herpetiformis and gluten Intolerance, products, ingredients and preparation may change over time. Your reactions to a specific product, ingredient may be different from the reactions of others. Like eating at a restaurant, you have to make a choice whether to consume/use a product. The list is meant to be a "guide" and does not guarantee that a product is 100% free of gluten. Dacia Lehman, Avon and GIG assume no responsibility for its use and any resulting liability or consequential damages is denied." LETTER: - Proctor and Gamble "The WHMIS rating is designed to rate raw materials and not formulated products such as ours. Nor are our consumer products required to be labeled under the Occupational Safety and Health Administration (OSHA) Hazard Communication Standard. Thus labelling of our products with WHMIS ratings or any other hazard rating should not be required by any state health and safety regulatory agencies." That letter is signed by Asela for the Pantene Team. LETTER:- May 2, 2012 - xyz@ca.loreal.com - "We have received your message and we will get back to you as soon as possible. Web Sites: Gluten-free Lifestyle: glutenfree-lifestyle.com (Gives gluten free products by type and by company) i.e.: deodorants, face & body wash, make-up, suntan lotion, toothpaste, moisturizer, lotion, shampoo & conditioner, shave cream, gels, after shave, laundry products, cleaners, soap, etc. Beauty Industry: Who Owns What? Glutino - Hidden Gluten in Health Products - Glutino & Gluten Free Pantry Blogs: www.gluten-free-cosmetic-counter.org Beauty Blogging Junkie Ebates Shopping Blog In The Makeup Lipstick Powder n'Paint Shop With a Vengeance Smarter Beauty Blog The Beauty Brains Sephora Sephora's iGoogle Beauty Portal References: Codex Standard for Foods for Special Dietary Use for Persons Intolerant to Gluten. Codex STAN 118 - 1979 ROME Government of Canada 2008 - Regulations Amending the Food and Drug Regulations (1220- Enhanced Labeling for Food Allergen and Gluten Sources and Added Sulphites) Health Canada 2007 - celiac disease and the Safety of Oats Labeling of Natural Health Products Containing Gluten - Health Canada Notice 2010
-
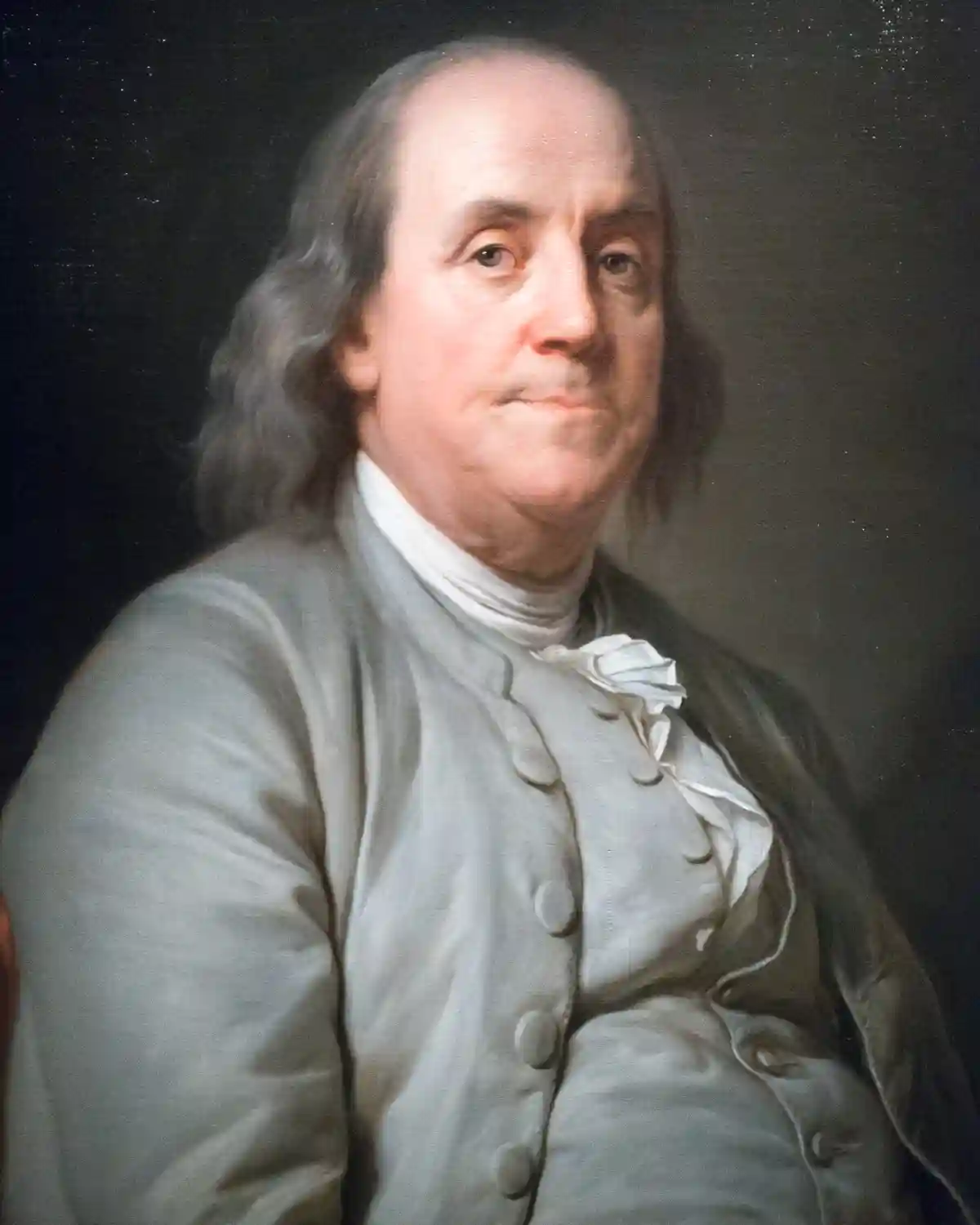
Celiac.com 04/06/2024 - Benjamin Franklin, one of America's most renowned Founding Fathers, was a man of many talents and achievements. From his contributions to science and literature to his pivotal role in shaping the nation's early history, Franklin's legacy is undeniable. However, behind the brilliance and accomplishments, there may have been a hidden health struggle that modern medicine could shed light on: celiac disease. In this speculative exploration, we delve into the possibility of Benjamin Franklin having celiac disease. While no definitive medical records exist to confirm this hypothesis, we rely on historical reports of Franklin's health issues and current understanding of celiac disease symptoms to speculate on this intriguing aspect of his life. Benjamin Franklin's Known Symptoms: Could They Mean Celiac Disease? Historical accounts of Benjamin Franklin's health often mention various symptoms that could potentially align with celiac disease. Reports indicate that Franklin experienced chronic gastrointestinal issues, including bloating, gas, and diarrhea. These symptoms are hallmark indicators of celiac disease, a condition characterized by an immune reaction to gluten, a protein found in wheat, barley, and rye. Furthermore, Franklin reportedly suffered from skin rashes and irritations, which are common extraintestinal manifestations of celiac disease. Dermatitis herpetiformis, a skin condition linked to celiac disease, often presents as itchy, blistering rashes on the elbows, knees, scalp, and buttocks. While historical descriptions of Franklin's skin issues are not conclusive evidence, they raise intriguing parallels with celiac-related dermatological symptoms. Could A Genetic Sample Exist to Determine if Benjamin Franklin Had Celiac Disease? Advancements in genetic testing have revolutionized our ability to diagnose and understand various medical conditions, including celiac disease. Genetic markers associated with celiac disease, such as the HLA-DQ2 and HLA-DQ8 genes, can be identified through DNA analysis. This begs the question: could a genetic sample from Benjamin Franklin or his descendants provide insights into his potential predisposition to celiac disease? While obtaining a genetic sample from historical figures presents logistical challenges, it is not entirely implausible. Descendants of Benjamin Franklin may possess genetic material that could be analyzed for celiac-related markers. However, this hypothetical scenario would require extensive collaboration between historians, geneticists, and medical professionals to access and analyze such genetic data ethically and accurately. Several locks of Benjamin Franklin's hair are known to exist, including one held by the Library Company of Philadelphia. Private collectors and museums also possess locks of Franklin's hair. While these physical items could potentially retain DNA that could be used for genetic analysis, the condition of the DNA and the feasibility of extracting viable genetic material depend on factors such as preservation methods and environmental conditions over time. If a suitable genetic sample could be obtained from these locks of hair, it might offer insights into whether Benjamin Franklin could have had celiac disease. Exploring Franklin's Dietary Patterns: Clues to Celiac Disease? Another aspect worth considering is Benjamin Franklin's dietary habits and preferences. Historical records suggest that Franklin adopted a vegetarian diet later in life, favoring fruits, vegetables, and grains like corn and possibly oats. While this dietary shift aligns with modern recommendations for managing celiac disease, it is essential to note that gluten-free diets were not recognized or understood during Franklin's era, and it is possible that he also included wheat and rye in his diet. However, Franklin's reported avoidance of certain foods, particularly those that caused digestive discomfort, could indicate an intuitive response to gluten-related issues. Additionally, his documented interest in health and wellness, as evidenced by his writings on nutrition and exercise, hints at a potential awareness of dietary influences on well-being. Given Franklin's reputation as a keen observer and a proponent of scientific inquiry, it's plausible to speculate that he may have used scientific methods to identify foods that caused him discomfort. Franklin was known to be health-conscious and mindful of his diet, which aligns with the behavior of someone who may have had undiagnosed celiac disease or gluten intolerance. Historical records suggest that Franklin was selective about his food choices and avoided certain items that he believed were detrimental to health. He promoted moderation in eating and emphasized the importance of a balanced diet, indicating a level of awareness regarding the impact of food on well-being. Considering his documented health issues, such as his gout and digestive complaints, it's reasonable to assume that Franklin may have experimented with different foods and dietary patterns to alleviate symptoms. His avoidance of heavy, rich foods and preference for lighter fare further support the notion that he was attuned to how food affected his body. While there is no direct evidence linking Franklin to celiac disease or gluten intolerance, his lifestyle and dietary preferences suggest a level of awareness and experimentation that aligns with modern approaches to managing gluten-related disorders. The Enigma of Benjamin Franklin's Health In conclusion, the question of whether Benjamin Franklin had celiac disease remains an intriguing and speculative aspect of his life. While historical accounts provide glimpses into Franklin's health struggles, definitive evidence linking him to celiac disease is lacking. Future research, including genetic investigations and interdisciplinary collaborations, may offer new insights into Franklin's health legacy and the potential intersection with celiac disease. As we continue to unravel the mysteries of historical figures' lives, Benjamin Franklin's health journey serves as a reminder of the complexities and nuances of medical history. Speculative explorations like this invite curiosity and dialogue, bridging the past with modern medical understanding in fascinating ways.
-
Celiac.com 10/27/2014 - There have been a few reports tying cortical myoclonus with ataxia to celiac disease. Such reports also suggest that the former is unresponsive to a gluten-free diet. A team of researchers recently set out to determine if there is any significant connection between the two conditions. The research team included Ptolemaios G. Sarrigiannis, Nigel Hoggard, Daniel Aeschlimann, David S. Sanders, Richard A. Grünewald, Zoe C. Unwin, and Marios Hadjivassiliou. They are variously associated with the Departments of Gastroenterology, Neurology, Neurophysiology and Neuroradiology at Royal Hallamshire Hospital, in Sheffield, UK, and with the College of Biomedical and Life Sciences at Cardiff University in Cardiff, UK. The team presented detailed electro-clinical characteristics of a new syndrome of progressive cortical hyperexcitability with ataxia and refractory celiac disease. Regular follow ups of over 600 patients with neurological manifestations due to gluten sensitivity revealed 9 patients with this syndrome. They found that all nine patients, six men and three women, experienced asymmetrical irregular myoclonus involving one or more limbs and sometimes face. This was often stimulus sensitive and became more widespread over time. Three patients had a history of Jacksonian march, and five had at least one secondarily generalized seizure. Electrophysiology showed evidence of cortical myoclonus. Three showed a phenotype of epilepsia partialis continua at onset. All patients showed clinical, imaging and/or pathological evidence of cerebellar involvement. All patients followed a strict gluten-free diet, and most successfully eliminated gluten-related antibodies. However, all patients still showed evidence of enteropathy, suggests that refractory celiac disease is to blame. During the study, two patients died from enteropathy-associated lymphoma and one from status epilepticus. Five patients were treated with mycophenolate and one in addition with rituximab and IV immunoglobulins. These patients showed improvement of ataxia and enteropathy, but continued to suffer the effects of myoclonus. These results indicate that myoclonus ataxia might be the most common neurological manifestation of refractory celiac disease. The clinical involvement, apart from ataxia, covers the whole clinical spectrum of cortical myoclonus. Source: Open Original Shared LinkOpen Original Shared Link
- 13 comments
-
Celiac.com 04/01/2024 - Recent research has shed light on a concerning correlation between celiac disease and various reproductive disorders in women, emphasizing the importance of awareness and proactive healthcare measures for individuals living with this autoimmune condition. According to a study presented at the 2023 annual meeting of the American College of Gastroenterology by lead researcher Rama Nanah, MD, patients with celiac disease face significantly elevated risks for several female reproductive disorders compared to those without the condition. The study, drawing from the comprehensive TriNetX database, revealed that women with celiac disease have a two times higher risk for endometriosis, three times higher risk for polycystic ovary syndrome (PCOS), and six times higher risk for ovarian dysfunction. The association between celiac disease and female reproductive disorders has been noted in previous studies, but the latest findings add new dimensions to our understanding. Notably, the study uncovered increased rates of PCOS and endometriosis among women with celiac disease, highlighting the urgent need for further investigation into these connections. A Range of Reproductive Health Abnormalities Associated with Celiac Disease The retrospective analysis, which included over 9,000 women with celiac disease and more than 25 million healthy controls, revealed a range of reproductive health abnormalities associated with celiac disease across different age groups. These include menstrual irregularities, delayed menarche, infertility, recurrent pregnancy loss, and pain associated with menstruation. Despite the compelling data, the exact mechanism underlying the association between celiac disease and reproductive disorders remains unclear. Dr. Nanah emphasized that the study did not establish causality, nor did it provide insights into whether adherence to a gluten-free diet could mitigate reproductive risks. While the study underscores the importance of considering undiagnosed celiac disease in women with gynecologic disorders, it also highlights the need for prospective studies to validate these findings and explore potential screening and risk reduction strategies. Benjamin Lebwohl, MD, MS, director of clinical research at the Celiac Disease Center at Columbia University, stressed the importance of future research to further elucidate these associations and inform evidence-based healthcare practices. For individuals living with celiac disease, the study underscores the importance of comprehensive healthcare management that includes regular screenings and discussions about reproductive health. By raising awareness and advancing research in this area, healthcare professionals can better support the unique needs of women with celiac disease, ultimately improving their overall quality of life and well-being. Read more at Gastroendonews.com
-
- celiac disease
- female
-
(and 5 more)
Tagged with:
-
Celiac.com 03/28/2024 - Twenty years after an initial landmark survey, the latest update by Celiac Canada shows little has changed for hundreds of thousands of Canadians living with celiac disease. Celiac Canada reveals ongoing challenges for Canadians living with celiac disease. Living with celiac disease in Canada continues to pose significant challenges, according to the latest survey conducted by Celiac Canada. The survey, titled "State of Celiac Disease in Canada: 20 Years Later," highlights persisting issues of underdiagnosis, unaffordable gluten-free diets, and difficulties accessing safe food for individuals with celiac disease. Celiac disease, an autoimmune condition triggered by ingesting gluten found in wheat, rye, and barley, affects about one percent of the world's population. However, up to 80% of affected individuals remain undiagnosed, leading to painful symptoms and potential long-term health complications. The Survey's Key Findings: Gathered from 7,500 Canadians Living with Celiac Disease Delays in Diagnosis: Despite increased awareness of gluten-free diets, many Canadians still face significant delays in receiving a celiac disease diagnosis, with some waiting up to 10 years for proper identification of symptoms. Changing Symptoms: Neurological symptoms such as anxiety, brain fog, and headaches are becoming increasingly prevalent among individuals with celiac disease, alongside traditional gastrointestinal symptoms like bloating and diarrhea. Affordability: The high cost of gluten-free foods remains a top concern for respondents, impacting their dietary choices and financial well-being. Gluten-free products can cost up to 500% more than conventional counterparts, placing a significant financial burden on individuals with celiac disease. Risk of Unsafe Foods: Accessing safe gluten-free foods, particularly in hospitals and care homes, remains challenging for many respondents, increasing the risk of exposure to harmful gluten-containing products. Mental Health Impact: Following a gluten-free diet can contribute to feelings of frustration, isolation, and stress among individuals with celiac disease, affecting their social participation and overall well-being. To address these ongoing challenges, Celiac Canada has proposed several recommendations: Improving Diagnosis: Implementing standardized blood tests for celiac disease and developing new guidelines to enhance diagnosis rates and standards of care. Financial Relief: Introducing federal income tax claims to alleviate the financial burden of gluten-free diets, providing true financial relief for affected individuals. Ensuring Safe Foods: Requiring publicly funded health institutions to provide safe gluten-free food options and developing regulations for standardized allergen labeling in food service delivery. Regulating Food Labels: Implementing regulations to standardize the use of "gluten-free" labels on food products, ensuring accurate representation of product content. By addressing these recommendations, policymakers, healthcare professionals, and stakeholders can work together to improve the quality of life for Canadians living with celiac disease and promote greater awareness and understanding of this autoimmune condition. Read more at finance.yahoo.com
-
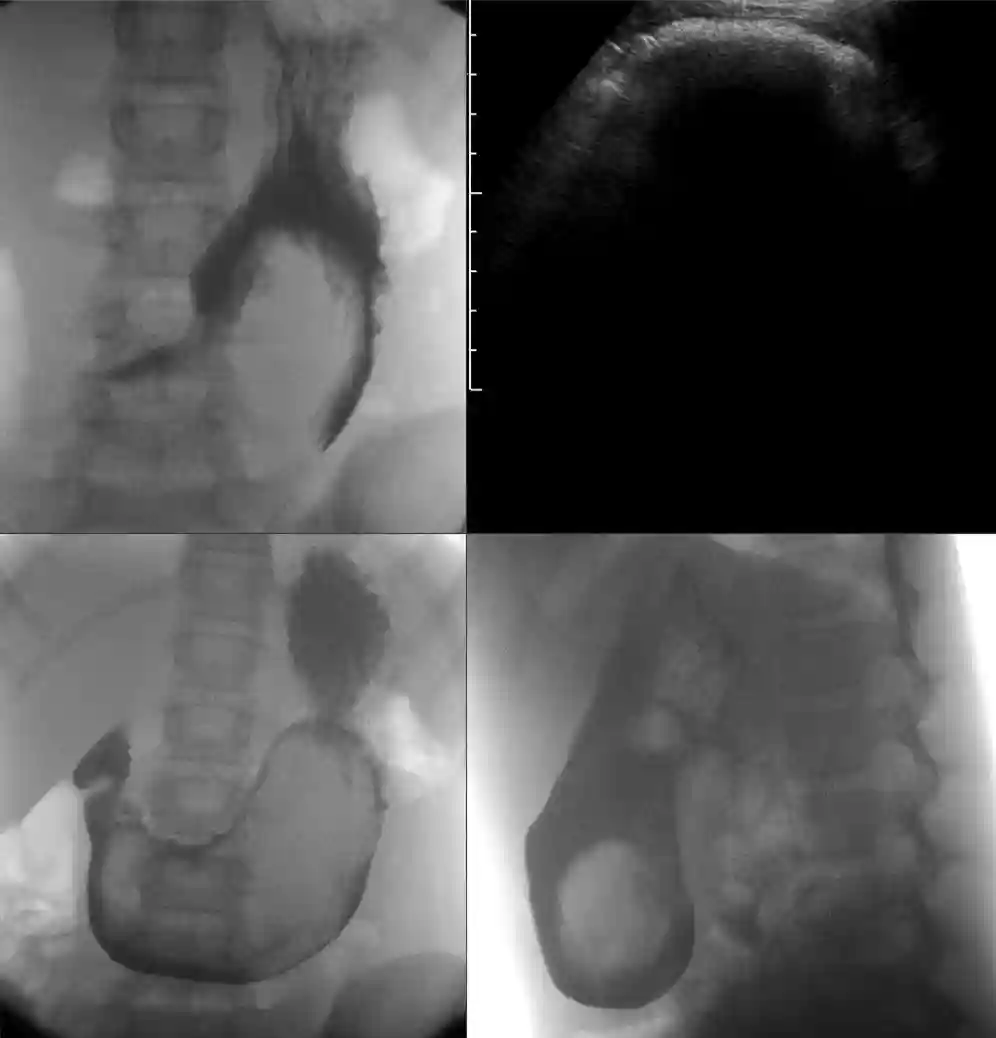
Celiac.com 03/11/2024 - Celiac disease, a condition triggered by gluten sensitivity in genetically susceptible individuals, affects approximately 1% of the global population. Traditionally, diagnosing celiac disease involves a stepwise process, beginning with blood tests to detect antibodies against tissue transglutaminase (tTG), followed by an invasive duodenal biopsy to confirm the diagnosis. However, this biopsy procedure poses risks and discomfort to patients. Recent research has explored the feasibility of diagnosing celiac disease without the need for a biopsy, relying solely on serological markers. A team of scientists conducted a retrospective analysis of medical records from biopsy-diagnosed celiac disease patients. They specifically examined the correlation between the severity of intestinal damage, as assessed by Marsh grading, and levels of anti-tTGA antibodies in the blood. The research team included Parul Punia, Kiran Bala, Mansi Verma, Ankita Nandi, Parveen Mahlotra, Sunita Singh, Seema Garg, Aparna Parmar, and Devender Kumar. They are variously affiliated with the departments of Microbiology, Pandit Bhagwat Dayal Sharma Post Graduate Institute of Medical Sciences, Rohtak, IND; Microbiology, PGIMS, Rohtak, IND; Gastroenterology, PGIMS, Rohtak, IND; and Microbiology, bps khanpur gmch, Sonepat, IND. Severity of Marsh Lesions Corresponds to Anti-tTGA Antibody Levels Their study included 94 symptomatic celiac disease patients with available anti-tTGA antibody reports. Among these patients, those with more severe intestinal damage, categorized as Marsh grade 3 lesions, consistently exhibited higher levels of anti-tTGA antibodies. Remarkably, serum antibody levels exceeding ten times the upper limit of normal (ULN) were strongly associated with Marsh grade 3 lesions. These findings suggest that in symptomatic adults with celiac disease, the severity of intestinal damage may be accurately predicted using blood tests alone, without the need for invasive biopsies. Specifically, anti-tTGA antibody levels exceeding ten times the ULN could serve as a reliable indicator of Marsh grade 3 lesions. Adopting a non-biopsy approach to diagnose celiac disease could offer several benefits, including reduced patient discomfort, avoidance of procedural risks, and potentially faster diagnosis and initiation of treatment. However, further research and validation studies are warranted to confirm the reliability and effectiveness of this approach across diverse patient populations. In conclusion, the non-biopsy approach for diagnosing celiac disease represents a promising avenue for improving patient care, and diagnostic efficiency, in people with celiac disease. Read more at Cureus.com
- 3 comments
-
- biopsy
- celiac disease
-
(and 4 more)
Tagged with:
-
Celiac.com 03/21/2024 - For people with celiac disease, managing symptoms and maintaining a gluten-free lifestyle are essential for overall health. However, recent research has uncovered another potential cause of enteropathy that presents a diagnostic challenge for both patients and healthcare providers: olmesartan-induced enteropathy. Olmesartan, an angiotensin II receptor antagonist commonly prescribed for hypertension, has been linked to enteropathy in rare cases, and another brand name for it is Benicar. This side effect, while uncommon, can manifest as chronic diarrhea, weight loss, and signs of malabsorption, mirroring the symptoms of celiac disease. A team of researchers set out to study the diagnostic challenges related to non-celiac enteropathy, specifically focusing on olmesartan-induced enteropathy. Here's what they found. The research team included Doukas S G, Doukas P G, and Velpari S. They are variously affiliated with the Department of Medicine, Saint Peter's University Hospital in New Brunswick, NJ, USA; the Department of Forensic Sciences and Laboratory of Toxicology, University of Crete, Medical School in Heraklion, GRC; and the department of Gastroenterology and Hepatology, Rutgers Robert Wood Johnson Medical School/Saint Peter's University Hospital in New Brunswick, USA. Their recent study focused on a 73-year-old woman who presented to the emergency department with watery diarrhea, weight loss, and electrolyte imbalances. Despite extensive testing, including celiac disease panels and imaging studies, the cause of her symptoms remained elusive until duodenal biopsies revealed moderate to severe villi blunting and intraepithelial lymphocytosis—a hallmark of olmesartan-induced enteropathy. History of Taking Olmesartan The patient's history of olmesartan use prompted the discontinuation of the medication, leading to a remarkable improvement in her symptoms and duodenal biopsy results within one month. This case underscores the importance of considering medication history and ruling out other potential causes of enteropathy in patients with symptoms suggestive of malabsorption. Olmesartan-induced enteropathy can mimic celiac disease both clinically and histopathologically, often leading to unnecessary diagnostic investigations and delays in appropriate treatment. Greater awareness of medication-related diarrheal syndromes, such as olmesartan-induced enteropathy, is crucial for prompt diagnosis and management. Healthcare providers should be vigilant in recognizing the potential link between olmesartan use and enteropathy, as simple discontinuation of the medication can lead to significant clinical improvement. For people with celiac disease and other gastrointestinal conditions, understanding the potential causes of enteropathy beyond gluten exposure is essential for effectively managing symptoms, and optimizing health outcomes. By staying informed and working closely with healthcare providers, patients can navigate the complexities of non-celiac enteropathy, and advocate for their well-being. Read more at Cureus 16(2): e54373. doi:10.7759/cureus.54373
-
- celiac disease
- connection
-
(and 3 more)
Tagged with:
-
Celiac.com 03/18/2024 - A recent study aimed to uncover the prevalence of celiac disease among individuals with systemic lupus erythematosus, shedding light on potential connections between the two conditions. Researchers conducted a thorough investigation, reviewing 14 studies that met their inclusion criteria. They analyzed data from over 1200 patients with systemic lupus erythematosus to determine the prevalence of biopsy-verified celiac disease and serological markers indicative of celiac disease. The research team included Adonis Sotoodeh, Madeleine Nguyen Hoang, Karin Hellgren, and Anders Forss. They are variously affiliated with the Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden; the Gastroenterology Unit, Department of Gastroenterology, Dermatovenereology and Rheumatology, Karolinska University Hospital, Stockholm, Sweden; and the Department of Medicine, Solna, Division of Clinical Epidemiology, Karolinska Institutet, Stockholm, Sweden. Serological Markers for Celiac Disease in Those with Systemic Lupus Erythematosus was 3.7% Surprisingly, the study found that the prevalence of biopsy-verified celiac disease in patients with systemic lupus erythematosus was comparable to that of the general population, at 0.7%. However, the prevalence of serological markers for celiac disease was slightly higher, at 3.7%. Despite these findings, the researchers did not identify any significant associations between the prevalence of celiac disease in individuals with systemic lupus erythematosus and various study characteristics or demographics. Based on these results, the researchers concluded that routine screening for celiac disease may not be necessary for all patients with systemic lupus erythematosus. However, they suggested that individual screening could be considered in cases where there is clinical suspicion or additional risk factors for celiac disease. While further research is needed to fully understand the connection between these two conditions, this study provides important guidance for healthcare professionals in managing patients with systemic lupus erythematosus, who may also be at risk for celiac disease. Read more in Lupus Science & Medicine at the BMJ
-
- celiac disease
- erythematosus
-
(and 3 more)
Tagged with:
-
Celiac.com 08/20/2020 - I am afraid that the following article might not make me very popular—if I had any popularity remaining after my last one! If you saw “The Paleo Template” here on these pages, you’ll recall that its ideas rest upon the theory that humans are healthiest when eating the types and classes of foods we’ve been consuming for the overwhelming majority of the roughly two and one half million years we’ve been on this earth. It wasn’t until very, very recently, in the grand scheme, that we’ve been consuming the products of agriculture: wheat; dairy; beans; and any foods that required more than the bare minimum of processing to make them edible. To greater or lesser degrees consuming these new foods isn’t good for us. As paleo nutritionist Ray Audette put it in his book Neanderthin (St. Martin’s Press, 2000), historically we’ve only consumed those items we could get if we were “naked with a sharp stick”: meat; certain vegetables; low glycemic; high fiber fruits; and certain nuts: hunter gatherer foods. Modern diseases are reactions to those foods that have only recently been added to our diets, gluten-containing foods being the most immediately obvious to this publication’s readership. Well, here’s one modern food that may deserve the same level of scrutiny as gluten-containing grains, even given its worship by what appears to be a totality of today’s nutritionists: our beloved chocolate. Now wait a minute. What kind of sadist would want to find fault with this giver of pleasure and apparent health panacea? Well, before we go there, let’s step back a moment to the naked with a sharp stick idea. Would chocolate, cocoa, cacao—or anything remotely similar—have been consumed by our paleo ancestors? No. Even in its purest commercial forms, it does require quite a deal of processing before it is edible: drying, fermenting, roasting, powdering, etc. Raw cacao proponents would disagree with this and, even though it is a tiny, tiny fraction of the market, there are raw, unpeeled, whole beans available for purchase. But let me get to a more important point. Chocolate, cocoa, cacao, in any form, was apparently discovered by native South Americans around 3000 years ago and didn’t make its way into the European diet until the 16th century, with widespread usage delayed until the Industrial Age a little more than 100 years ago. So if you’re a native of the tropical rainforests of South America, you’ve had a very short period of time for adaptation. If you don’t fit that description, you’ve had effectively zero time to adapt to this food. So what if it’s new? The so what is this: new foods—gluten-containing grains included—are almost always the cause of modern disease and as such deserve a closer look because of their novelty. Maybe chocolate’s ok to eat, maybe not. As mentioned above, it’s not “maybe” in current nutritional culture. Chocolate is lauded as the perfect health food. A simple search on Medscape.com yields more than 380 studies touting its benefits: they say it reduces blood pressure, decreases risk for pregnancy-induced hypertension, improves vasodilation, reduces platelet adhesion, reduces cholesterol, improves post-exercise workout recovery, improves insulin sensitivity, protects smokers’ hearts, improves endothelial function, even helps with diarrhea. And to top it off, it’s apparently a wonderful aphrodisiac. Turn on your television or radio, open a newspaper or log onto an Internet site and you’re sure to see a thousand more benefits claimed. We want this stuff to be good for us. Before we go on, I want to take another step back, change the subject entirely again, and talk about depression. Wikipedia defines it as “a mental disorder characterized by a pervasive low mood and loss of interest or pleasure in usual activities.” Ron Hoggan points out in his excellent article “Food Allergies and Depression,” that this condition is a “very common symptom of celiac disease,” and by extension gluten intolerance. Why did I suddenly change the subject to depression? Here’s why: a new study out of Australia (Gordon Parker, Isabella Parker, Heather Brotchie, Mood state effects of chocolate, Journal of Affective Disorders 92, 2006, 149-159) shows that chocolate may actually cause and/or deepen depression. The study shows a link between a worsening of depressive symptoms and chocolate consumption for those “emotional eaters” who are attempting to self-medicate. As the authors put it in the conclusion of the study: "When taken in response to a dysphoric state as an 'emotional eating' strategy it may provide some transient ”comforting” role but it is more likely to prolong rather than abort the dysphoric mood. It is not, as some would claim, an antidepressant." Now we already know that celiacs and the gluten intolerant are very prone to depression. We now know that chocolate may deepen depression. But, since there’s not a whole lot of data out there linking mood, chocolate, and gluten intolerance, I decided to do a personal experiment. Of course, the data is anecdotal, but I think informative and revealing. I regularly eat a diet free of gluten, diary, legumes, and artificial fats and had been very faithful to the regimen for a few months. For the purpose of the experiment I consumed one bar of Green & Blacks 70% Cocoa Content Dark. I quickly felt contentment, even mild euphoria. I was able to concentrate for quite a long time and actually did quite a bit of research for this article. But that evening I experienced a shallow, dream-filled sleep before awaking in a fog early the next morning. I had some gas, bloating, and was itchy with what I’ll call proto-hives. Within a few hours I had gained almost a pound of water weight and felt as if I had a hangover, mild depression. And, boy, was I irritable! I also noted mild shakes and muscular tension and some knots. Again, one guy = anecdotal evidence. But this doesn’t sound at all like a food that’s good for you! As a fellow gluten intolerant, I’d like to challenge you to the same experiment. Pick up a copy of a book I recommended in my last article, Loren Cordain’s The Paleo Diet (Wiley, 2002), and follow its dietary regimen for three weeks to eliminate from your system whatever non-paleo foods you might have floating around in your body. Then try a bar of quality dark chocolate and send me an email to tell me how it made you feel. Truth is, my reaction surprised me. But should it have? Chocolate is composed of foreign substances only very recently introduced into the human diet and apparently causes an immune system reaction similar to that caused by gluten. And, like the psychoactive effects felt when one ingests gluten, the initial euphoria and increased attentiveness caused by chocolate wears off relatively quickly and, for me at least (and I suspect for quite a few of the gluten intolerant) serious after effects remain. Maybe this isn’t the miracle food it’s purported to be.
- 6 comments
-
- celiac disease
- chocolate
- (and 3 more)
-
Celiac.com 03/13/2024 - Trichobezoar may sound like a term from a medical textbook, but for some individuals, it's a real and challenging condition. Imagine a solid mass forming in your stomach, composed of hair and food debris. This unusual condition, known as trichobezoar, is exceptionally rare, particularly in children. However, a recent case study has shed light on a unique connection between trichobezoar and celiac disease, emphasizing the importance of understanding these conditions and their treatment. A team of researchers present an unusual case involving the discovery of gastric trichobezoar in a 15-year-old girl who had undiagnosed celiac disease. The condition manifested after she experienced abdominal pain and pallor. Trichobezoar typically occurs in less than 1% of children, with most cases observed in young girls with psychiatric disorders. The condition arises from a compulsion to pull out hair (trichotillomania) and ingest it (trichophagia), leading to the accumulation of hair within the stomach lining. While trichobezoar is often associated with psychiatric conditions, its link to celiac disease is less common but noteworthy. In a recent case study, a 15-year-old girl presented with symptoms of trichobezoar, including abdominal pain, vomiting, and unexplained weight loss. Upon examination, doctors discovered a firm mass in her abdomen, along with signs of hair loss on her scalp. What made this case unique was the subsequent diagnosis of celiac disease, a condition characterized by an adverse reaction to gluten. Celiac disease is a chronic autoimmune disorder triggered by the ingestion of gluten, a protein found in wheat, barley, and rye. While the association between trichobezoar and celiac disease is unusual, researchers suggest two possible explanations. Firstly, deficiencies in iron and folic acid, common in individuals with celiac disease, may lead to behavioral disorders such as trichophagia. Secondly, celiac disease itself may directly contribute to the development of trichobezoar. Treatment for trichobezoar typically involves surgical removal of the mass, followed by psychological support to prevent recurrence. In cases associated with celiac disease, adopting a gluten-free diet is essential to manage symptoms and promote healing. This comprehensive approach addresses both the physical and psychological aspects of the condition, offering patients a chance at improved health and well-being. While trichobezoar and celiac disease are relatively rare on their own, their coexistence presents a unique challenge for patients and healthcare providers alike. By raising awareness of this uncommon association and emphasizing the importance of early detection and treatment, we can better support individuals living with these conditions. As medical research continues to advance, we hope to gain further insights into the complex relationship between trichobezoar, celiac disease, and other related disorders, ultimately improving outcomes for those affected. Read more at cureus.com The research team included Hassnae Tkak, Amal Hamami, Aziza Elouali, Nadir Miry, Amal Bennani, Houssain Benhaddou, Abdeladim Babakhouya, and Maria Rkain. They are variously affiliated with the Department of Pediatrics, University Hospital Mohamed V, Faculty of Medecine and Pharmacy, University Mohamed first, Oujda, MAR; the Department of Pediatrics, Mohammed VI University Hospital, Oujda, MAR; the Faculty of medicine and pharmacy of Oujda, Mohammed I University of Oujda, Morocco; Oujda, MAR; the Pathology department, Mohammed VI University Hospital; Oujda, MAR; the Histopathology department, Faculty of Medicine and Pharmacy, Oujda, MAR; the Department of Pediatric Surgery, Mohammed VI University Hospital, Oujda, MAR; the Service de Pédiatrie, CHU Mohammed VI, Oujda, Maroc. , Faculté de médecine et de pharmacie d'Oujda, Université Mohammed I d'Oujda, Maroc., CHU Mohammed Vi Oujda Morocco, Oujda, MAR; the Department of Pediatrics, Mohammed VI university hospital, Oujda, Morocco., Faculty of medicine and pharmacy of Oujda, Mohammed I University of Oujda, Morocco, Oujda, MAR; and the Pediatric Gastroenterology, CHU Mohammed Vi Oujda Morocco, Oujda, MAR.
-
- celiac disease
- connection
-
(and 3 more)
Tagged with:
-
Celiac.com 02/28/2024 - We get a lot of questions about what celiac disease trials and studies are going on, but there are so many, it can be hard to keep track. One easy source is the Mayo Clinic, which is at the forefront of a number of research trials, and studies to better understand, and treat celiac disease. Currently, there are more than a dozen exciting clinical trials underway, each focusing on different aspects of the celiac disease. One study aims to assess the effect of gluten on gut barrier function by using a novel gut permeability test developed by Mayo Clinic researchers. Another trial is evaluating the safety and tolerability of a potential new treatment, KAN-101, for celiac disease patients. Additionally, researchers are investigating the effectiveness and safety of numerous compounds for relieving symptoms in adult celiac disease patients. These trials represent important steps forward in advancing our understanding of celiac disease and developing new therapies to improve the lives of those affected by this condition. Celiac disease trials and studies currently underway at the Mayo Clinic facilities include: Gut Permeability Assessment in Celiac and Gluten Sensitive Children Rochester, MN This study will assess the effect of gluten on gut barrier function. Investigators at the Mayo Clinic have developed a new gut permeability test using rhamnose (sugar & water solution), and are hoping to prove its effectiveness in a clinical setting. A Study to Assess the Safety and Tolerability of Single and Multiple Doses of KAN-101 in Celiac Disease Patients Rochester, MN The purpose of this study is to assess the safety and tolerable of single and multiple doses of KAN-101 in patients with Celiac disease. A Study to Evaluate the Effectiveness and Safety of Larazotide Acetate for the Relief of celiac disease Symptoms Rochester, MN The purpose of this study is to assess the effectiveness and safety of larazotide acetate versus placebo for the relief of persistent symptoms in adult celiac disease patients. Study of the Safety, Tolerability, Pharmacokinetics and Biomarker of DONQ52 in Celiac Disease Patients Rochester, MN The purpose of this study is to evaluate the safety and tolerability of single and multiple doses of DONQ52 in celiac disease patients and to evaluate the safety and tolerability of DONQ52 in celiac disease patients in the presence of gluten after multiple doses of DONQ52. Furthermore, to characterize the DONQ52 PK profile following single and multiple subcutaneous (SC) dose(s) in celiac disease patients and to investigate the immunogenicity of DONQ52. A Study of the Response to and Changes in Intestinal Permeability 4 hours after a Gluten Challenge in Subjects with Celiac Disease and Non Celiac Gluten Sensitivity Rochester, MN The purpose of this study is to identify mediators—innate immune system and intestinal permeability—of acute onset gastrointestinal symptoms after gluten ingestion in subjects with celiac disease and non-celiac gluten sensitivity. Gut Permeability in Environmental Enteropathy Rochester, MN The goal of this project, to develop a simple and sensitive test of small bowel permeability, will improve the scientific and public health understanding of environmental enteropathy and guide development of preventative and treatment modalities such as clean water and sanitation. Mucosal Interactions in Celiac Disease Rochester, MN To obtain biopsies and blood from subjects not previously known to have celiac disease who are undergoing duodenal biopsies for clinical indications. The subjects will have no prior diagnosis of celiac disease and are eating a gluten-containing diet. The biopsies will be treated “in vitro” with enzymatic digests of gluten derived from bread made from different species of wheat, the auto-antigen tTg, cytokines, or other proteins. A Study to Evaluate the Safety, Effectiveness, and Tolerability of Latiglutenase to Treat Patients with Well-Controlled Celiac Disease Rochester, MN The purpose of this study is to demonstrate a positive correlation of histologic protection (biological signature) and symptom protection (clinical outcome) for latiglutenase treatment versus placebo in Celiac Disease (celiac disease) patients undergoing a deliberate gluten challenge. A Study of the Safety, Pharmacodynamics, Effectiveness, and PK of TIMP-GLIA in Subjects with Celiac Disease Rochester, MN The purpose of this study is to evaluate participants for immune responses and histological changes in the small bowel following 2 doses of TIMP-GLIA or placebo and a 14-day oral gluten challenge. Dose-Ranging Study of the Efficacy and Safety of TAK-101 for Prevention of Gluten-Specific T Cell Activation in Participants With Celiac Disease on a Gluten-Free Diet Rochester, MN The purpose of this study is to compare the number of baseline interferon-gamma (IFN-γ) spot forming units (SFUs) to the number of IFN-γ SFUs after a 6-day oral gluten challenge among HLA DQ2–positive subjects treated with TAK-101 versus placebo. A Study of Simvastatin Metabolism as a Test for Celiac Disease Activity Rochester, MN The purpose of the study is to assess the connection between simvastatin metabolism by an enzyme that varies based on the state of the small intestine in treated celiac disease. Antibody Treatment for Advanced Celiac Disease Rochester, MN Celiac disease is a condition where the immune system attacks the cells of the small intestine. The intestine becomes inflamed and cannot digest food properly. The disease most often causes a reaction to foods that contain gluten. Most people can treat celiac disease with a gluten-free diet. However, some people have digestion problems even on a gluten-free diet. Researchers want to try a new antibody therapy for celiac disease. The treatment may block the immune reaction that causes the disease. They will test this antibody in people who have celiac disease that has not responded to a gluten-free diet. Prospective, Randomized, Double-Blind, Placebo-Controlled, Crossover Study in Symptomatic Celiac Disease Patients Rochester, MN This is a phase 2b, multi-center, prospective, randomized, double-blind, placebo-controlled, crossover study in symptomatic celiac disease patients attempting a gluten free diet (GFD) for at least one year prior to screening. A Study of TAK-062 in Treatment of Active Celiac Disease in Participants Attempting a Gluten-Free Diet Rochester, MN; Scottsdale/Phoenix, AZ The purpose of this study is to see how TAK-062 works to reduce celiac-related symptoms and improve small intestinal damage due to gluten exposure, in participants with celiac disease (celiac disease) attempting to maintain a gluten-free diet (GFD) in treated participants versus placebo controls. A Study of the Safety, Effectiveness and Tolerability of Nexvax-2 in Patients with Celiac Disease (celiac disease) Rochester, MN The purpose of this study is to evaluate the human leukocyte antigen (HLA)-DQ 2.5+ in adults with celiac disease (celiac disease). Evaluation of the Efficacy and Safety of ALV003 in Symptomatic in Celiac Disease Patients Scottsdale/Phoenix, AZ; Jacksonville, FL; Rochester, MN To determine the effects of 12 weeks administration of different dose levels of ALV003 on the mucosal lining of the small intestine and symptoms in celiac disease patients. Minimal Risk Registry of Endoscopic Image and Pathology Correlation for Fujiflim Jacksonville, FL; Rochester, MN The purpose of this study is to see if advanced endoscopic imaging may be helpful to accurately distinguish pathological tissue from normal tissue and guide therapy of endoscopically identified pathology. Functional Gastrointestinal Disease, Celiac Disease, and Non-celiac Gluten Sensitivity in an Olmsted County Cohort Rochester, MN The aim of this study is to the number of individuals following a gluten-free diet and possible reasons including symptoms of non-celiac gluten sensitivity and functional gastrointestinal diseases (FGIDs). lso assess Diagnoses and lab values associated with celiac disease, NCGS, and FGIDs will also be assessed, as well as past GI survey data and medical record data available through the Rochester Epidemiology Project. Stay tuned for updates on the progress of these and other related studies! Read more at Mayo.edu
- 3 comments
-
- celiac disease
- mayo clinic
-
(and 3 more)
Tagged with:
-
Celiac.com 03/04/2024 - Chugai Pharmaceutical Co., Ltd. has announced significant strides in the development of a potential treatment for celiac disease with their novel multi-specific antibody, DONQ52. The company recently announced that the non-clinical research results on DONQ52 have been published in Nature Communications, a prestigious multidisciplinary scientific journal. This milestone represents a significant step forward in the quest to find effective therapies for celiac disease, a condition currently without approved treatment options. DONQ52, discovered by Chugai, has shown promise in selectively inhibiting the immune response to gluten, a key component in the pathology of celiac disease. Through advanced antibody engineering technologies, DONQ52 was designed to target and neutralize multiple gluten peptides in complex with HLA-DQ2.5, a genetic marker strongly associated with celiac disease. The research findings published in Nature Communications outline the potential of DONQ52 to effectively inhibit gluten-dependent T-cell activation, a crucial step in the immune response cascade that leads to intestinal damage in celiac disease. Notably, DONQ52 demonstrated broad and selective recognition of over 25 distinct pathogenic gluten peptides, indicating its versatility and potential as a therapeutic agent. The Goal is to Develop a Therapy that can Provide Relief to Individuals Living with Celiac Disease Dr. Osamu Okuda, President and CEO of Chugai, expressed optimism about the future of DONQ52 in celiac disease treatment. He highlighted the ongoing Phase I clinical study, which aims to assess the safety and efficacy of DONQ52 in patients with celiac disease. The ultimate goal is to develop a therapy that can provide relief to individuals living with celiac disease, addressing an unmet medical need in the field. “We are very pleased to announce that that the results of basic research on a multi-specific antibody DONQ52 discovered by our company have been published in Nature Communications. Although technical hurdles have prevented practical use to date, our non-clinical study shows that specific and broad inhibition of HLA-T cell interactions is a useful therapeutical approach for celiac disease,” said Dr. Okuda. As the Phase I study progresses, Chugai remains committed to advancing the development of DONQ52 and leveraging their expertise in antibody engineering to explore new possibilities in celiac disease therapy. With continued research and innovation, DONQ52 has the potential to offer hope and improved quality of life for those affected by celiac disease. Stay tune for more on this and related stories. Read more at chugai-pharm.co.jp
- 5 comments
-
- celiac disease
- chugai
-
(and 3 more)
Tagged with:
-
Celiac.com 03/07/2024 - A recent study of mice has shed light on the potential effects of chronic oral exposure to silicon dioxide (fg-SiO2), a common food additive, on food sensitivities and immune responses. This research is particularly relevant to individuals with celiac disease and other food sensitivities. Silicon dioxide, a versatile additive, plays a vital role in maintaining the quality and integrity of numerous dry and powdered food products. It can be found in ingredients of more than 2,600 processed foods worldwide, from savory soups to aromatic spices, and even infant formula. Its presence ensures that food items remain free-flowing and devoid of unsightly lumps, and it isn't always included on ingredient lists. The study, led by a team of researchers, aimed to understand how exposure to silicon dioxide, in the form of food-grade silicon dioxide (fg-SiO2), might influence the immune system's response to food antigens. Using mouse models, the researchers investigated the effects of silicon dioxide on oral tolerance (OT) induction and gluten immunopathology. The research team included Bruno Lamas, Natalia Martins Breyner,, Yann Malaisé, Mark Wulczynski, Heather J. Galipeau, Eric Gaultier, Christel Cartier, Elena F. Verdu, and Eric Houdeau. They are variously affiliated with the Toxalim (Research Centre in Food Toxicology), Team Endocrinology and Toxicology of Intestinal Barrier, INRAE/ENVT/Paul Sabatier University, Toulouse, France; and the Farncombe Family Digestive Health Research Institute, Department of Medicine, McMaster University, Hamilton, Ontario, Canada. Their findings revealed that exposure to silicon dioxide led to changes in immune cell function and cytokine production in the intestines. Specifically, cells from the mesenteric lymph nodes (MLNs) showed decreased proliferation and reduced secretion of key regulatory cytokines involved in OT, such as interleukin 10 (IL-10) and transforming growth factor beta (TGF-β). Furthermore, mice exposed to silicon dioxide exhibited signs of intestinal inflammation, including increased levels of fecal lipocalin-2 (Lcn-2) and interferon gamma (IFN-γ). This inflammation was associated with a breakdown of oral tolerance and alterations in immune cell populations in the intestines. Chronic Oral Exposure to Silicon Dioxide May Worsen Food Sensitivities In a mouse model of gluten-induced immunopathology, chronic exposure to silicon dioxide exacerbated intestinal damage and inflammation. These effects were observed through changes in villus-to-crypt ratio and increased infiltration of inflammatory T cells. Overall, the study suggests that chronic oral exposure to silicon dioxide may disrupt oral tolerance induction and worsen food sensitivities, particularly in individuals predisposed to conditions like celiac disease. While the study was conducted in mice, its findings underscore the need for further research to explore the potential link between silicon dioxide exposure and food sensitivities in humans. In conclusion, people with celiac disease and other food sensitivities may benefit from understanding the potential impact of food additives like silicon dioxide on their immune responses. Further investigation into this area could provide valuable insights into strategies for managing and mitigating food sensitivities in affected individuals. Read more at Environmental Health Perspectives Journal
-
- celiac disease
- food
- (and 6 more)
-
Celiac.com 02/27/2024 - For people with celiac disease, finding gluten-free alternatives to traditional wheat flour has been a challenge. That is until now. Enter Bread Free, a Spanish biotech start-up breaking barriers with its groundbreaking creation: gluten-free wheat flour. But how does it work, and what does it mean for those of us who need to avoid gluten? Let's dig in. A Game-Changer for Those with Celiac Disease Bread Free has pioneered the development of gluten-free wheat flour, making them the first company to achieve this feat. Traditionally, wheat flour is off-limits for those with celiac disease due to its gluten content. However, Bread Free's innovative approach removes the gluten while preserving the flour's essential qualities. Benefits of Bread Free Flour Juan Garrido, co-founder of Bread Free, explains that their product maintains all the organoleptic properties of conventional wheat flour. Translation? It looks, feels, and tastes like the real deal. This is fantastic news for individuals with celiac disease who miss the taste and texture of wheat-based products. Why It Matters Celiac disease is a serious autoimmune condition triggered by the consumption of gluten, a protein found in wheat, barley, and rye. Symptoms can range from mild discomfort to severe digestive issues and nutrient deficiencies. With approximately 0.7% of the EU population affected by celiac disease, finding safe and affordable gluten-free options is crucial. Addressing Price Concerns One of the main challenges for individuals with celiac disease is the high cost of gluten-free products. Shortages of ingredients like rice flour have further strained prices in recent years. However, Bread Free's manufacturing process, similar to that of ordinary wheat flour, helps mitigate these price pressures without compromising quality or nutrition. Translation: The price should be reasonable. Nutritional Quality Despite concerns about the nutritional quality of gluten-free products, Bread Free flour maintains the nutritional benefits of wheat. This means individuals can still enjoy the dietary advantages of wheat flour while adhering to a gluten-free diet. Is It Safe for Celiacs? The company touts the product as gluten-free. If the final product is under 20ppm gluten, then it's likely safe for people with celiac disease. Utilizing Artificial Intelligence and Biotechnology to Remove Gluten, Not Genetic Modification Bread Free utilizes biotechnology, not genetic modification, to remove gluten from their flour. By leveraging artificial intelligence (AI), they optimize their production process to ensure product safety and efficiency. The result? A gluten-free wheat flour that meets food regulations and exceeds expectations. Looking Ahead Bread Free plans to launch its product first in Spain and then expand throughout Europe. This exciting development promises to revolutionize the gluten-free market and provide new options for individuals with celiac disease. Bread Free's gluten-free wheat flour offers hope and opportunity for those living with celiac disease. With its ability to deliver the taste, texture, and nutrition of traditional wheat flour without the harmful effects of gluten, it represents a significant step forward in gluten-free innovation. Stay tuned for more updates as Bread Free makes its mark on the world of gluten-free baking!
- 13 comments
-
- biotechnology
- celiac disease
-
(and 3 more)
Tagged with:
-
Celiac.com 02/24/2024 - A recent poll conducted by Celiac.com shed light on various aspects of celiac disease knowledge and experiences among respondents. However, one finding stands out starkly: 18% of respondents admitted to cheating on their gluten-free diet. This revelation underscores the critical importance of emphasizing the necessity of strict dietary compliance for individuals with celiac disease. Cheating on a gluten-free diet can have serious consequences, ranging from uncomfortable symptoms to long-term health complications such as intestinal damage, malnutrition, and an increased risk of other autoimmune conditions. In this article, we explore the implications of this poll result and why maintaining a gluten-free diet is paramount for the health and well-being of individuals living with celiac disease. Question 1: Celiac disease is an autoimmune disorder. Celiac.com's poll revealed that 100% of respondents correctly identified this statement as true. This is an essential fact about celiac disease. When individuals with celiac disease consume gluten, their immune system mistakenly attacks the lining of the small intestine, leading to various symptoms and potential long-term complications. The autoimmune nature of the condition underscores the seriousness of adhering to a strict gluten-free diet to manage symptoms and prevent further damage. Question 2: Celiac disease is primarily a genetic condition. While 58% of respondents recognized this statement as true, it's crucial to emphasize that genetics play a significant role in celiac disease. Having certain genetic markers, such as the HLA-DQ2 and HLA-DQ8 genes, increases the likelihood of developing the condition. However, genetics alone do not determine who will develop celiac disease, as environmental factors also play a role. Question 3: Cross-contamination with gluten can trigger symptoms in individuals with celiac disease. Nearly all respondents (98%) correctly identified this statement as true. Cross-contamination occurs when gluten-free foods come into contact with gluten-containing products or surfaces, leading to the inadvertent ingestion of gluten. Even trace amounts of gluten can provoke symptoms in individuals with celiac disease, highlighting the importance of strict dietary adherence and careful food preparation practices. Question 4: What is the name of the protein in wheat that triggers the immune response in celiac disease? The majority of respondents (76%) correctly selected gliadin as the protein in wheat responsible for triggering the immune response in celiac disease. Understanding the specific components of gluten, such as gliadin, is crucial for individuals with celiac disease to effectively identify and avoid gluten-containing foods. Question 5: Celiac disease is more common in people of European descent. A significant majority of respondents (68%) correctly identified this statement as true. While celiac disease can affect individuals of any ethnicity, it is more prevalent among those of European descent. This highlights the importance of considering genetic predisposition when assessing the risk of celiac disease in different populations. Question 6: Dermatitis herpetiformis is a skin manifestation associated with celiac disease. A vast majority of respondents (92%) correctly recognized this statement as true. Dermatitis herpetiformis is a chronic, blistering skin rash that is strongly associated with celiac disease. It is caused by the same immune response to gluten that damages the intestinal lining in individuals with celiac disease. Question 7: What percentage of people with celiac disease may go undiagnosed? 28% of respondents correctly identified 50% as the percentage of people with celiac disease who may go undiagnosed. This statistic sheds light on a concerning reality within the celiac disease community. Despite increased awareness and diagnostic tools, a significant portion of individuals with celiac disease remain undiagnosed. There are several factors contributing to this high rate of underdiagnosis. Firstly, the symptoms of celiac disease can vary widely and overlap with those of other gastrointestinal disorders, making it challenging for healthcare providers to recognize the condition. Additionally, some individuals with celiac disease may experience mild or atypical symptoms, leading them to dismiss their symptoms or attribute them to other causes. Cultural and societal factors may also play a role, as misconceptions about celiac disease and gluten sensitivity persist, leading to delays in seeking medical attention or reluctance to undergo testing. Furthermore, lack of access to healthcare, particularly in underserved communities, can further exacerbate the problem of underdiagnosis. Addressing these barriers to diagnosis and increasing awareness among both healthcare providers and the general public are crucial steps in improving the identification and management of celiac disease. Question 8: Medications can sometimes contain gluten as an inactive ingredient. An overwhelming majority of respondents (96%) correctly identified this statement as true. It's essential for individuals with celiac disease to carefully check the ingredients of medications, as gluten can sometimes be present in inactive ingredients or as a coating on tablets. Question 9: The terms "wheat-free" and "gluten-free" are interchangeable. While 91% of respondents correctly identified this statement as false, it's worth emphasizing the important distinction between "wheat-free" and "gluten-free." While a wheat-free diet excludes wheat and its derivatives, a gluten-free diet eliminates all sources of gluten, including wheat, barley, and rye. Question 10: Which nutrient deficiency is commonly associated with untreated celiac disease? A significant majority of respondents (70%) correctly selected vitamin D deficiency as a common nutritional consequence of untreated celiac disease. Malabsorption of nutrients due to damage to the intestinal lining can lead to deficiencies in various vitamins and minerals, highlighting the importance of proper nutritional management in individuals with celiac disease. Question 11: Celiac disease can affect the neurological system, leading to issues such as gluten ataxia. An overwhelming majority of respondents (96%) correctly identified this statement as true. Neurological manifestations of celiac disease, such as gluten ataxia, underscore the systemic nature of the condition and the potential for diverse symptoms beyond gastrointestinal issues. Question 12: What is the most reliable treatment for celiac disease? An overwhelming majority of respondents (98%) correctly selected a gluten-free diet as the most reliable treatment for celiac disease. Strict adherence to a gluten-free diet is essential for managing symptoms, promoting intestinal healing, and preventing long-term complications associated with celiac disease. Question 13: Celiac disease has been linked to an increased risk of osteoporosis. A vast majority of respondents (90%) correctly identified this statement as true. Malabsorption of calcium and vitamin D, along with chronic inflammation associated with celiac disease, can contribute to decreased bone density and an increased risk of osteoporosis. Question 14: Quinoa is a grain that contains gluten. 86% of respondents correctly identified this statement as false. Quinoa is a gluten-free grain that can be safely consumed by individuals with celiac disease as part of a gluten-free diet. Question 15: What is the medical term for the biopsy procedure used to diagnose celiac disease? The majority of respondents (79%) correctly selected endoscopy as the medical term for the biopsy procedure used to diagnose celiac disease. During an endoscopy, a small tissue sample is taken from the small intestine to assess for characteristic changes associated with celiac disease. Question 16: Do you cheat on your gluten-free diet? This question delves into a significant issue within the celiac disease community: adherence to a gluten-free diet. While 82% of respondents reported not cheating on their gluten-free diet, 18% admitted to doing so. This highlights the challenges that individuals with celiac disease may face in maintaining strict dietary compliance and underscores the need for ongoing education, support, and access to gluten-free resources to help individuals effectively manage their condition and prevent potential health complications. Additionally, it's worth noting the significant advancements in gluten-free food options in recent years. With the increasing awareness of celiac disease and gluten sensitivity, there has been a proliferation of gluten-free products available in grocery stores and online retailers. Moreover, many whole foods are naturally gluten-free, including fruits, vegetables, meats, fish, dairy, and gluten-free grains like quinoa and rice. Restaurants have also responded to the demand for gluten-free options, with many establishments now offering dedicated gluten-free menus or clearly labeling gluten-free choices on their regular menus. With such wide availability of gluten-free alternatives, individuals with celiac disease have more options than ever to enjoy delicious and safe meals without the need to compromise their dietary restrictions. This accessibility underscores the importance of making informed choices and prioritizing health by adhering to a strict gluten-free diet. In 2002 Celiac.com ran a similar poll question where ~42% of people reported cheating regularly on their gluten-free diets, so in comparison to 22 years ago there has been a significant decrease in the number of people who cheat on their gluten-free diets. In conclusion, Celiac.com's latest poll provides valuable insights into the knowledge, experiences, and challenges faced by individuals living with celiac disease. From understanding the autoimmune nature of the condition to recognizing the importance of dietary adherence and vigilance in avoiding gluten, these findings underscore the multifaceted nature of managing celiac disease and the ongoing need for education, support, and advocacy within the celiac disease community.
- 7 comments
-
- celiac disease
- cheat
-
(and 6 more)
Tagged with:
-
Celiac.com 12/08/2018 - Recently CNN published an article entitled “Will a Gluten Free Diet Improve Your Health?” Honestly there were a lot of plus-points to this article. But unfortunately the negatives could very well outweigh them if you’re considering, or are new to, the gluten-free diet. Let’s review the positives and negatives as they appear in the article: 1. Dr Leffler from Harvard Medical School was quoted as saying that: “Gluten is fairly indigestible in all people.” “There’s probably some kind of gluten intolerance in all of us.” Bravo! I was very excited to read this remark. Although I often promote this information, I haven’t heard it from others aside from Dr. Fasano. The fact that humans can’t properly digest gluten is an important truth that should be better known and more widely taught. 2. Experts now believe that celiac disease represents just one extreme of a broad spectrum of gluten intolerance that includes millions of people. It can sometimes be interesting when unnamed “experts” are quoted, but in this case I agree. I’ve often written about my belief that celiac disease to gluten sensitivity is likely one spectrum. The fact that those with gluten sensitivity don’t undergo the outright destruction of the small intestine as in the case of celiac disease, in no way puts gluten sensitivity in a less serious category. It’s a “different” reaction but no less serious. 3. They go on to state that people with celiac disease and gluten sensitivity usually have stomach aches, gas, and diarrhea -- as do people with IBS. “Usually” is not the case and it would give someone without digestive complaints a false sense that they do not have gluten intolerance. In fact, according to research, for every person with celiac disease who experiences digestive symptoms, there are eight without digestive complaints. This is why, all too often, people continue to live with migraines, depression, infertility, skin problems, obesity and autoimmune disease that is gluten related but the gluten connection remains undiagnosed because they have no digestive complaints. Let’s not kid ourselves. We’re only diagnosing, at best, seven percent of the celiacs in our country. In our medically advanced society, missing over ninety percent of those suffering with the most common lifelong disorder in the US and Europe, is beyond pitiful. Unfortunately, it is statements such as the above, limiting our focus to digestive complaints that are partly to blame for our poor rate of diagnosis. 4. Gluten sensitivity, on the other hand, is a gray area that “lacks any defining medical tests,” Leffler says. People who fall into this group exhibit the classic symptoms of celiac disease yet have no detectable intestinal damage, and test negative for certain key antibodies (though in some cases they may have elevated levels of others). The issue here might be “medical tests” and Dr. Leffler may not know about the gluten sensitivity tests that are available. However, they are available and they have recently taken a nice jump in sensitivity due to a new lab in the US (Cyrex Labs – again, I have no affiliation with this lab). I also take umbrage to the reference to the lab tests as almost an afterthought in parentheses. The truth lies within those parentheses – gluten sensitive individuals do show elevation of key antibodies that are different than those seen in celiac disease. Does that make those elevations somehow less important? Of course not! They are just different. 5. “A recent study by Fasano and his colleagues offers some clues about what gluten sensitivity is, and how it differs from celiac disease. Although they show no signs of erosion or other damage, the study found, the intestines of gluten-sensitive patients contain proteins that contribute to a harmful immune response, one that resembles -- but is distinct from -- the process underlying celiac disease. “ This is a very good point. First, Dr Fasano is spending his time researching gluten sensitivity. This is not something we would have seen several years ago. His latest research showed that the immune system DOES create a harmful immune response in the intestines of those suffering from gluten sensitivity. Is it the same response as that seen in celiacs? No. But we didn’t expect that it would be. We know that small intestinal erosion doesn’t happen in the gluten sensitive patient. What’s earth shattering about this research finding is that it completely validates what I and other clinicians like me have been saying for several years – gluten sensitivity is the adverse effect of the body’s immune system having a deleterious reaction to gluten. This research proves that point. 6. “Recommendations for people with gluten sensitivity aren’t as clear-cut. Unlike celiac disease, gluten sensitivity hasn’t been linked to intestine damage and long-term health problems, so some experts say that people on the less severe end of the spectrum should feel comfortable eating as much gluten as they can handle without feeling sick.” Ah, so easy to write, so hard to take back or explain. This is a dangerous couple of sentences. Let’s dissect: They join “intestine damage” with “long-term health problems” as if it were impossible to have a long-term health problem without intestinal damage. Nothing could be further from the truth! I have many, many patients with gluten sensitivity, and therefore none of the intestinal destruction seen with celiac disease, who would beg to differ as regards long-term health problems being associated with gluten sensitivity, not just celiac disease. These patients have seen their serious long-term health problems resolve as a result of eliminating gluten from their diet. And they did not have celiac disease. Is schizophrenia a health problem? What about migraines? How about eczema? Is infertility a health problem when you’re trying to get pregnant? What about depression? I could go on and on. And it’s not just my opinion or my patients’ opinions. This is very well substantiated by research. You cannot “feel” damage and inflammation to certain organs of your body. In fact, autoimmune disease markers can be present for well over a decade before the first symptoms show themselves. Should we wait? Is that smart? Let’s continue: In the last sentence of point #6 above, we come across those unnamed “experts” I was referring to earlier. I would really like to know names on this one. Perhaps they were misquoted, or misunderstood. The truth of the matter is that gluten is not called the “great masquerader” because it creates overt symptoms all the time, quite the contrary. That is why one never is quite sure what symptoms will improve until one actually embarks on a gluten-free diet. In fact it was this realization that caused us to write the book “The Gluten Effect” two years ago. There was little appreciation at that time of all the effects that gluten could create in the non-celiac individual, which is why we were compelled to share our experiences. 7. “Some people can be exquisitely sensitive and have to be as strict as people with celiac disease, while others can eat a pizza,” Fasano says. [he was referring to gluten sensitivity] You might imagine that a newly diagnosed individual might very well read this sentence and be keeping their fingers crossed that they might be one of the lucky ones who could eat the pizza. I am a huge fan of Dr. Fasano’s and to give this quote the benefit of the doubt I’m going to give you my interpretation. I have patients who have gone out and eaten pizza and “felt fine”. In fact they seemed to feel so “fine” that they did it again. Did they ultimately end up fine? No, they did not. They found themselves days, weeks or months later quite ill, not only with old symptoms returning but often with new ones as well. What, then, could Dr. Fasano have meant by his comment? I believe that he was trying to make a point about the difference between a celiac and a person with gluten sensitivity. A celiac could have a miniscule amount of a crouton drop into their salad and be very ill almost immediately, while a person with gluten sensitivity would not necessarily have such an acute reaction. But to take that to mean that it is in some way “fine” or healthy for them to eat gluten is definitely not the case and I don’t believe that’s what Dr. Fasano meant. 8. “If you suspect your body can’t tolerate gluten, the first thing you should do is get tested for celiac disease. If the test comes back negative, try a gluten-free diet for a week to see if you feel better, Leffler says.” The cells in the intestine take about a month to turn over and renew themselves. A week on a gluten-free diet is not sufficient, in the main, to determine whether one has a problem. A month of absolutely no gluten is a more appropriate standard. With that said, some people do feel better almost immediately but I wouldn’t want to miss those who take several weeks to feel the change by not pointing out the 30 day recommendation. 9. Finally, ending on an up note: “People with gluten sensitivity who don’t respond this way [meaning feeling ill immediately] aren’t necessarily in the clear, however. Experts like Marlisa Brown, a registered dietitian and author worry that gluten could have long-term negative consequences that just haven’t been identified yet.” As we’ve been discussing many of the consequences are known and they are serious. But I do agree with her that just because you don’t feel sick right away is no reason to eat gluten when you are sensitive to it. I hope this helps clarify this recent article and gives you and those you care about the support you need to continue your gluten-free lifestyle. It is worth it, I promise! References: www.CyrexLabs.com www.Enterolab.com Alimentary Pharmacology & Therapeutics. 2009 Jun 15;29(12):1299-308. Epub 2009 Mar 3.
- 3 comments
-
- celiac disease
- cheat
-
(and 2 more)
Tagged with:
-
Hey there! Before I get into the details, I just wanted to start off by saying how grateful I am to have come across this website. It is so comforting to know that there’s a community of people out there who understand the difficulties of celiac disease first hand. So thank you all for sharing your experiences. Below I’ve listed three main issues I’ve started seeing and I am seeking some advice. For context: I’ve been following an 100% gluten free diet for about 6 months now, but just started noticing these symptoms within the last couple of weeks or so. I’m not sure if anyone else has experienced these problems too but just thought it wouldn’t hurt to reach out. LACK OF APPETITE: Has anyone else experienced a lack of appetite after following a strict gluten free diet? I’ve personally always had a great relationship with food and eating regularly. But ever since following a gluten free diet, I haven’t been eating much, or anything at all for that matter. Sometimes I won’t even realize that I haven’t eaten anything by dinner time. I genuinely don’t feel hungry. Can others relate? Any tips? INSOMNIA: It just these last couple of weeks where I have been experiencing the worst insomnia. I can’t sleep at all anymore. I’m lucky if I fall asleep around 2-3 o’clock. It’s been so incredibly frustrating for me to deal with. I just feel so lost with this. I’ve tried googling and to my understanding, no gluten in my diet makes it harder to get tired? Idk. Feel free to correct me on that one. I’ve tried sleeping pills but I really want to avoid relying on them if possible. I have a vitamin b-12 deficiency, and have read that others have found that taking b-12 before bed has improved sleep. Im willing to try anything at this point, so I’ll see if it works. Haha as I’m writing this at 2:30 am. NAUSEA: I’ve noticed as I’m lying down to sleep I feel slightly nauseous. I just have to sit up which makes it harder to sleep. Disclaimer, i haven’t actually thrown up yet. It’s weird, it doesn’t reach or get to that point really, but I’ll still feel nauseous. Mainly at night but sometimes during the day. Has anyone else experienced this? If you have any advice please share.
- 4 replies
-
- appetite
- celiac disease
-
(and 6 more)
Tagged with:
-
Celiac.com 02/03/2018 - People with celiac disease need to avoid consuming products that contain gluten, including those made with wheat, rye and barley. So, what about Annatto color? You may know annatto color as one of those common ingredients in food. Annatto color is used to color yellow or orange cheese. To make matters more confusing, annatto color still appears on some old, outdated lists as not gluten-free, and unsafe. Many of these listings of supposedly problematic ingredients were based "solely on guesses and suspicions." As such, they commonly promoted incorrect or incomplete information. Annatto color is derived from the seeds of the Achiote, also known as the Lipstick tree (Bixa orellana), it is often used in cheese, but also in many other orange-colored foods. Achiote seeds do not contain gluten. Annatto color is gluten-free and generally safe for people with celiac disease on a gluten-free diet. Some people with celiac disease do claim sensitivity to annatto color, but they are likely not reacting to gluten. Annatto color appears on Celiac.com's list of safe and gluten-free foods. Here's a helpful bit by a member Celiac.com's gluten-free forum, named Richard: "Annatto is gluten-free. Without question. I suspect your info came from CSA/USA, which for years put out bad information about ingredients based solely on guesses and suspicions." For years, some celiac organizations warned members that annatto might cause gluten-like reactions. They cited concerns about the "processing of the seed into a colorant that causes concern as it appears to use alcohol in the process. There is also suspicion that caramel color may be included in the annatto colorant. Anecdotal evidence has some celiacs reacting to foods with annatto color in them but this may be a non-celiac reaction to the annatto itself." So, the shorthand is that annatto coloring is gluten-free and generally safe for people with celiac disease. Folks who cannot tolerate annatto coloring are not reacting to gluten, but to something else.
- 9 comments
-
- annatto color
- celiac disease
-
(and 2 more)
Tagged with:
-
Celiac.com 02/19/2024 - A recent study presented at the 2023 annual meeting of the American College of Gastroenterology has raised concerns about the increasing incidence of enteropathy-associated T-cell lymphoma (EATL) – a rare and aggressive form of T-cell, non-Hodgkin lymphoma. This alarming trend has prompted researchers to explore the possible connection between EATL and celiac disease, shedding light on the risks faced by individuals with this autoimmune condition. Lead investigator Dr. Isabel Hujoel, Clinic Director of the Celiac Disease Center at UW Medical Center, Seattle, highlighted the strong association between EATL and celiac disease. While EATL is rare, most cases are observed in patients with celiac disease, suggesting a potential link between the two conditions. The study, utilizing data from the Surveillance, Epidemiology, and End Results (SEER) program database, identified 463 cases of EATL between 2000 and 2020, with an age-adjusted incidence rate of 0.014 per 100,000 people. Alarmingly, the incidence of EATL increased by 2.58% annually over this 20-year period. Despite advancements in medical treatment, the prognosis for EATL remains poor, with a median survival of approximately six months. Findings from the study revealed that most cases were treated with a combination of surgery and chemotherapy. However, survival outcomes did not improve over the study period, underscoring the urgent need for more effective treatment strategies. Dr. Sophia Dar, a gastroenterology fellow at Southern Illinois University School of Medicine, emphasized the importance of early detection and treatment. While chemotherapy showed promising results, the overall mortality rate remained high, highlighting the challenges in managing this aggressive cancer. Researchers emphasized the need for further investigation into the factors contributing to the high mortality rate associated with EATL. Understanding these factors could pave the way for more efficient treatment plans and improved outcomes for patients. Debra Silberg, MD, PhD, Chief Scientific Officer of the nonprofit Beyond Celiac, emphasized the rarity of EATL and the need for targeted screening. Screening for EATL should be considered in cases of refractory celiac disease or when there is suspicion of complications related to celiac disease. The rise in cases of EATL serves as a sobering reminder of the potential complications associated with celiac disease. Heightened awareness, early detection, and improved treatment options are crucial in addressing this rare but deadly cancer among individuals with celiac disease. Read more at gastroendonews.com
- 11 comments
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8-M):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8-M):