-
Welcome to Celiac.com!
You have found your celiac tribe! Join us and ask questions in our forum, share your story, and connect with others.
-
Celiac.com Sponsor (A1):
Celiac.com Sponsor (A1-M):
-
Get Celiac.com Updates:Support Celiac.com!
Search the Community
Showing results for tags 'diagnose'.
-
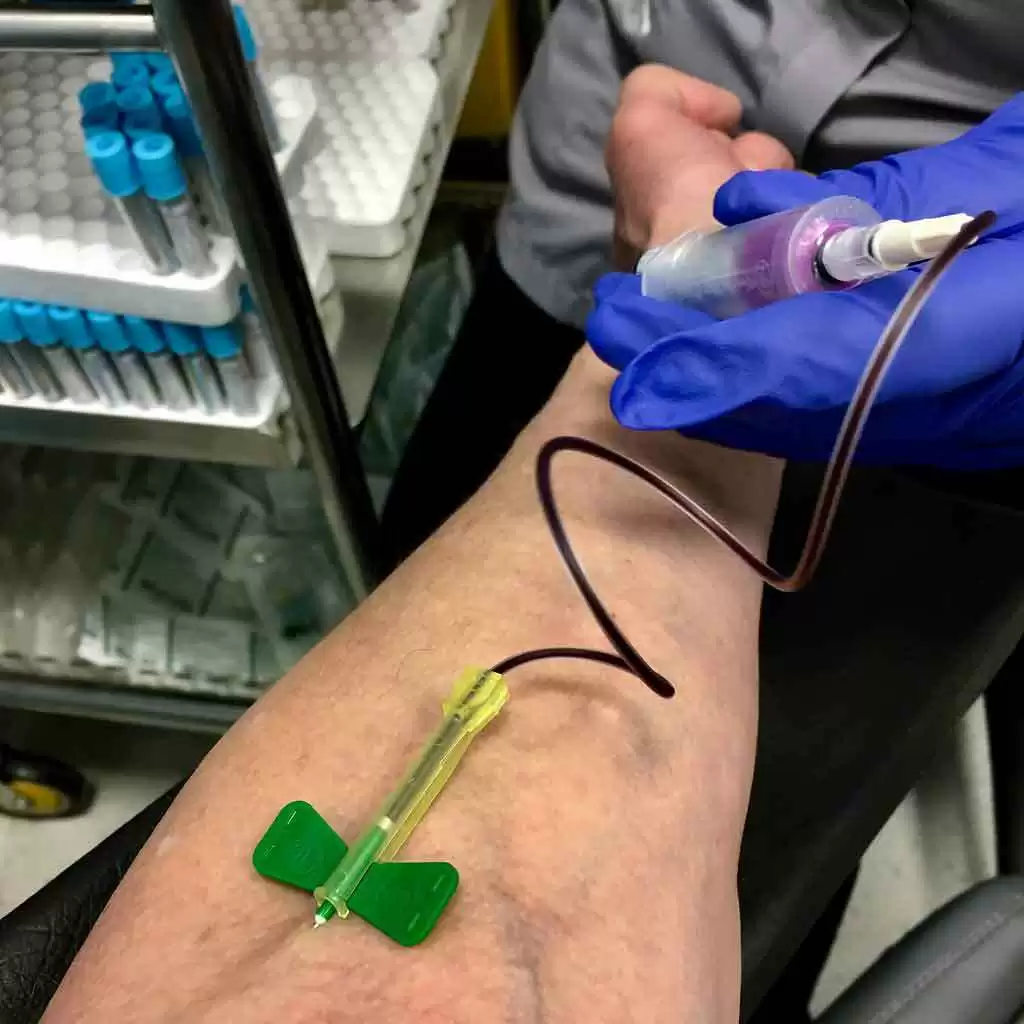
Celiac.com 07/13/2017 - Until recently, duodenal biopsy was considered the gold standard for diagnosing celiac disease, but that is changing. A number of studies have shown that celiac disease can be diagnosed using serological tests alone, but many clinicians have yet to embrace this approach. In both retrospective and prospective studies, one research team showed that certain IgA-tissue transglutaminase antibodies levels can predict celiac disease in adults 100% of the time. After making some adjustments to the analytical method for measuring the antibody, a team of researchers recently set out to to determine whether such serum tests can reliably diagnose celiac disease in large numbers adult patients without the need for small bowel biopsy. The research team included GKT Holmes, JM Forsyth, S Knowles, H Seddon, PG Hill, and AS Austin. They are variously associated with the Royal Derby Hospital, the Department of Pathology, and the Derby Digestive Diseases Centre at the Royal Derby Hospital in Derby, UK. For their study, the team conducted a retrospective analysis in an unselected series of 270 adult patients who underwent small bowel biopsies and the measurement of serum IgA-tissue transglutaminase antibody levels from 2009 to 2014. At an IgA-tissue transglutaminase antibody cut-off greater than 45 U/ml (>8×upper limit of normal+2SDs) the positive predictive value for celiac disease in this cohort was 100%; 40% of cases were above this cut-off. The team found that they could use IgA-tissue transglutaminase antibody levels to reliably diagnose celiac disease in a high proportion of these adult patients. This study adds to the growing body of evidence that supports the diagnosis of celiac disease without a mandatory small bowel biopsy. As a realist of these findings, the study team has changed the diagnostic guidelines for their center, and will now make celiac diagnosis based on cut-off levels of IgA-tissue transglutaminase. This is exciting news. For many, many years, the biopsy was considered the gold standard for diagnosing celiac disease. By eliminating biopsies in favor of IgA-tissue transglutaminase levels, diagnosing celiac disease could become much easier and even cheaper. Do you have celiac disease? Did you receive a biopsy for diagnosis? How do you feel about celiac diagnosis without biopsy? Share your thoughts below. Source: Eur J Gastroenterol Hepatol. 2017 Jun;29(6):640-645. doi: 10.1097/MEG.0000000000000841.
-

Can Doctors Diagnose Celiac Disease in Kids Without Biopsy?
Jefferson Adams posted an article in Latest Research
Celiac.com 03/09/2016 - Can doctors reliably diagnose celiac disease in kids without duodenal biopsy? A team of researchers recently set out to see if they could use predictive values of transglutaminase (tTG) antibodies to diagnose celiac disease in kids, without performing duodenal biopsy. The research team included MA Aldaghi, SM Dehghani, and M Haghighat, of the Department of Pediatrics at Shiraz University of Medical Sciences in Shiraz, Iran. For their study, the team selected patients with likely celiac disease, who had been referred to a gastrointestinal clinic. The team first conducted physical examinations of the patients and performed tissue transglutaminase-immunoglobulin A (tTG-IgA) tests. For patients with serological titers higher than 18 IU/mL, the team performed upper endoscopy. The team assessed a total of 121 children, 69 female and 52 male, averaging 8.4 years of age. They found a significant association between blood tests and biopsy results; in other words, subjects with high antibody levels had more positive pathologic results for celiac disease, compared to others (P < 0.001). They achieved maximum sensitivity and maximum specificity of about 65% with a serological titer of 81.95 IU/ml. The calculated accuracy was lower in comparison with other studies. The team found lower antibody levels in patients with failure to gain weight and higher antibody levels in diabetic patients. In this study, a single blood test (tTg-IgA test) was not sufficient for researchers to reliably diagnose celiac disease without duodenal biopsy. Source: Iran J Pediatr. 2016 Feb;26(1):e3615. doi: 10.5812/ijp.3615. Epub 2016 Jan 30. -
Celiac.com 10/31/2020 - Since this article was originally published in 2008, the tTG test has become the standard for celiac disease screening, while a newer test called "Deamidated Gliadin Peptide (DGP)" is now considered the best for CD, and the company 2G Pharma is unfortunately no longer in business. Do you know someone who might benefit from a celiac blood test? Maybe they are too shy to assert themselves. Or maybe they’ve been turned down flat by a physician who is not current with the medical literature on celiac disease. As many of us know, asking for celiac testing is sometimes like hitting a brick wall. Stories abound of incorrect diagnoses, cavalier indifference, dismissal, denial, frustration, illness, often leading to a pervasive sense of futility. Each of these stories is punctuated by pain, illness, heartache, and sometimes, death. For the lucky ones, a health care professional who is well versed in celiac disease sometimes furnished the answer. Others found their own way to a gluten free diet. Until now, most have not been so lucky. However, the brick wall is starting to crumble. A powerful force is poised to bring new hope to that unlucky, unhappy, unhealthy majority of untreated, undiagnosed group with celiac disease. 2G Pharma Inc. is now offering an at-home test for IgA tissue transglutaminase antibodies (tTG) called the Biocard celiac test. Although currently only available in Canada, it can be ordered over the Internet for only $50. Although not yet approved by Health Canada, the newer version also tests for IgA deficiency, and will thus be more accurate than the celiac testing offered by many conventional laboratories (because they often fail to consider IgA deficiency). Few physicians would deny the extreme likelihood of celiac disease in the context of positive tTG test results. If the test shows IgA deficiency (when approved) although it is not as reliable an indicator of celiac disease, it would also be well accepted as indicating the need for further investigation for celiac disease. So this new test is offering something very special, and for a very small price. Those of us who are familiar with celiac disease know that if it goes untreated it can pose a wide range of challenges. Untreated celiacs can appear healthy. Or they can manifest just a single sign or symptom such as isolated iron deficiency or osteoporosis, or rheumatoid arthritis or cancer or thyroid disease or a brain disorder or a fertility problem. On the other hand, untreated celiacs can also show a confusing array of signs, symptoms, and associated autoimmune disease. Still others will report concerns and symptoms that seem more like psychological complaints than physical manifestations of a diet-driven autoimmune disease. For instance, we now know that there are more overweight and obese individuals with untreated celiac disease than there are underweight celiacs. That is what they mean when researchers talk about the protean manifestations of celiac disease. Whatever the symptom, sign, or ailment, it can stand alone as the sole indicator, or it can be one of a constellation of problems that are due to, or associated with, an underlying case of undiagnosed celiac disease. Yet few physicians will make the connection. Until now, most cases of celiac disease will never be diagnosed because medical professionals are taught to look for a consistent complex of signs and symptoms. Most believe that untreated celiac patients are gaunt, wasted, sickly, and have protruding bellies. While this may have been true in the past we now know that celiac disease is difficult, often impossible, to identify on the basis of symptoms. Objective testing is often the only way that celiac disease can be diagnosed. Thus, this new test will identify the vast majority of untreated celiac patients. And the test is easily defended against those who might look askance at home testing. Korponay-Szabo et. al. report in Alimentary Pharmacology and Therapeutics that this test is 97% specific and 97% sensitive (1). Test sensitivity is determined by how many celiacs are identified by a positive test. Only 3% of those with celiac disease failed to be identified by this test. However, the one celiac patient that was missed in this research project suffered from IgA deficiency, which is much more common in the context of celiac disease than in the general population. Further, because the newer form of this test would have identified this deficiency, it is very likely that the patient would be further investigated for celiac disease. Thus, the test could be argued to have been 100% sensitive in their study. The same group reported that the test is 97% specific. That means that the test will show positive in cases of celiac disease as well as in 3% of patients who do not have celiac diseae. Several other groups of researchers report that many of those who test positive for tTG often go on to develop celiac disease within a few months or years. Crovella et. al., report in Digestive and Liver Disease, similar results but with one important exception. When this test was used among a group of impoverished individuals who were infected with filariasis its specificity weakened substantially. People who were infected with this parasite showed positive tTG test results despite the absence of celiac disease. Thus, despite 100% specificity among Brazilian urbanites, the test was only 76% specific when used to screen impoverished suburban Brazilians. Thus, although this test is less than ideal in some third world settings among those with filariasis infections, it is clearly a powerful tool for identifying celiac disease in the industrialized world. Closer to home, 2G Pharma Inc. is rolling out this new test in Canada, as I write this column. I suggested to Janet Monk that there might be a little cross-border shopping. Her company has chosen to take the high road and avoid the risk of contravening U.S. import/export laws. Sadly, many crooks and charlatans feel perfectly happy to send drugs and other dangerous substances into the US. Yet this young company, offering a simple (but powerful) blood test that could save the US medical system billions of dollars annually, is forced to await appropriate approvals before sending their product into the US. Bear in mind that it is not a drug. It is an at-home test for a dangerous disease that goes undiagnosed in 97% of cases in the U.S. (3) and because of all the associated ailments, takes an enormous toll on at least three million Americans (4). I would love to see this product available in the U.S., if only to stem the enormous risk of illness and lurking cancers that have been shown to reduce on a gluten free diet among those with celiac disease. If you live in Canada, you can order or encourage others to order the test. If you live elsewhere, perhaps there is something you can do to make this test available in the U.S. If nothing else, you can order and make use of the test when you visit Canada. In the meantime, this grand new test is poised and ready help diagnose the millions of Americans who will otherwise go untested and undiagnosed. I am confident that some alternative can be implemented to harness this test and get it working for Americans and Canadians alike. Sources: Korponay-Szabó IR, Raivio T, Laurila K, Opre J, Király R, Kovács JB, Kaukinen K, Fésüs L, Mäki M.Coeliac disease case finding and diet monitoring by point-of-care testing. Aliment Pharmacol Ther. 2005 Oct 15;22(8):729-37. Crovella S, Brandao L, Guimaraes R, Filho JL, Arraes LC, Ventura A, Not T.Speeding up coeliac disease diagnosis in the developing countries. Dig Liver Dis. 2007 Oct;39(10):900-2. Epub 2007 Aug 13. Green PH.Where are all those patients with Celiac disease? Am J Gastroenterol. 2007 Jul;102(7):1461-3. Fasano A, Berti I, Gerarduzzi T, Not T, Colletti RB, Drago S, Elitsur Y, Green PH, Guandalini S, Hill ID, Pietzak M, Ventura A, Thorpe M, Kryszak D, Fornaroli F, Wasserman SS, Murray JA, Horvath K. Prevalence of celiac disease in at-risk and not-at-risk groups in the United States: a large multicenter study. Arch Intern Med. 2003 Feb 10;163(3):286-92.
- 2 comments
-
- blood test
- blood testing
-
(and 5 more)
Tagged with:
-
Celiac.com 03/02/2020 - Current practice of using biopsy to diagnose children with celiac disease is changing to diagnosis without biopsy. The European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) recently issued new guidelines that recommend doctors diagnosing celiac disease omit biopsy in favor of a two-stage blood test, for the majority of children suspected of having the disease. New guidelines for diagnosing celiac disease in children call for avoiding biopsies in favor of a two-stage blood test. Until now, about half of all kids diagnosed with celiac disease got a biopsy. The new guidelines mean that nearly all kids will avoid the procedure in favor of a two-stage blood test. The new guidelines recommend that doctors: Conduct antibody screening in children with suspected celiac disease; Diagnose symptomatic children without biopsy, using the same criteria as in patients with symptoms; Invite parents and, where appropriate, children into any discussion about using biopsy; The new guidelines appear in the Journal of Pediatric Gastroenterology and Nutrition and call for clinicians diagnosing children with celiac disease to rely on accurate serology-based diagnosis without biopsy. Being able to diagnose children without biopsy is a major advance in celiac disease diagnosis, and will save millions of parents and children from what can be a costly, intimidating, and uncomfortable procedure that is not free of risk. Read more at News-medical.net
- 3 comments
-
- biopsy
- blood tests
-
(and 6 more)
Tagged with:
-
Celiac.com 04/24/2020 - We've all heard of smart phones and smart TVs, but what about smart toilets? You heard right. In the near future, a simple trip to the bathroom might provide a medical diagnosis for celiac or numerous other diseases and medical conditions. Researchers at Stanford University have created a toilet attachment that can analyze urine and feces for common diseases and medical conditions, such as celiac disease, and irritable bowel syndrome, among others. The sensor attaches to the inside of the toilet bowl, records samples, and analyzes the results using complex software. Results are then stored in the cloud for doctors to review. Aside from taking readings to diagnose disease, the toilet works exactly the same as any other toilet, which is part of the plan. “The user doesn’t have to do anything differently,” said lead author Sanjiv Gambhir. Since everyone uses the bathroom, the smart toilet offers clinicians a reliable way to collect patient data, which unlike wearable technology, cannot be forgotten. The smart toilet won't be taking the place of a doctor, nor will it be providing diagnosis directly to the patient. "In fact, in many cases," says Gambhir, "the toilet won’t ever report data to the individual user.” Turns out you bum hole is every bit as unique as your fingerprint, which means it can be used to identify any given user. In the same way a smartphone can identify users with fingerprints or facial scans, the smart toilet can do the same with an anal print. The reason for this is that more and more toilets are hands-free, so making sure the data is properly recorded for each user becomes an issue. With anal recognition technology, the smart toilet can identify each user with complete accuracy. You won't find the smart toilet online just yet. The device is currently only for use on test subjects at Stanford. The development team is still working to accurately improve the toilet, and they are working to develop modules that detect symptoms and illnesses like dehydration, enlarged prostate, including "cancers and COVID-19," says senior researcher Seung-min Park Read more at Medgadget.com
- 3 comments
-
- celiac
- celiac disease
- (and 7 more)
-
Hello, this is my first post and to be honest I’m shocked I’m here. I have no stomach problems and felt generally healthy up until a few weeks ago. I am now broken. Ive had an itchy scalp for ages but recently it got infected. The doc treated the infection but since I have broken out in the most horrendous rash which I think is D.H which just stared on my scalp It started as small red spots, watery blisters that pop under the lightest touch. Now huge raised crusty lumps. All itching to my bones and sometimes burning. I have been docs 5 times in two weeks and today a&e as I feel completely desperate. I’m scared, anxious and a shell of the person I was last month. I keep mentioning the gluten rash to people and they’re brushing it off, saying it’s viral, a reaction etc. I feel crazy as I 100% tick every box for this. I’m also light headed and my eyes hurt. So my question would be,how do I get help. What do I say? Ive had a gluten blood test so waiting on the result. I’ve been referred to dermatologist but that could take 12 weeks. This is consuming me and I’m so scared it could take forever to get sorted. thanks in advance xx
- 3 replies
-
- dermatitis
- diagnose
-
(and 1 more)
Tagged with:
-
Hello, I am new here My son is 11yo, he is in the spectrum. My son used to have recurrent cavities until I changed dentists and he said no gluten, dairy or refined sugars. I took him out of those 3 and he "only" has a cavity every year or so In 2017 my dad (his grandpa) passed away from complications to celiac that was not diagnosed in time. But I cannot get mt son's dad to cooperate, we are divorced, joint custody 50/50 time split, which means he is every other whole weekend with his dad eating basically chicken nuggets, cake, cookies, oreos, kitkat, pizza, cheese sticks steak and rice. This is right from the dad's mouth as well as the kids account. No veggies at all. Now I need him diagnosed just so that his dad will eliminate the gluten. I do not know if my son is celiac, But I am learning that unless I myself give him big amounts of gluten, I will not get any gluten issues in a blood test or even endoscopy What can I do, do I have to put my son in weeks of gluten just that it shows in a test? If its genetic, will it show? Doing tests in children is tough, doing them in children with Autism is 3 times harder, just getting the stool sample, which is the only tests I have completed, was difficult How can I help my son? Thank you!! in avance
-
Celiac.com 02/01/2018 - To make a clinical diagnosis of celiac disease, doctors use serological testing for IgA antibodies to human tissue transglutaminase (anti-tTG) which indicate celiac disease autoimmunity. However, some tests are more highly sensitive for anti-tTG, while other tests are highly specific. So, is combining two tests a reliable strategy for screening for celiac disease in clinical practice? A team of researchers recently compared the performance of three kits used to diagnose celiac disease, and evaluated the point prevalence of celiac disease autoimmunity in a South Indian urban population. The research team included G Venugopal, J Mechenro, G Makharia, A Singh, S Pugazhendhi, R Balamurugan, and BS Ramakrishna. They are variously associated with the SRM Institutes for Medical Science, Jawaharlal Nehru Salai, Vadapalani in Chennai, India, the SRM Medical College Hospital and Research Centre, Kattankulathur, India, the All India Institute of Medical Sciences, Ansari Nagar, New Delhi, India, the Kansas University Medical Center, Kansas City KS, USA, the Indian Institute of Technology, Samantapuri, Bhubaneswar, India, the SRM Institutes for Medical Science, Jawaharlal Nehru Salai, Vadapalani, Chennai, India, and with the SRM Medical College Hospital and Research Centre, Kattankulathur, India. For the first part of their study, the team performed anti-tTG testing on sera from 90 patients with documented celiac disease and 92 healthy controls using three different kits. They then tested one thousand nine hundred and seventeen healthy adults residents of the Vellore and Kancheepuram districts for celiac disease autoimmunity using a sequential two-test strategy. Based on these results, the team suggests that using first a highly sensitive test for anti-tTG followed by a highly specific test is a reliable strategy for screening for celiac disease in clinical practice. Source: Indian J Gastroenterol. 2017 Dec 22. doi: 10.1007/s12664-017-0803-z.
-
Celiac.com 08/28/2017 - After 14-day gluten challenge, an HLA-DQ-gluten tetramer blood test provides better detection of celiac disease than biopsy. Can that lead to new disease detection methods in patients who are already on a gluten-free diet? Doctors attempting to diagnose celiac disease are often confronted by patients who have already given up gluten. For such patients, diagnostic guidelines currently call for a gluten challenge of at least 14 days, followed by duodenal biopsy. There isn't much good data on how many false-positive results are generated by this method. To get a better picture, a team of researchers recently studied responses to 14-day gluten challenge in subjects with treated celiac disease. The research team included Vikas K Sarna, Gry I Skodje, Henrik M Reims, Louise F Risnes, Shiva Dahal-Koirala, Ludvig M Sollid, and Knut E A Lundin. They are variously affiliated with the Department of Immunology and Transfusion Medicine, Oslo University Hospital, Norway; K. G. Jebsen Coeliac Disease Research Centre, University of Oslo, Norway; Department of Clinical Service, Oslo University Hospital, Norway; Department of Pathology, Oslo University Hospital, Norway; Centre for Immune Regulation, University of Oslo and Oslo University Hospital, Norway; and the Department of Gastroenterology, Oslo University Hospital, Norway. The research team took a group of 20 patients with biopsy-verified celiac disease, all in confirmed mucosal remission, and presented them with a dietary gluten challenge of 5.7 grams per oral gluten per day for 14 days, then conducted duodenal biopsies. They analyzed blood by multiplex assay for cytokine detection, and by flow cytometry using HLA-DQ:gluten tetramers. Nineteen of the twenty participants completed the challenge. Biopsy results showed villous blunting in 5 of those 19 patients. Villous height to crypt depth ratio reduced with at least 0.4 concomitantly with an increase in intraepithelial lymphocyte count of at least 50% in 9 of the 19 patients. Interleukin-8 plasma concentration increased by more than 100% after 4 hours in 7 of 19 subjects. Frequency of blood CD4+effector-memory gut-homing HLA-DQ:gluten tetramer-binding T cells increased by more than 100% on day 6 in 12 of 15 evaluated participants. For most celiac patients, a 14-day gluten challenge did not result in sufficient mucosal architectural changes for clear diagnosis (sensitivity ≈25%–50%). The team found that an increase in CD4+ effector-memory gut-homing HLA-DQ:gluten tetramer-binding T cells in blood 6 days after gluten challenge is a more sensitive and less invasive biomarker for celiac disease. The team is calling for further study. Being able to diagnose celiac disease without biopsy could really help to improve the entire diagnostic process, and could easily lead to an increase in diagnosis. Source: Gut
-
Celiac.com 06/05/2017 - Doctors diagnose celiac disease by confirming various clinical, genetic, serologic, and duodenal morphology features. Based on retrospective data, recent pediatric guidelines propose eliminating biopsy for patients with IgA-TTG levels more than 10-times the upper limit of normal (ULN), along with a few other criteria. One retrospective study showed that researchers using levels of IgA-TTG and total IgA, or IgA-TTG and IgG against deamidated gliadin (IgG-DGL) could identify patients both with and without celiac disease. A team of researchers recently set out to validate the positive and negative predictive values (PPV and NPV) of these diagnostic procedures. The research team included Johannes Wolf, David Petroff, Thomas Richter, Marcus KH. Auth, Holm H. Uhlig, Martin W. Laass, Peter Lauenstein, Andreas Krahl, Norman Händel, Jan de Laffolie, Almuthe C. Hauer, Thomas Kehler, Gunter Flemming, Frank Schmidt, Astor Rodriques, Dirk Hasenclever, and Thomas Mothes. Their team conducted a prospective study of 898 children undergoing duodenal biopsy analysis to confirm or rule out celiac disease at 13 centers in Europe. They then compared results from antibody tests with results from biopsies, follow-up data, and diagnoses made by the pediatric gastroenterologists. In all cases, diagnosis was made for celiac disease, no celiac disease, or no final diagnosis. Blinded researchers measured levels of IgA-TTG, IgG-DGL, and endomysium antibodies, while tissue sections were analyzed by local and blinded reference pathologists. The team validated two procedures for diagnosis: total-IgA and IgA-TTG, as well as IgG-DGL with IgA-TTG. Patients whose antibody concentrations for all tests were below 1-fold the ULN were assigned to the no celiac disease category. Those whose antibody concentrations for at least one test were above 10-fold the ULN were assigned to the celiac disease category. All other cases were considered to require biopsy analysis. The team calculated the ULN values using the cut-off levels suggested by the test kit manufacturers. They conducted HLA-typing for 449 participants. To extrapolate the PPV and NPV to populations with lower rates of celiac disease, they used models that accounted for how specificity values change with prevalence. In all, the team found 592 patients with celiac disease, 345 who did not have celiac disease, and 24 with no final diagnosis. The TTG-IgA procedure identified celiac disease patients with a PPV of 0.988 and an NPV of 0.934. The TTG-DGL procedure identified celiac disease patients with a PPV of 0.988 and an NPV of 0.958. Their extrapolation model estimated that PPV and NPV would remain above 0.95 even at a disease prevalence as low as 4%. Meanwhile, tests for endomysium antibodies and HLA type did not increase the PPV of samples with levels of IgA-TTG 10-fold or more above the ULN. Interestingly, the pathologists disagreed in their analyses of duodenal morphology about 4.2% of the time, a rate comparable to the error rate for serologic tests. This study validates the use of the TTG-IgA procedure and the TTG-DGL procedure in lieu of biopsy to diagnose pediatric patients with or without celiac disease. Source: Gastroenterology. DOI: http://dx.doi.org/10.1053/j.gastro.2017.04.023 The researchers are variously affiliated with the Institute of Laboratory Medicine, Clinical Chemistry and Molecular Diagnostics, Medical Faculty of the University and University Hospital, Leipzig, Germany, the Institute for Medical Informatics, Statistics & Epidemiology (IMISE), University of Leipzig, Germany, the Department of Paediatrics, University of Oxford, Oxford, United Kingdom, the Translational Gastroenterology Unit, Nuffield Department of Medicine, University of Oxford, John Radcliffe Hospital, Oxford, United Kingdom, the, University Children's Hospital Halle, Germany, the Medical School, Hannover, Germany, Helios Hospital, Department of Paediatrics, Plauen, Germany, the Children's Hospital Prinzessin Margaret, Darmstadt, Germany, the University Children's Hospital Graz, Austria, the Children's Hospital, Justus Liebig University Giessen, Germany, the University Children's Hospital Leipzig, Germany, the Children's Hospital of the Clinical Centre Sankt Georg Leipzig, Germany, the Clinical Trial Centre, University of Leipzig, Germany, the DKD Helios Children's Hospital, German Clinic for Diagnostics, Wiesbaden, Germany, the University Children's Hospital, Technical University Dresden, Germany, and the Alder Hey Children's National Health Service Foundation Trust, Liverpool, United Kingdom.
- 1 comment
-
- antibodies
- biopsy
-
(and 8 more)
Tagged with:
-
Celiac.com 01/09/2015 - A recent article by Jody Berger provides a cautionary tale for anyone suffering from non-classic symptoms of gluten-sensitivity or celiac disease. Berger, it turns out, has non-celiac gluten-sensitivity. Sounds simple enough, right? But in Berger’s case, it took her one year and visits to a dozen doctors to get an accurate diagnosis. Berger’s main symptom was tingling in her fingertips, a feeling of slight pins and needles, as if they were waking from a deep sleep. The sensation wasn’t painful, she said, but it was persistent, and concerned her enough that she sought medical help to figure out the cause. When her first doctor diagnosed her with multiple sclerosis after a very brief visit, Berger sought a second, then a third, then a fourth opinion. In the course of her many visits, doctors told her she had nutritional deficiencies, heavy metal toxicity, Lyme disease, and depression. After a dozen visits, she finally found an osteopath who was “well-versed in systems thinking,” and another physician who had trained in ayurvedic medicine, a holistic system of healing. The tingling, which the first doctor believed to be a sign of MS, is actually a fairly common, though not classic, symptom of gluten sensitivity. This story highlights the amount of work patients can face when they present with atypical symptoms of gluten-sensitivity. Many times, well-intended doctors can simply miss the dietary connection and get the diagnosis wrong. Do you have a similar story of well-intended, but misguided doctors wrongly diagnosing gluten-sensitivity or celiac disease? Read more about Berger’s year-long Odyssey here.
- 23 comments
-

How Early Can You Diagnose Celiac Disease?
Dr. Rodney Ford M.D. posted an article in Autumn 2016 Issue
Celiac.com 10/12/2016 - How early can you diagnose celiac disease? This is a most challenging question for everyone: children, parents, pediatricians, gastroenterologists and many other health professionals. This is because, like so many other diseases, celiac disease is a progressive condition that slowly creeps up on you. In addition, there is disagreement about what constitutes a definitive diagnosis of celiac disease. What if the small bowel biopsy result is at odds to the blood test results? It is my opinion that the fundamental diagnostic requirements for celiac disease remain unresolved. This makes early diagnosis problematic! Do you keep waiting (whilst suffering from symptoms) for classic gut damage to be visible in a bowel biopsy before adopting a gluten-free diet? Or do you recognize the early onset of celiac disease and go gluten-free prior to this gut damage occurring? Will you be accused of "masking" celiac disease if you are an early gluten-free adopter? Currently, most guideline protocols require a definitive diagnosis of celiac disease by demonstrating small bowel tissue damage. This is achieved by performing and upper gastrointestinal endoscopy, taking a tissue biopsy of the mucous lining of the small bowel, and then showing specific tissue damage (villus atrophy) under the microscope: this is the small bowel biopsy procedure. However there is significant controversy about the accuracy and necessity of a small bowel biopsy test. We will have a close look at the difficulties and shortcomings of these tests. But first, let's look at these diagnostic problems in relation to Francesca. Meet Francesca who is highly at risk of celiac disease So how early could we diagnose Francesca's celiac disease? She has just turned 3-years-old. Her mother has celiac disease, diagnosed over 10 years ago. So mum bought Francesca for my opinion because she had started to have some loose bowel motions (runny poops), although sometimes she did have hard bowel motions, which were difficult to pass. She also had a big distended tummy, was getting more cranky, and a bit more tired. Because of mother's celiac disease, Francesca was already consuming a smaller amount of gluten, although she was eating at least one slice of normal wheat gluten bread each day. Her mother's question was: "Has Francesca now developed celiac disease?" This problem confronts me most days in the Clinic. How should I investigate and manage her illness? What blood tests should I request? How do I interpret her results? Should I organize a small bowel biopsy? Do we look for early evidence of gluten problems, or do we wait for end stage celiac damage? Should she go on a gluten-free diet now? Should we be concerned about "masking" celiac disease? Francesca's blood tests show: She does carry the HLA gene DQ2: this makes her a likely candidate for developing celiac disease. The tissue-damage antibodies were normal: the tTG (tissue Trans-Glutaminase) levels were low normal, but the IgG-DGP (Diamidated Gliadin Peptide) levels were borderline (18 units, with a normal range 0-20). Her EMA (Endomesial Antibody) was negative: the borderline DGP is very suspicious and evidence of early celiac disease. IgG-AGA (Anti-Gliadin-Antibody) level was moderately raised: showing that she has developed an immune response to gluten. She has not had an endoscopy: with her tissue damage antibodies at low levels, the likelihood of abnormal tissue histology is very low. My opinion In my opinion, this child is at extreme risk of developing celiac disease. I would like to see her on a strict gluten zero. However, it is now up to her parents to decide whether they will wait until she actually develops gut damage, or do something now to prevent her getting a serious disease. What would you do if she were your child? Well her parents decided to place her gluten-free and they saw a big change for the better in just a few weeks. Her bowels become normal, her energy levels improved and she is now a happy girl. So what is her diagnosis? I call her early celiac disease. Others would say she has non-celiac gluten-sensitivity. Some would claim that I am unwarranted to suggest a gluten-free diet until she has a positive biopsy and they accuse me of "masking" celiac disease by treating her symptoms. Why let Francesca unnecessarily suffer whilst waiting for her to get progressively sicker until we can get a tissue diagnosis? Written in the spirit of cooperation and knowledge sharing. You can read many more patient stories in my book "Gluten-Related Disorder: Sick? Tired? Grumpy?" (www.GlutenRelatedDisorder.com).- 12 comments
-
- celiac
- celiac disease
-
(and 3 more)
Tagged with:
-
Celiac.com 01/26/2015 - Celiac disease occurs along a spectrum, which includes cases where patients have only minor histological abnormalities, or, what is called "potential celiac disease." Can a scientific equation based on immunohistochemical analysis of duodenal biopsies help to better diagnose celiac disease and cases of potential celiac disease? A team of researchers recently set out to assess the potential of immunohistochemical analysis of duodenal biopsies to aid in the diagnosis of gluten-related minor enteropathy. The research team included A. Tosco, M. Maglio, F. Paparo, L. Greco, R. Troncone, and R. Auricchio. They are affiliated with the Department of Translational Medical Science, Section of Pediatrics, and the European Laboratory for the Investigation of Food Induced Diseases at the University Federico II in Naples, Italy. For their analysis, the team looked at duodenal biopsies from 56 untreated celiac patients and 56 control subjects, and assessed patients based on CD3 and γδ intraepithelial lymphocytes number, γδ /CD3 ratio, and density of CD25+ lamina propria cells. To help them blindly evaluate 61 more biopsies with normal villous architecture, the team used a discriminant equation, that is, an equation that allows them to determine whether the patient has celiac disease based on the four factors noted above. Both celiac patients and control subjects showed widely variable immunohistochemical ranges, and no single parameter showed sufficient specificity for celiac disease. However, by combining parameters for all four markers, the team was able to produce an accurate discriminant equation. The result of the team’s discriminant equation is a score called a Dscore. Their equation is as follows: Dscore = (CD3 x 0.06) - (γδ x 0.119) + (CD25 x 0.012) + (γδ /CD3 x 0.131) - 4.709. Under the team’s system, patients’ Dscores could be used to correctly point to celiac disease in 97.3% of cases. When the team applied this equation to a validation set of 61 patients with normal villous architecture and unknown diagnosis, 92.9% of those with a positive score turned out to be potential celiac patients. However, a normal score did not exclude celiac disease. In certain cases, immunohistochemistry can be helpful for diagnosing celiac disease, but, because it lacks sensitivity, it can miss some potential celiac cases. Source: J Pediatr Gastroenterol Nutr. 2014 Dec 14.
- 1 comment
-
- celiac
- celiac disease
-
(and 4 more)
Tagged with:
-
Celiac.com 09/08/2014 - Currently, physicians trying to diagnose celiac disease in patients with lymphocytic enteritis look for subepithelial deposits of anti-tissue transglutaminase IgA. However, it is known that an increase in CD3+TCRγδ+ coupled with a decrease in CD3- intraepithelial lymphocytes (IEL) is a flow cytometric pattern clearly indicating celiac disease with atrophy. To determine which method yielded better diagnostic results, a research team set out to compare and contrast intestinal intraepithelial lymphocyte cytometric pattern with subepithelial deposits of anti-tissue transglutaminase IgA for diagnosing lymphocytic enteritis due to celiac disease. The researchers included F. Fernández-Bañares, A. Carrasco, R. García-Puig, M. Rosinach, C. González, M. Alsina, C. Loras, A. Salas, J.M. Viver, M. Esteve. They are variously affiliated with the Department of Gastroenterology, Hospital Universitari Mutua Terrassa, University of Barcelona, Centro de Investigación Biomédica en Red de Enfermedades Hepáticas y Digestivas (CIBERehd), the Department of Pediatrics, Hospital Universitari Mutua Terrassa, University of Barcelona, the Department of Pathology, Hospital Universitari Mutua Terrassa, University of Barcelona, CIBERehd, Terrassa, and the Department of Immunology, CATLAB, Viladecavalls, all in Barcelona, Spain. For their study, the team evaluated 144 women and 61 men, with positive celiac genetics, who underwent duodenal biopsy for celiac disease. Fifty patients showed villous atrophy, and 70 showed lymphocytic enteritis, while 85 showed normal histology. Eight patients with non-celiac atrophy and 15 with lymphocytic enteritis secondary to Helicobacter pylori served as control group. The team used duodenal biopsies to assess both celiac disease, IEL flow cytometric (complete or incomplete), and IF patterns. Sensitivity of IF, and complete and incomplete cytometric patterns for celiac disease diagnosis in patients with positive serology (Marsh 1+3) was 92%, 85% and 97% respectively, but only the complete cytometric pattern showed 100% specificity. Twelve seropositive and 8 seronegative Marsh 1 patients received a celiac disease diagnosis at the beginning of the study or after gluten free-diet, respectively. For celiac disease diagnosis in lymphocytic enteritis at baseline, cytometric pattern yielded better diagnostic results than both IF pattern and serology (95% vs 60% vs 60%, p = 0.039). Analysis of the IEL flow cytometric pattern offers fast, accurate reliable way to spot celiac disease in the initial diagnostic biopsy of patients presenting with lymphocytic enteritis, even for patients with negative blood screens, and seems superior to anti-TG2 intestinal deposits. These results support the analysis of the IEL flow cytometric pattern as the best way to spot celiac disease at the first diagnostic biopsy of patients presenting with lymphocytic enteritis, even for patients with negative blood screens. Source: PLoS One. 2014 Jul 10;9(7):e101249. doi: 10.1371/journal.pone.0101249.
-
- celiac
- celiac disease
-
(and 6 more)
Tagged with:
-
Celiac.com 08/01/2014 - I sometimes have to remind myself that it’s the 21st century, and that some amazing scientific breakthroughs that sound like something out of science fiction are, in fact, real. Take for example the technology, recently developed by researchers at the University at Buffalo, that allows researchers to safely examine intestines using nanoparticles. The popular name for these orally administered nanoparticles suspended in liquid is ‘Nanojuice.’ Human small intestines are each about 23 feet long and 1 inch thick. Located between the stomach and the large intestine, the small intestine is notoriously difficult to examine, hence procedures like biopsies, endoscopies, etc. The new technique, being developed by researchers at the University at Buffalo, uses nanoparticles and lasers to image the organ. Once the nanoparticles reach the intestines, doctors can strike the particles with a harmless laser. The technique provides real-time view of the intestine. This will help doctors diagnose irritable bowel syndrome, celiac disease, Crohn's disease and other gastrointestinal illnesses, according to the researchers. So far, the research team has only tested their technology on mice, but they plan to refine the technique for clinical trials on human subjects. Researchers say that this method can help doctors get a better picture of the nature of celiac and other diseases. The study is published in the journal Nature Nanotechnology. What do you think? Will products like nanojuice represent the future of celiac disease diagnosis? If it is shown to be safe, would you prefer it to a biopsy? Source: Natureworldnews.com
- 2 comments
-
- celiac
- celiac disease
-
(and 3 more)
Tagged with:
-
Celiac.com 02/18/2013 - Currently, there are two main diagnostic tools available to would-be celiacs: biopsy and serological (antibody) tests. For the past few decades, biopsy has been the only relatively reliable (and diagnostically accepted) path to diagnosis. The problem is, biopsies are expensive and highly invasive – antibody tests would be a cheap and painless alternative, but they haven't proven themselves to be accurate enough for conclusive diagnosis. However, a recent analysis shows that antibody tests have improved a great deal in recent years and when used to test for multiple antibodies concurrently, they can be almost as effective as biopsies for diagnosing celiac disease. The study's facilitators began their restrospective analysis by collecting serum samples from 268 patients at hospitals throughout Switzerland, Germany and Austria. All included patients suffered from celiac-like symptoms and underwent both biopsy and antibody testing within 2 months of serum collection. All included patients were on gluten-containing diets at the time of testing. 149 of the patients were ultimately diagnosed with celiac disease; the other 119 showed normal intestinal mucosa and were considered celiac-free. These patients were the control group. Usually, potential celiac patients are tested for IgA anti- tTG or EMA. If the test is positive, then diagnosis is then confirmed with biopsy. However, there is still a chance that the test will throw a false positive, meaning many people are put through unnecessary biopsies. The goal of the present study was to develop a method for reducing the number of these unnecessary biopsies. It was found that when two antibody tests are used, the reliability of the tests increased substantially, weeding out a great many false positives, as well as picking up some false negatives. When three tests were used, the numbers became even more accurate – when used concurrently and all three show a positive result, the IgA anti-dpgli, igG anti-dpgli and IgA anti-tTG achieved an 87% positive likelihood and .01% negative likelihood (compared to a positive likelihood of only 7% and negative likelihood of 0.04% with just the IgA anti-tTG). Using these three tests together, only one test subject came through as a false positive, and only two came through as false negatives (compared to 16 false positives and 5 false negatives with the IgA anti-tTG only). 60 came through with discordant results (meaning at least one of the tests came back negative – in these cases, biopsy is necessary). When considering that biopsy really only has a real-world diagnostic accuracy rate of about 90%, the three test combination utilized in this study achieves strong enough numbers that biopsies are starting to look unnecessary. Biopsy still might be the surest way of detecting celiac disease, but this study shows that it is not necessary in all cases, and patients seeking celiac diagnosis have a few more tests they can ask their doctors for. Source: http://www.biomedcentral.com/1471-230X/13/19
- 9 comments
-
Celiac.com 04/01/2013 - There haven't been many studies that evaluate the usefulness of capsule endoscopy in equivocal celiac disease. A team of researchers recently set out to conduct an evaluation of capsule endoscopy in adult celiac disease, and to assess its potential role in equivocal cases of celiac disease compared with patients with biopsy-proven and serology-proven celiac disease who have persisting symptoms. The research team included M. Kurien, K.E. Evans, I. Aziz, R. Sidhu, K. Drew, T.L. Rogers, M.E. McAlindon, and D.S.Sanders. They are affiliated with the Department of Gastroenterology at Royal Hallamshire Hospital, Sheffield Teaching Hospitals NHS Foundation Trust in Sheffield, South Yorkshire, United Kingdom. To determine the use of capsule endoscopy in patients with equivocal celiac disease, compared to patients with biopsy-proven and serology-proven celiac disease who have ongoing symptoms. To do this, the team conduced a prospective cohort study of 62 patients with equivocal celiac disease and 69 patients with non-responsive celiac disease. They measured outcome according to the diagnostic yield of capsule endoscopy in equivocal cases and accuracy of mucosal abnormality detection in patients with non-responsive celiac disease. They found that the 62 cases of equivocal celiac disease could be divided into two subgroups: group A, with 32 cases of antibody-negative villous atrophy, and group B with 30 cases of Marsh 1-2 changes. In group A, using capsule endoscopy, the team was able to diagnose celiac disease or Crohn's disease in 9 of 32 patients (28%), compared with just 2 of the 30 patients in group B (7%; P = .044). In patients with persistent celiac disease symptoms, the team made significant capsule endoscopy findings in 8 of 69 patients (12%), including 2 cases of enteropathy-associated lymphoma, 4 cases of type 1 refractory celiac disease, 1 polypoidal mass histologically confirmed to be a fibroepithelial polyp, and 1 case of ulcerative jejunitis. This outcome was significantly lower than the diagnostic yield of capsule endoscopy in antibody-negative villous atrophy (P = .048). It is important to remember that this study was restricted to a single clinic. That said, this is the first time that researchers have used capsule endoscopy to systematically evaluate equivocal celiac disease. Because the diagnostic rates for capsule endoscopy in patients with antibody-negative villous atrophy are better than that of capsule endoscopy in patients with celiac disease with persisting symptoms, the researchers are encouraging the use of capsule endoscopy in equivocal cases, especially in cases where patients antibody-negative villous atrophy. Source: Gastrointest Endosc. 2013 Feb;77(2):227-32. doi: 10.1016/j.gie.2012.09.031.
-

Can Bacteria Help Researchers Better Diagnose Celiac Disease?
Jefferson Adams posted an article in Latest Research
Celiac.com 01/30/2013 - Currently, doctors diagnose celiac disease with blood tests that screen for two antibodies, one that targets gluten and another that goes after an intestinal protein. The tests work pretty well to spot advanced cases of celiac disease, but by that time, patients are already suffering intestinal damage. A research team looking into a method for reliable earlier detection of celiac disease focused on the responses of certain bacteria to celiac disease. They have built a library of peptides on the surfaces of bacteria which capture new antibodies associated with celiac disease. This, in turn, has led them to a new technique for harvesting celiac disease antibodies, which may help improve diagnosis for celiac disease, especially early on. The researchers say the technique may allow them to successfully tell, much earlier than before, which perspective celiac sufferers are sick and which are healthy. The research team included Bradley N. Spatola, Joseph A. Murray, Martin Kagnoff, Katri Kaukinen, and Patrick S. Daugherty. They are affiliated with the Department of Chemical Engineering at the University of California at Santa Barbara, California, the Division of Gastroenterology and Hepatology, Mayo Clinic, Rochester, Minnesota, the Laboratory of Mucosal Immunology, Department of Medicine and the Department of Pediatrics at the University of California at San Diego in La Jolla, California and with the Department of Gastroenterology and Alimentary Tract Surgery, Tampere University Hospital, Tampere, Finland. For their study, Patrick Daugherty, of the University of California, Santa Barbara, and his team aimed to find previously unknown disease-linked antibodies. Their strategy centered on building an enormous library of random peptide sequences to find ones that would bind to the antibodies. To create their library, the researchers inserted one billion random peptide genes into Escherichia coli, with one peptide gene per bacterium. Once the genes were expressed inside the bacteria, thousands of copies of the peptides migrated to the cells’ surface. The researchers hoped that some of these peptides would bind antibodies from the blood of people with early-stage celiac disease, but not those in samples from healthy people. The team hoped that their approach, with numerous bacteria each bearing a different peptide, would be more likely to identify unknown antibodies than are current types of peptide libraries, which must be mounted on hard surfaces. To test their new library approach, the researchers collected blood samples from 40 healthy people and 45 people who had been diagnosed with celiac disease. They purified antibodies from the blood samples, then labeled antibodies from half the celiac patients with a green fluorescent dye and the rest of the patients’ antibodies with a red dye. They then mixed the peptide-coated bacteria together with all the antibodies, adding five times as many unlabeled antibodies from the healthy subjects to block labeled antibodies from binding to peptides found in people with and without celiac disease. Next, they sorted the cells, collecting only those bacteria displaying both red and green fluorescence. Cells labeled with both dyes, the researchers reasoned, help a peptide that could bind to an antibody found in at least two people, one patient from each group. These antibodies, they say, could be markers for celiac disease. Additional screening of the peptides with antibodies from healthy patients and those with celiac disease, the researchers narrowed the bacterial pool down to six unique peptides, none of which bind to known celiac antibodies. The researchers then measured binding between these peptides and the full suite of antibodies from patients’ blood. Based on that data, they used a statistical analysis to conclude that they could identify correctly 85% of people with celiac disease and 91% of healthy – nearly matching the values of existing diagnostic tests. It remains uncertain whether this approach will permit doctors to diagnose celiac disease at earlier stages than current methods, but the results look promising, and the team remains hopeful. Daugherty says that the method is applicable to other immune disorders, including difficult-to-diagnose illnesses such as lupus, multiple sclerosis, and some cancers. Source: Anal. Chem., 2013, 85 (2), pp 1215–1222. DOI: 10.1021/ac303201d -
Celiac.com 12/10/2012 - In celiac disease, doctors use video capsule endoscopy (VCE) mainly to follow-up on stubborn cases, and to diagnose adenocarcinoma, lymphoma or refractory celiac disease. However, some doctors are suggesting that VCE could replace standard esophagogastroduodenoscopy (EGD) and biopsy in certain circumstances. A team of researchers recently evaluated the use of VCE to diagnose celiac disease in place of esophagogastroduodenoscopy (EGD) and biopsy under certain circumstances. The research team included Matthew S. Chang, Moshe Rubin, Suzanne K Lewis, and Peter H. Green. They are variously affiliated with the Celiac Disease Center, Division of Digestive and Liver Diseases of the Department of Medicine at Columbia University College of Physicians and Surgeons in New York, and with the Division of Gastroenterology and Hepatology of the Department of Medicine at New York Hospital Queens, Weill Cornell Medical College in Flushing, New York. For their study, the team evaluated eight patients with suspected celiac disease who were diagnosed by VCE. Of the eight patients, four underwent EGD and biopsy, with negative biopsy results. Two patients declined the procedure, and two showed contradictory results due to hemophilia and von Willebrand disease. Using VCE, the team found that all patients showed mucosal scalloping, mucosal mosaicism and reduced folds in either the duodenum or jejunum. After treatment with a gluten-free diet, seven patients who participated in follow-up showed improvement in either their blood tests, or their presenting clinical symptoms. From this small study, the team concludes that VCE and the observation of the classic mucosal changes of villous atrophy may replace biopsy as the mode of diagnosis for celiac disease in patients who either decline EGD, or show contradictory results, or in suspect patients with negative duodenal biopsy. They encourage further study to determine the role and cost of using VCE to diagnose celiac disease. Source: BMC Gastroenterolohy. 2012;12(90)
-
Celiac.com 03/19/2012 - A clinical gastroenterology research team recently weighed in on the practice of using weight as a factor to screen for celiac disease. They are calling for doctors to ignore body-mass when assessing patients for possible celiac disease screening. The team was made up of Fabio Meneghin, Dario Dilillo, Cecilia Mantegazza, Francesca Penagini, Erica Galli, Giulia Ramponi, and Gian Vincenzo Zuccotti. They are affiliated with the Department of Pediatrics of the Università di Milano Luigi Sacco Hospital in Milan, Italy. The team argues that, more and more, people with clinical celiac disease are presenting widely varied symptoms, while classic gastrointestinal symptoms like diarrhea or failure to thrive are becoming less frequent at diagnosis. In fact, data shows that symptoms once considered to be atypical are now appearing at least as often as classical symptoms related to nutritional malabsorption. Recent studies and case reports show that the expected clinical-condition of malnutrition, typical in a disease where there is a disorder of absorption, is less frequent than in the past. Meanwhile, overweight and even obesity are increasingly common in people with as yet undiagnosed celiac disease. The team points out that obesity has become the most prevalent nutritional disorder among children and adolescent of United States, and also in many European countries. They note that a rates of overweight and obesity have doubled in a single generation. They use these facts to encourage doctors to screen for celiac disease without regard for the patient’s body weight, and thus speeding diagnosis and avoiding possible clinical consequences for patients. For now, their call has been rejected by the editors of Gastroenterology Research and Practice. However, look for this kind of call to be echoed in the future, as data are compiled, and the realities of celiac disease are better understood. Source: Gastroenterology Research and Practice
-
Celiac.com 06/03/2008 - Among the main things doctors look for when they’re trying to make a classic diagnosis of celiac disease are small intestinal mucosal membrane villous atrophy and inflammation. However, the latest research indicates that these criteria are possibly too narrow, leading to a lack of diagnosis and treatment of people with celiac disease. If this turn out to be the case, then far more people than previously imagined may suffer from celiac disease and not even know it. In an effort to find out if present current diagnostic criteria are in fact too narrow, Finnish researchers led by Markku Maki, MD, professor of pediatrics at the University of Tampere, Celiac Disease Study Group, Tampere, Finland, evaluated 145 patients who were presumed to have celiac disease. Just under half (71) of the patients showed positive endomysial antibodies, and out of these only 48 patients met the textbook definition for celiac disease. The research team then split the 23 patients left into two groups. They put the first group on a gluten-free diet for one year, and the second group on a on a standard gluten-inclusive diet for one year. At the end of the year, the doctors conducted follow-up biopsies on all 23 patients. The doctors discovered that the patients who had been on the gluten-free diet did in fact have celiac disease (even though they didn't have any obvious symptoms), and any symptoms that they did have disappeared—they lost their endomysial antibodies and any inflammation that was detected in their intestinal mucosa. On the other hand, the patients in the second group whose diets included gluten showed no such positive changes, and their symptoms continued. The still showed positive endomysial antibodies, along with inflammation of intestinal mucous membrane, and gluten-induced lesions in the small intestine. The study director said that each of the patients on the gluten-free diet had chosen to remain gluten-free thereafter, and that the patients on the gluten-inclusive diet had chosen to eliminate gluten from their diets and over time also became symptom-free—endomysial antibody-free and showed signs of healing of the mucous membrane. Other studies have shown that over time untreated patients who show positive endomysial antibodies may develop the gut injury that is currently required as part of the criteria for diagnosing celiac disease. A greater understanding of the negative effects of untreated or undiagnosed celiac disease, coupled with better testing methods have led to a new strategy that allow doctors to detect celiac disease as early as possible—before any serious damage can occur—this new strategy is likely to be resoundingly welcome among celiac disease sufferers. Hopefully the results of this study and others like it will lead to a new awareness among doctors, and will ultimately lead to better methods for diagnosing celiac disease at an earlier stage. This could ultimately mean less suffering and long term physical damage for many people. Presented at 2009 Digestive Disease Week in San Diego, CA by Dr. Kurppa, a member of Dr. Maki’s research team, on Tuesday, May 20 at 10:30 a.m. Pacific Time in room 10 (San Diego Convention Center).
- 10 comments
-
- celiac
- celiac disease
- (and 4 more)
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8-M):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8-M):














.webp.79fe4ff0953d341e8fcc0a75b227c7ec.webp)