-
Welcome to Celiac.com!
You have found your celiac tribe! Join us and ask questions in our forum, share your story, and connect with others.
-
Celiac.com Sponsor (A1):
Celiac.com Sponsor (A1-M):
-
Get Celiac.com Updates:Support Celiac.com!
Search the Community
Showing results for tags 'endoscopy'.
-
Celiac.com 11/15/2023 - Imagine enjoying your favorite pasta dish one day, and the next day, experiencing mysterious and uncomfortable symptoms like stomach pain, vomiting, fatigue, or skin rashes. What could be causing these problems? One possibility might be celiac disease. Celiac disease is a relatively common autoimmune disorder that affects the small intestine. It's triggered by the consumption of gluten, a protein found in wheat, barley, and rye. When someone with celiac disease eats gluten, their immune system reacts by damaging the lining of the small intestine, which can lead to a wide range of symptoms and complications. Getting the diagnosis correct is important, because celiac disease is often misdiagnosed. Symptoms of Celiac Disease The symptoms of celiac disease can vary greatly from person to person, and some individuals may not experience any symptoms at all. Here are some common signs to watch out for: Digestive Troubles: Symptoms often involve the digestive system, such as diarrhea, constipation, bloating, gas, and abdominal pain. Fatigue: Many people with celiac disease report feeling excessively tired, even after a full night's sleep. Weight Loss: Unintended weight loss can occur due to malabsorption of nutrients caused by intestinal damage. Skin Issues: Some individuals develop skin conditions, itchy rashes, like dermatitis herpetiformis, which is closely linked to celiac disease. Joint Pain: Joint pain and inflammation may affect those with celiac disease. Mood Changes: Mood swings, depression, or anxiety can be related to the condition. Delayed Growth in Children: Celiac disease can hinder proper growth and development in children. Diagnosis of Celiac Disease Getting a proper diagnosis is crucial for managing celiac disease effectively. Here's how doctors typically diagnose it: Blood Tests: Initially, blood tests are done to check for elevated levels of certain antibodies, such as anti-tissue transglutaminase (tTG) and anti-endomysial antibodies (EMA). Higher levels of these antibodies can be a sign of celiac disease. Biopsy: If blood tests indicate celiac disease, a small intestine biopsy may be performed. During this procedure, a tiny sample of the intestinal lining is taken and examined under a microscope. Damage to the lining is a key indicator of the disease. In more and more cases, celiac disease can be diagnosed without biopsy. Treatment of Celiac Disease The primary treatment for celiac disease is a strict gluten-free diet. Once diagnosed, individuals need to eliminate all sources of gluten from their diet, including bread, pasta, cakes, and even certain sauces. This can be challenging, as gluten can hide in unexpected places, so reading food labels and avoiding gluten ingredients is a must. Most people with celiac disease notice significant improvements in their symptoms once they adopt a gluten-free lifestyle. Over time, the intestinal lining often heals, allowing for better nutrient absorption. In some cases, complications of celiac disease may require additional medical attention. For instance, individuals with severe malabsorption may need vitamin and mineral supplements. Dermatitis herpetiformis may be treated with medications. Living with Celiac Disease While a gluten-free diet is the cornerstone of managing celiac disease, it's also essential to be vigilant about cross-contamination. This means avoiding utensils, kitchen appliances, and cooking surfaces that have come into contact with gluten-containing foods. Celiac.com offers numerous forums for discussing celiac disease and gluten-free challenges with other celiacs who can share experience and help guide your celiac and gluten-free journey. Support groups and dietary counselors can be incredibly helpful for those newly diagnosed with celiac disease. They provide practical tips for maintaining a gluten-free lifestyle and offer emotional support during the transition. In conclusion, celiac disease is a common but manageable condition. By recognizing its symptoms, seeking a proper diagnosis, and committing to a gluten-free diet, individuals with celiac disease can lead healthy and fulfilling lives. If you suspect you have celiac disease, don't hesitate to consult a healthcare professional for guidance and testing. Your well-being is worth it!
- 1 comment
-
- biopsy
- blood tests
- (and 7 more)
-
hi guys, i have recently (July) been diagnosed with celiac disease however via blood results my ttg iga was 128 which is ten times over normal and endomysial was a strong positive. I also had high lymphocytes and low vitamin B12. My GP advised due to how high to start a gluten free diet immediately which i did, my bloating, brain fog, bowels etc got how they should be and anxiety also. The Gastro dept have contacted me asking for me to go onto a gluten diet for 8 weeks for a biopsy which i have been glutened and has caused me utter hell in past. My concern is why on celiac foundation website are we told if it is ten times over normal count that pt should not necessarily need an Endoscopy. I have had a MRI due to brain fog, and they had found white matter on my brain that is linked to celiac. PLEASE HELP I HAVE NO IDEA WHAT TO DO, HE JUST TOLD ME TO GO ON GLUTEN DIET NO ADVISORIES NOTHING, EVEN WHEN I AM A STRONG POSITIVE!!!! and i really do not know if it is worth the trauma.
- 18 replies
-
- biopsy
- blood test
-
(and 6 more)
Tagged with:
-
Currently going through the process of eating gluten every day to confirm diagnosis. Have a colonoscopy scheduled on the 27th and trying not to loose hope while eating all this gluten. Breaking out in a rash, brain fog, head aches, joint pain, and of course endless stomach issues and pain. Anyone else on their diagnosis journey? Trying to stay positive and keep going but I really want to just stop eating the big G.
- 1 reply
-
- colonoscopy
- endoscopy
-
(and 1 more)
Tagged with:
-
I ate SO much gluten for the holidays. my family baked croissants every day and I shoveled them in. In the days leading up to the new year I ate lots of pizza, tacos, pastries- typical junk food. January 1st I had to stop. I work as a scientist and I needed to get a lot of paperwork done- so I didn't want to feel like garbage. I mostly completely cut out gluten. 11 days later, today is my endoscopy. There's no way my stomach has healed in that time right? For the past few days I've included small amounts of gluten like in meatloaf or croutons on my salad (I'm in a lot of pain rn). Anyway, what do you think?
-
Celiac.com 06/13/2022 - In 1992 Dr. Michael Marsh developed his "Marsh Classification" system to describe the various stages of microscopic damage to the small intestine (histological changes) seen in those with celiac disease. The original system ranged from 0 - 4, and 3 or higher meant celiac disease, but his system was modified for consistency and reproducibility between pathologists. Today, anyone who has been diagnosed with celiac disease has likely heard about the Marsh classification system. Using the Marsh Classification allows clinicians to accurately measure the full extent of the damage to the villi that line the small intestine, to determine the extent of celiac disease progress and damage. Modified Marsh Classification of histologic findings in celiac disease (Oberhuber) are measured in units of IEL/100 enterocytes, intraepithelial lymphocytes per 100 enterocytes. Current Marsh Classification Marsh Type 0 - Normal; celiac disease highly unlikely. IEL / 100 enterocytes – jejunum <40 IEL / 100 enterocytes - duodenum <30 Normal crypt hyperplasia Normal villi Marsh Type 1 - Seen in patients on gluten free diet (suggesting minimal amounts of gluten or gliadin are being ingested); patients with dermatitis herpetiformis; family members of celiac disease patients, not specific, may be seen in infections. IEL / 100 enterocytes – jejunum >40 IEL / 100 enterocytes - duodenum >30 Normal crypt hyperplasia Normal villi Marsh Type 2 - Very rare, seen occasionally in dermatitis herpetiformis. IEL / 100 enterocytes – jejunum >40 IEL / 100 enterocytes - duodenum >30 Increased crypt hyperplasia Normal villi Marsh Type 3 - Spectrum of changes seen in symptomatic celiac disease. Marsh Type 3a IEL / 100 enterocytes – jejunum >40 IEL / 100 enterocytes - duodenum >30 Increased crypt hyperplasia Mild villous atrophy Marsh Type 3b IEL / 100 enterocytes – jejunum >40 IEL / 100 enterocytes - duodenum >30 Increased crypt hyperplasia Marked villous atrophy Marsh Type 3c IEL / 100 enterocytes – jejunum >40 IEL / 100 enterocytes - duodenum >30 Increased crypt hyperplasia Complete villous atrophy In an effort to simply the Marsh Classification system, the following Simplified Celiac Classification System has been proposed by researchers Corazza, Roberts, and Ensari, which may be much easier and more reproducible. Simplified Celiac Classification System Grade A/Type 1: increased intraepithelial lymphocytes but no villous atrophy. This occurs in those on a gluten-free diet and is likely caused by patients who consume small amounts of gluten due to cross-contamination or in those who cheat on their diets, and in patients with dermatitis herpetiformis, family members of celiacs, and can also be seen in certain infections. Grade B1/Type 2: villi still present but shortened. This level of damage is accompanied by many symptoms associated with celiac disease. Grade B2/Type 3: complete villous atrophy. This level of damage is accompanied by many symptoms associated with celiac disease. To date, there has been no good study data comparing the two systems. Certainly, a simpler, more reproducible Marsh system would make the job of measuring the progress of celiac disease and the gluten-free diet in celiac patients much easier. Stay tuned for more on this and related stories. Read more at stanford.edu.
-
- biopsy
- biopsy results
-
(and 6 more)
Tagged with:
-
Recognizing Celiac Disease Down the Endoscope
William Dickey, PhD, MD posted an article in Autumn 2004 Issue
Celiac.com 05/27/2022 - Among the many symptoms associated with celiac disease, some of the commonest fall into the broad category of “dyspepsia”. These are symptoms more usually attributed to acid reflux from the stomach into the esophagus (heartburn, regurgitation, even difficulty swallowing a.k.a. dysphagia) or to peptic ulcer disease (upper abdominal pain, indigestion, fullness). While we are not entirely sure why celiac disease causes these, often in the absence of typical “bowel” symptoms, we do know how(1) . Studies of the upper gut in celiac disease patients frequently show abnormal motility and peristalsis: the conveyor belt isn’t working properly (The constipation that is often paradoxically a symptom of celiac disease probably has the same basis). So many celiac patients are going to be referred not for small bowel investigation but for upper GI endoscopy, and the gastroenterologist is expecting not celiac disease, but reflux esophagitis, hiatus hernia, gastritis or peptic ulcer disease. Wouldn’t it be nice—and wouldn’t it make life a lot simpler for the so far undiagnosed celiac patient—if the gastroenterologist could spot villous atrophy like these other conditions? The good news is that you can see villous atrophy down an endoscope. Well, some of the time (but more of that later). One of the most exciting developments in my career as a celiac diagnostician was when our museum piece fiberoptic endoscopes were replaced by full color videoscopes. Endoscopy was no longer an uncomfortable (for the endoscopist!) and hurried foray into the upper gut, hunched over with one eye peering down a clouded eyepiece, frantically trying to see everything and get the heck out before the disinfectant fumes wafting up the scope dissolved the glue holding my spectacles together. Instead it became a civilized stroll which ended in a duodenum filling a ten inch TV picture in glorious color. And it became clear to me and many other celiac specialists that the duodenums of celiac patients didn’t look quite right when they were up close and magnified in this way. Abnormalities seen in our patients with villous atrophy(2) include mosaic mucosa (53%), scalloped folds (50%), fold loss (15%) and nodular mucosa (6%) and erosions (small ulcers) in the second part of duodenum in 7%. Occasionally the mucosa is so thin that blood vessels can be seen through it. Although uncommon in celiac disease, the finding of erosions in the second part of duodenum is of particular interest as clinicians may simply flag it up as peptic ulcer disease, even though peptic ulcers usually only affect the first part of duodenum. I’ve seen a few patients who had previously been wrongly diagnosed “peptic” because of this endoscopic feature. So how have these endoscopic markers changed my practice? Around half of my new celiac patients present with dyspepsia and are recognized at endoscopy(3) . One in 60 (twice the background prevalence of celiac disease) patients referred for endoscopy from primary care with dyspepsia are diagnosed celiac because of these markers(4). Often the story is of dyspeptic symptoms which have not responded to ulcer healing drugs—while on a gluten-free diet they disappear magically. There are two caveats regarding endoscopic markers. While villous atrophy in adults is pretty much synonymous with celiac disease in Western Europe, elsewhere it may sometimes indicate other disease, as reported by the New York Group(5) . Secondly, the bad news is that villous atrophy can’t always be spotted. We found that only 74% of villous atrophy cases had endoscopic markers(2) , and as many patients had endoscopy for biopsy because we were expecting to find celiac disease, that figure may be an overestimate of routine practice. The Mayo Clinic found markers in only 59% of celiac patients from a group of anemic patients having endoscopy(6). While 82% of our patients with subtotal or total villous atrophy had one or more endoscopic markers, the yield fell to 58% for partial villous atrophy(7). And as you might expect, I have never seen endoscopic markers in gluten-sensitive patients with milder (Marsh I, Marsh II) histologic abnormalities which have not yet progressed to villous atrophy. So lack of markers does not mean that there is no need to biopsy, particularly in high risk groups like patients with anemia and insulin dependent diabetes. In an ideal world, duodenal biopsy would be a routine part of every upper GI endoscopy, as already proposed by Peter Green and Joe Murray(8). In practice, particularly in the good ol’ underfunded UK National Health Service that I work for, this would have very significant resource implications. I suspect such a policy—duodenal biopsies taken at every endoscopy— implemented without a major funding initiative on my side of the Atlantic might find our already overworked and undervalued histopathologists under the cars of gastroenterologists furiously cutting through their brake lines. In the meantime, and until the New Jerusalem of routine duodenal biopsy during endoscopy is constructed, recognition of the endoscopic markers of celiac disease, while not foolproof, represents a pragmatic way of diagnosing celiac patients who present with dyspepsia. References: Bassotti G, Castellucci G, Betti C et al. Abnormal gastrointestinal motility in patients with celiac sprue. Dig Dis Sci 1994; 39: 1947-54. Dickey W, Hughes DF. Erosions of the second part of duodenum in patients with villous atrophy. Gastrointestinal Endoscopy 2004; 59: 116-118. Dickey W. Diagnosis of coeliac disease at open access endoscopy. Scandinavian Journal of Gastroenterology 1998; 33: 612- 5. Dickey W, Hughes DF. Prevalence of celiac disease and its endoscopic markers among patients undergoing routine endoscopy. American Journal of Gastroenterology: 1999; 94: 2182-6. Shah VH, Rotterdam H, Kotler DP, Fasano A, Green PHR. All that scallops is not celiac disease. Gastrointest Endosc 2000; 51: 717-20. Oxentenko AS, Grisolano SW, Murray JA et al. The insensitivity of endoscopic markers in celiac disease. Am J Gastroenterol 2002; 97: 933-8. Dickey W, Hughes DF. Disappointing sensitivity of endoscopic markers for villous atrophy in a high-risk population: implications for celiac disease diagnosis during routine endoscopy. Am J Gastroenterol 2001; 96: 2126-8. Green PHR, Murray JA. Routine duodenal biopsies to exclude celiac disease? Am J Gastroenterol 2003; 58: 92-5.-
- biopsy
- celiac disease
- (and 7 more)
-
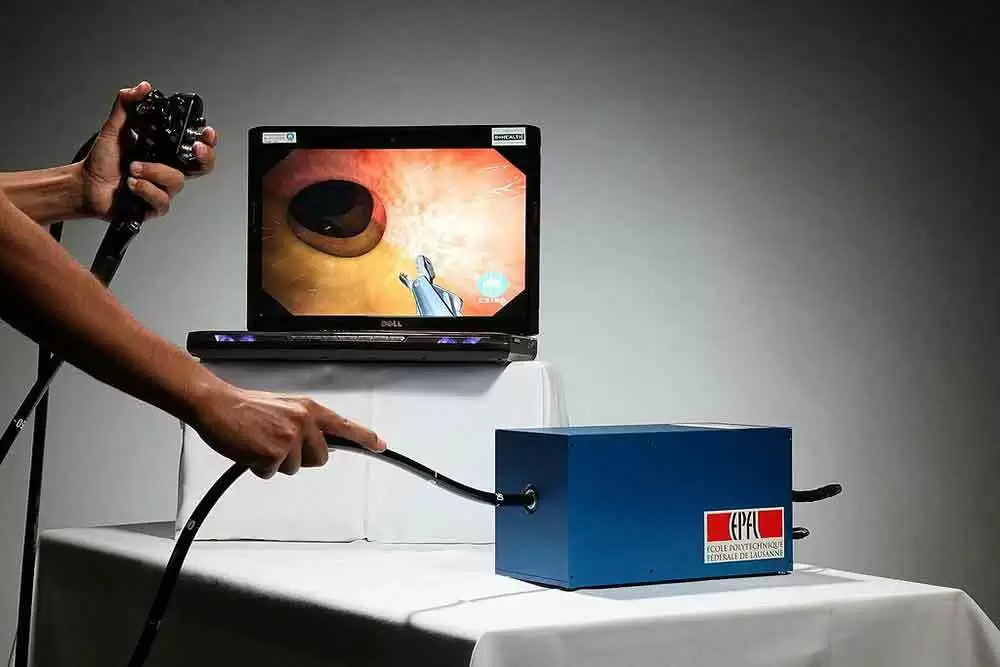
Celiac.com 04/16/2021 - When undergoing an evaluation for possible Celiac disease or gluten sensitive enteropathy doctors usually recommend an upper endoscopy with small intestinal biopsy. What that is and why it is recommended may not be clear to many people who are facing the decision of whether to undergo the procedure themselves or whether to subject their child to this exam. What is an endoscopy and how is it done? During upper endoscopy a thin flexible tube, about the diameter of a fat pencil, is passed in the mouth down the upper gastrointestinal tract. This tube has a video chip on its tip. From the mouth it is advanced down the esophagus, or inside a feeding tube, into the stomach. It is then advanced into the first part of the small intestine known as the duodenum. Thus, upper endoscopy is also known as esophagogastroduodenoscopy or EGD for short. The scope has internal channels for flushing water, suctioning secretions and passing instruments that can obtain pinch biopsy samples of tissue for microscopic examination. The scope dials control internal cables that allow the tube to be turned up/down and right/left at the tip. Do you feel and endoscopy or remember it? Typically, people undergoing the exam in the U.S. are sedated with medication. These medications are similar to Valium. They have a good amnesia and relaxing effect and are called midazolam or versed and are usually combined with a narcotic pain medication like meperidine (Demerol) or Fentanyl. The result is a sort of drowsy twilight amnesia. Lately, a very short-acting intravenous sedative, called propofol (diprovan) is increasingly being used for deeper sedation or general anesthesia. Occasionally, usually in very young children or people with severe lung problems, general anesthesia is required. The exam is usually not felt or remembered because of the medications. What is examined and how well is the lining is seen? Celiac disease affects the upper portion of the small intestine, in the two sections known as the duodenum and jejunum. The examination of the small intestine is usually limited to the first section, termed the duodenum, though occasionally the second section known as the jejunum may be reached especially when a longer endoscope is used. The video images are very high resolution with the latest endoscopes and may have a magnification and color contrast mode to detect very subtle signs of damage of the small intestine. What are the typical endoscopy findings? The characteristic appearance of the surface of the small intestine in celiac disease includes superficial ulcerations that are commonly linear, flattening of the folds, notching or scalloping of the folds and a mosaic-like pattern. However, the surface may appear normal and only under microscopic examination of samples will the lining show signs of gluten-induced injury. What are intestinal biopsies? What are their limitations? What can be missed? Samples of small intestine are obtained with biopsy forceps that consist of tiny jaws with cups that permit pinching off samples of the intestinal lining. This is painless and very safe. The samples are placed in a preservative solution and sent to a pathology lab. The tissue is then processed, embedded in paraffin wax, cut into thin slices and mounted on a microscope slide. The slides are stained before being examined under the microscope by a pathologist. Small intestine injury from gluten may be patchy. Therefore, several samples are recommended. A minimum of 4 pieces and preferably 8 to 12 samples should be obtained to avoid missing microscopic signs of Celiac disease. What does the pathologist look for on the slides to determine if there is Celiac disease or gluten injury? The pathologist examines the slide for evidence of damage or injury characteristic of gluten sensitivity. Occasionally special stains are required to see signs of irritation known as inflammation. Inflammation in the gut is characterized by an increased number of a type of white blood cells. For Celiac disease the characteristic white blood cell involved in gluten-induced intestinal injury are called lymphocytes. In early celiac and gluten sensitivity without celiac disease, the biopsy may be normal and the diagnosis may not be established by intestinal biopsy without special stains or, in the research setting, by electron microscopy. Summary The procedure of endoscopy is safe, painless, and very helpful for confirming the diagnosis of celiac disease while excluding other upper intestinal disorders. However, the main drawback of endoscopy is that nearly everyone must have sedation to tolerate the exam and it can be expensive if not fully covered by the patient’s insurance. Furthermore the biopsies may not confirm the diagnosis. If the biopsy is normal, misread as normal, or is borderline, the diagnosis of celiac disease is neither confirmed nor excluded. Sometimes, celiac disease is diagnosed by endoscopic biopsy in people who either have normal blood tests or as an incidental finding in those undergoing endoscopy for other reasons. When the biopsy is abnormally classic for Celiac disease and the blood tests are negative but the patient responds to a gluten-free diet, the term seronegative (blood test negative) celiac disease is often used. Fear or confusion about endoscopy should not prevent anyone who is suspected of having celiac or gluten sensitivity from undergoing endoscopy.
-
To All, I found this new research on the Pill Cam being used to diagnose Celiac's. I know Scott will probably do an article on it soon....but I didn't see a reason to wait....to get some feedback on it. Entitled "New Evidence Supports Using Capsule Endoscopy for Complicated Celiac Disease: 40% of lesions were found distal to the ligament of Treitz and would have likely been missed by standard endoscopy" https://www.medpagetoday.com/reading-room/aga/lower-gi/89840 What do you think is this a better method than Endoscopy to use to be diagnosed as a Celiac? Is this the end of Endoscopy? It looks like it could at least cut down on unnecessary repeated endoscopy's.... How long do you think it would be before medical practitioners begin using this new method to discover Villous Atrophy? I hope this is helpful but it is not medical advise. Posterboy,
-
Hello, I just tested positive for celiac in two different blood panels and have a vitamin A deficiency and was referred for an endoscopy. Does anyone know if false positives are common and do people usually go gluten free as soon as the endoscopy is done? I have a one month wait between the endoscopy and seeing the GI and don't want to be damaging my body more if I have it. Thanks.
-
Hi there, I’m due for an endoscopy (currently no longer have a date due to COVID) and am just very nervous about what to expect. I have quite a low pain tolerance and an awful gag reflex, would it be worth me requesting sedation for the procedure or is it not that bad? I’m the first member of my family (that I know of) to have one so just don’t know what to expect. Any guidance would be greatly appreciated (please be brutally honest)
-
Celiac.com 03/11/2020 - Researchers don't have a very good understanding about the connection between symptoms, blood tests, and the results of small bowel capsule endoscopy (SBCE) in celiac patients. Better understanding such connections will help to figure out whether symptoms and blood tests can determine the severity and extent of disease using SBCE. A team of researchers recently set out determine if symptoms and blood tests can determine the severity and extent of disease using SBCE. The team included Stefania Chetcuti Zammit, David S. Sanders and Reena Sidhu, of the Academic Unit of Gastroenterology, Royal Hallamshire Hospital, Sheffield, UK. The research team enrolled newly diagnosed celiac patients, and noted Information on SBCE, along with symptoms and indications upon presentation, blood test results, and levels of disease histology in the duodenum. A total of 60 newly diagnosed celiac patients were included, who averaged about 45 years of age. Older patients and those with iron deficiency anemia showed more small bowel involvement. Nearly 40% of patients with weight loss had small bowel involvement beyond the duodenum, compared to those without. Patients with iron deficient anemia and weight loss were much older at the time of diagnosis. There was no significant association between blood antibodies and amount of small bowel mucosa damage. Patients with higher Marsh scores on duodenal histology showed more widespread small bowel involvement. This is the largest assessment of SBCE in newly diagnosed celiac disease so far conducted. The data reveal that older patients showed more widespread celiac disease on SBCE upon diagnosis. Aside from weight loss and iron deficiency anaemia, symptoms and blood test results were independent of the team's findings. Read more in the Eur J Gastroenterol Hepatol 31: 1496–1501
-
- capsule endoscopy
- celiac disease
-
(and 5 more)
Tagged with:
-
Celiac.com 02/26/2020 - Patients with established celiac disease can present with signs and symptoms requiring small bowel capsule endoscopy (SBCE) to assess for persistent disease beyond the duodenum and to rule out complications. There is limited data celiac disease and histology, clinical and serological parameters as they reflect the extent of celiac disease on small bowel capsule endoscopy. A team of researchers recently set out to assess the role of small bowel capsule endoscopy in established celiac disease, by looking at the relationship between symptoms, celiac disease serology and Marsh classification of disease and extent of disease on small bowel capsule endoscopy in patients with established celiac disease. The team included S. Chetcuti Zammit; M. Kurien; D.S. Sanders; and R. Sidhu. They are associated with the Academic Department of Gastroenterology, Royal Hallamshire Hospital, Sheffield Teaching Hospitals in Sheffield, UK. The researchers conducted small bowel capsule endoscopies on 100 known celiac patients, and 200 control subjects. The results were reviewed by a team of experts. The team noted the progression of disease on small bowel capsule endoscopy, celiac disease findings and small bowel transit times. The gold standard for diagnosing celiac disease is a duodenal histology, with D2 and Marsh 3a or above. The team's results show that small bowel capsule endoscopy can spot active disease with over 87% sensitivity, and 89% specificity. Univariate analysis showed that the degree of affected small bowel mucosa correlates with the patient's age at small bowel capsule endoscopy, albumin, and hemoglobin, Marsh score of histology from the duodenal bulb (D1) and the second part of the duodenum, and refractory celiac disease on histology. Multiple regression analysis, albumin and Marsh score of histology (D1) all showed vitamin B12 and folate levels to be measurably significant. Celiac patients with complications including those with refractory celiac disease show much more affected SB mucosa. This is the first time a study has shown a connection between degree of disease and levels of malabsorption for duodenal histology markers, such as folate levels and vitamin B12, along with the complications of celiac disease. Among other findings, the study shows that: small bowel capsule endoscopy reveals macroscopic changes in celiac disease patients with a high level of sensitivity; low levels of vitamin B12 and folate due to malabsorption match the severity of celiac disease; celiac patients with a normal small bowel capsule endoscopy result are not likely to have significant active disease. Read more in Clinics and Research in Hepatology and Gastroenterology
- 1 comment
-
- b12
- capsule endoscopy
-
(and 6 more)
Tagged with:
-
Celiac.com 02/10/2020 - There are no articles in the medical literature about the role of repeat small bowel capsule endoscopy (SBCE) in patients with refractory celiac disease (RCD) following treatment with steroids and/or immunosuppressants. A team of researchers recently set out to compare the findings on SBCEs from a group of 23 patients with histologically proven RCD against the results of 48 patients with uncomplicated celiac disease. All patients had concurrent duodenal histology and serology taken at the time of SBCE. The team included Stefania Chetcuti Zammit, David S. Sanders, Simon S. Cross, and Reena Sidhu. They are variously associated with Academic Department of Gastroenterology, Royal Hallamshire Hospital, Sheffield Teaching Hospitals, Sheffield; and the Academic Unit of Pathology, Department of Neuroscience, Faculty of Medicine, Dentistry & Health, The University of Sheffield, Sheffield, UK. SBCE revealed refractory celiac disease patients to have greater mucosal involvement than patients with uncomplicated celiac disease. After steroid and/or immunosuppressant treatment, refractory celiac disease patients showed an improvement in the extent of affected small bowel mucosa. Statistically, both histology and serology were the same for first and second SBCE in refractory celiac disease patients. The study data indicates that SBCE is useful in documenting the degree of mucosal involvement in refractory celiac disease patients. The team notes that this is the first study to demonstrate the value of a second look SBCE to assess the degree of improvement in celiac disease in the small bowel following treatment. However, more study is needed to more firmly establish these results. Read more in J Gastrointestin Liver Dis, March 2019 Vol. 28 No 1: 15-22
- 1 comment
-
- capsule endoscopy
- celiac
- (and 6 more)
-

FDA Warns of Deadly Duodenoscope Contamination Rates
Jefferson Adams posted an article in Additional Concerns
Celiac.com 06/03/2019 - In 2015, the FDA ordered duodenoscope makers Olympus, Fujifilm, and Pentax to conduct post-market surveillance studies to determine how infections were being transmitted, and to assess the factors that may be contributing to the problem. Interim results from those FDA–mandated studies show unacceptably high contamination rates after reprocessing, with deaths and infections as a result, the FDA said today. The agency said three deaths in the United States in 2018 were likely due to contaminated duodenoscopes. "That's three deaths too many," Jeff Shuren, MD, director of the Center for Devices and Radiological Health, said in a statement. The problem first surfaced in 2013, when the FDA became aware that reprocessed duodenoscopes were transmitting multidrug-resistant bacteria. In 2015, when the sampling studies were ordered, the FDA expected total contamination rates for any type of organism of "less than 1% or as close to zero as possible for duodenoscopes," he added. However, results from studies released in December 2018 show a 3% contamination rate for "high-concern" bacteria, such as Escherichia coli and Staphylococcus aureus, which can cause deadly infections. However, the latest results show that up to 5.4% of all properly collected samples tested positive for "high-concern" organisms, "which is significantly higher than the earlier results reported," Shuren said. The numbers from 2018 also show that medical device reports (MDRs) of patient infections and device contamination have continued to roll into the FDA. A review of 205 MDRs received between October 15, 2018, and March 31, 2019, includes 45 reports of patient infection, one report of patient exposure, and 159 reports of device contamination, in addition to the deaths. The FDA is "continuing to evaluate the benefit-risk profile of these devices, and we'd like to see strong evidence that proper cleaning and reprocessing can virtually eliminate any bacteria residue that can spread infections. Currently, that evidence is lacking, and we're considering what additional regulatory actions may be necessary," said Shuren. The takeaway here is to be vigilant, and speak with your doctor in advance of any procedure involving a duodenoscope. Ask what can be done to mitigate the risk. Demand a new duodenoscope if necessary.-
- celiac disease
- duodenoscope
-
(and 5 more)
Tagged with:
-
Hi everyone, this is my first ever post, so I'm exciting to get to know people here. A bit of background about me... I’ve had problems for around 20 years with things like bloating, stomach doing the Mexican wave, excessive wind, abdominal pain, migraines up to 5 days a week, balance problems, feeling/being sick, depressive, anxiety, acne, itchy blister like rash on feet, hands and face, heartburn, joint paint in hips and back so bad I often can’t stand up for long or can’t stand up straight. I have tingles in my hands and feet and legs. I have a shooting nerve pain from my head/neck down my arm. Heart goes fast & heart palpitations, I can swell up. Struggle breathing. Constipation and diarrhoea. Mucus in stools. Tinnitus. Stomach aches. Brain fog. Tired. The list goes on. Last year I couldn’t take anymore and as I was fed up with feeling so sick all the time. The NHS told me I was lactose intolerant, but I never felt better, so I paid to see a Dietitian, who is incredible. She told me to give up dairy and soya and I instantly started feeling better. She said I had an dairy and soya allergy. Fast forward 10 months and I still have the underlying problems with wind, bad abdominal pain, bloating, acne, blistery itchy rashes, (my face was completely out of control with this strange red/blistery rash) migraines just ones a week (I feel I am blessed in comparison to what I was), heartburn, stomach aches, stomach moves up and down, balance problems, tingles in my hands and feet, stabbing nerve pain from neck to arm, tinnitus, joint problems, mucus, depression, heart palpitations. I have recently been told I have SIBO (small intestine bacteria overgrowth). I have been on the low FODMAP fruit and veg diet, which did nothing. By pure accident I took out wheat from my diet and suddenly realised I was feeling better, so my dietitian told me to go gluten free, which I did for 5 weeks. My skin had never been so clear. My face looked different. Stomach stopped bloating, wind improved, back ache/hip joints improved, but still not great, depression lifted, heart palpitations gone, felt so energetic and happy, heart burn and balance problems gone. I then decided to go back on wheat as I want to get tested for celiac, which I am on the waiting list for. I shouldn’t have come off it! Going back on gluten, my skins rubbish again, etc etc etc. Everything has come back, but my stomach pain isn’t as bad as it was. I am also being tested for inflammatory bowel disease as I have blood in my stools at times along with the mucus. I think that will be negative though. My question is, my symptoms were made even worse when I was on dairy and soya, in fact, I am terrified of them. My dietitian thinks that the dairy and soya allergy and SIBO could be caused by gluten. Does anyone know that to be tested if I should really have dairy and soya in my diet? I have seen lots of people with gluten problems, also have dairy problems, but I’m guessing most of these people worked this out after they cut out gluten. Just wondered if anyone else had experience with this? Also, with my symptoms, would you bother finding out if you were celiac as an endoscopy seems a lot to go through to find out all is fine. Really appreciate any replies. Thanks
-
I have my Endoscopy -finally- scheduled for February 5th. Long road with some uninformed doctors. I've been gluten-free/DF for about 3 months. I know I have to do a Gluten challenge. Should I start today? How much Gluten per day Should I be having? And a month is enough for the endoscopy correct? How long do results typically take? My follow up with the doctor is February 20th, not sure it's enough time. And should I stick with eating gluten until this check up? Also, should I go ahead and eat dairy again as well? I know it's definitely a problem because after accidentally having it recently I had some reactions. Or Should I mostly be concerned with getting the Gluten in my system? Sorry for so many questions Thank you!!
- 5 replies
-
- dairy free
- endoscopy
-
(and 2 more)
Tagged with:
-
Celiac.com 08/30/2018 - Celiac disease is a disorder characterized by a clinical syndrome of intestinal malabsorption and a characteristic though not specific histological lesion consisting in total, subtotal or partial small-bowel villous atrophy (predominating in the proximal segments). A correct gluten-free diet results in clinical and histological improvement(1,2). It has become increasingly apparent that the prevalence of celiac disease is higher than previously thought, and that this is mainly because of increasing awareness of atypical, mildly symptomatic, or silent cases(3). Therefore, many patients have upper gastrointestinal endoscopy as an initial investigation, which provides an opportunity to perform a biopsy in the second portion of the duodenum. The role of endoscopy in diagnosing celiac disease It has long been known that celiac disease can produce changes in the appearance of small intestine on barium contrast radiographs, one such change being so-called “loss” of duodenal folds. However, over the last two decades it has been recognized that a number of changes in the duodenum clearly associated with celiac disease can be identified endoscopically. Because it is now understood that the manifestations of celiac disease are wide and variable, and that the disease is more common than recognized in the past, the clinical significance of these endoscopic observations has been greatly amplified. Awareness of these endoscopic features may alert the endoscopist to the presence of celiac disease and the need for duodenal biopsies in patients undergoing endoscopy for symptoms unrelated to the disease as well as those with vague, non-specific manifestations. The endoscopic features in the duodenum that are well-established as markers for celiac disease include: loss of folds; scalloping of folds; mucosal mosaic pattern; whilst less commonly described findings include a visible vascular pattern and micronodularity in the duodenal bulb. 1. Loss of folds “Loss” of folds is defined as an obvious reduction in height or number of folds in the second portion when viewed with maximal air insufflation. The sensitivity and specificity of this marker range from 73 to 88% and from 83 to 97% respectively (4,5). 2. Scalloping of duodenal folds Scalloping occurs when multiple grooves run over the apex of a duodenal fold. Grooves in the mucosa between folds have also associated with celiac disease and likely a manifestation of the same process that leads to scalloping. The sensitivity and specificity of this marker are 88% and 87% respectively (6,7). 3. Mucosal mosaic pattern Mucosal mosaic pattern may be recognized both in the duodenal bulb and in the second portion of the duodenum, and its assessment may be easily performed by chromoendoscopy. Unfortunately, the sensitivity of this marker is quite low (57%) (8). 4. Micronodularity in duodenal bulb This marker is quite frequent in childhood and adolescent patients, but it can be also recognized in young adults 9-11. 5. Visible vascular pattern This marker describes a prominence of underlying duodenal blood vessels in patients with celiac disease. Unfortunately, this is the least sensitive endoscopic marker in all studies in which it was specifically evaluated (6,12,13). All these markers are helpful in recognising celiac disease. Moreover, in some cases specific endoscopic features can be associated with specific histological damage and may be associated with the clinical form of the disease. We found in fact that endoscopic appearance of the duodenum may be predictive of histological damage grading. Moreover, we showed that in young patient with subclinical/silent celiac disease there is a greater probability of finding slight/mild endoscopic abnormal/mild histological damage (11). Unfortunately, an endoscopic marker suspected for celiac disease itself is not specific for celiac disease. For example, looking at scalloping, Shah, et. al., described 13 cases in which scalloping of duodenal folds was not caused by celiac disease but due to other causes (HIV-related infection, tropical sprue, giardiasis, eosinophilic gastroenteritis)(14). On the other hand, the presence of one or more endoscopic markers increases the sensitivity and specificity ranging from 87.5 to 94% and from 99 to 100% respectively (12,15). There is non-existing classification of endoscopic lesions in celiac disease. However, I think that it may be graded according to some simple considerations. Celiac disease is considered a crianial-caudal disease which affects primarily the proximal segments (first the duodenal bulb and then the second and third duodenal portions) and then the distal segments of the small bowel (first jejeunum and then the ileum). Therefore, we may hypothesize that endoscopic damage occurs first in the duodenal bulb and then in the distal tracts of the duodenum. For this reason, and according to other endoscopists in Italy, I proposed the following classification in 2002(11): a. Slight/mild endoscopic damage: micronodular bulb, granular mucosa of the second duodenal portion, scalloping of duodenal folds, reduction of duodenal folds; b. Severe damage: “mosaic” pattern of the duodenal mucosa, visible vascular pattern, loss of duodenal folds. The effectiveness of this grading system was confirmed in the same study. In fact we found that the so-called “slight-mild endoscopic damages” seen at endoscopy was associated with a mild-moderate histological damage (p<0.005), while the so-called “severe endoscopic damages” was related to severe histological damage (p<0.0005). Unfortunately, no Consensus Conference on celiac disease has discussed this problem yet. New endoscopic methods Several new endoscopic techniques have been recently developed to increase the sensitivity and specificity of endoscopy in diagnosing celiac disease. a. “Immersion” technique. The “immersion” technique consists in observing duodenal mucosa using a high-resolution, high-magnifying (x2) videoendoscope that observes the villous architecture with a water film. This approach seems to be effective in allowing the visualization of duodenal villi and the detection of total villous atrophy(16). A recent study found that this approach is highly accurate in detecting total villous atrophy in suspected celiac cases, and it seems both accurate and cost-sparing to diagnose celiac disease in subjects with marked duodenal villous atrophy, having a sensitivity, specificity, and positive and negative predicting values of 100%17. Moreover, this approach also seems to be effective in detecting patchy villous atrophy in celiac patients with patchy lesions (18). b. Zoom endoscopy This technique provides a very impressive magnification capability of x115. This approach may allow the macroscopic detection of unrecognised villous atrophy in patients with unsuspected celiac disease. Badreldin, et. al., found recently that zoom endoscopy may be valuable in assessing degree of villous atrophy, having a positive predicting value of 83% and a negative predicting value of 77% in detecting villous atrophy (19). c. Double-balloon endoscopy (DBE) This technique will become probably the best endoscopy technique in investigating small bowel. It allows high-resolution visualization, biopsies and therapeutic interventions in all segments of the GI tract. DBE is a safe and feasible diagnostic and therapeutic tool for suspected or documented small-bowel diseases. However, it requires a long time for small bowel exploration (about 70 minutes from the oral route and about 90 minute from the anal route) and requires expertise personnel to obtain better results 20. At present, the best candidates for the procedure appear to be those with obscure GI bleeding. d. Wireless capsule endoscopy Celiac disease is an inflammatory disease that involves the entire small intestine. Even in the 1960s was documented, by using peroral biopsies, that the inflammatory atrophic process can extend a variable distance down the small intestine, not uncommonly involving the ileum(21). These data have been recently confirmed by endoscopic studies, that found ileal inflammatory changes predicting villous atrophy in duodenal biopsy specimens(22). Wireless capsule endoscopy is a new effective and easy method to investigate small bowel. The M2A video capsule endoscope (Given Imaging LTd; Yokneam, Israel) is a wireless capsule (11 mmx27 mm) comprised a light source, lens, CMOS imager, battery and a wireless transmitter. The slippery out side coating of the capsule allows easy ingestion and prevents adhesion of intestinal contents, while the capsule moves via peristalsis from mouth to anus. The battery provides seven to eight hours of work in which the capsule photographs two images per second (between 50,000-60,000 images all together), which are transmitted to a recorder which is worn on the belt. The recorder is downloaded into a computer and seen as a continuous video film. Since its development additional support systems have been added, a localization system, a blood detector and a double picture viewer. All of this is intended to assist the interpreter of the film and to shorten the reviewing period. The full range of indications for CE became apparent with time. The initial device was invented to address for a better diagnostic tool for small bowel pathologies (such as obscure gastrointestinal bleeding or Crohn’s disease)(23). In light of this high specificity for the diagnosis of small bowel diseases, it is considered that capsule endoscopy may be of value in the diagnosis of celiac disease for patients with a positive endomysial or tissue transglutaminase antibody and who are unable to or unwilling to undergo EGDscopy(24). The very important limit of this new technique in celiac disease is represented by the absence of histological-proven damage. It is recognised that the endoscopic signs of villous atrophy are not sensitive for the lesser degrees of villous atrophy, so partial villous atrophy may be missed by this approach(13). On the other hand, I think that the patients who appear to be ideal candidates for capsule endoscopy are those patients who fail to respond to a gluten-free diet, or who develop alarm symptoms while on a gluten-free diet. These patients often undergo extensive radiologic, and sometimes, surgical evaluation, because of concern for the development of complications (such as lymphoma(25,26) or ulcerative jejunitis(27). It is clear that lesions detected by capsule endoscopy in this high-risk group will require further evaluation of these abnormalities through biopsy. Capsule endoscopy may thus be used to select patients to undergo enteroscopy(28) or, more probably in the near future, double-balloon endoscopy(29). The role of endoscopy in the follow-up of celiac disease Data on small-intestinal recovery in patients with celiac disease are scarce and contradictory. This is especially the case for adult patients, who often show incomplete histological recovery after starting GFD. On the other hand, there are very few data about the endoscopic recovery on GFD. We recently conducted a two-year prospective study on 42 consecutive adults with newly diagnosed celiac disease. All the patients underwent EGDscopy and small-bowel biopsy. A normal endoscopic appearance (absence or mucosal irregular findings, normal duodenal folds) was found in 76.2% after two-year on a GFD. Subdividing the patients according to age, patients aged from 15 to 60 years showed significant improvement within 12 months but faster in patients in patients <45 years, whereas the improvement in endoscopic findings in patients older than 60 years was not statistically significant even 24 months after starting GFD. On the contrary, histological recovery was much more slower, since only younger patients (5-30 years) showed significant improvement of histology within 24 months(30). These data showed for the first time that endoscopic recovery is faster than histological recovery after starting GFD. Conclusive Advice A number of studies have demonstrated a strong correlation between the endoscopic duodenal findings and celiac disease. Furthermore, absence of specific features suspected from celiac disease does not exclude celiac disease and specimens should always be obtained when there is a suspicion that the disease may be present. For this reason, capsule endoscopy should be not recommended as first endoscopic step in searching celiac disease, but it may be best used to recognize endoscopic recovery and to exclude complication in celiac patients on GFD. The last question is: How long should we continue with endoscopic and histological follow-up? Looking at the results recently obtained from our group, my advice on follow-up could be summarized as follows: patients aged under 30 years should undergo endoscopic/histological assessment after one year; patients aged 30-45 years should be reassessed after two years; and patients aged 50 years and over should be reassessed after two years, including an immunohistological assessment to exclude refractory celiac disease. References: 1) Martucci S, Biagi F, Di Sabatino A, Corazza GR. Coeliac disease. Digest Liver Dis 2002;34 (suppl. 2): S150-S153. 2) When is a celiac a celiac? Report of a working group of the United European Gastroenterology Week in Amsterdam, 2001. Eur J Gastroenterol Hepatol 2001;13: 1123-8. 3) Tursi A, Giorgetti GM, Brandimarte G, Rubino E, Lombardi D, Gasbarrini G. Prevalence and clinical presentation of subclinical/silent coeliac disease in adults: an analysis on a 12-year observation. Hepato-gastroenterol 2001; 39: 462-4. 4) Brocchi E, Corazza G, Caletti G et al. Endoscopic demonstration of loss of duodenal folds in the diagnosis of celiac disease. N Engl J Med 1988;319: 741-4. 5) Mc Intere AS, Mg DP, Smith JA , Amoah J, Long RG. The endoscopic appearance of duodenal folds is predictive of untreated adult celiac disease. Gastrointest Endosc 1992;38: 148-51. 6) Corazza GR, Caletti GC, Lazzari R et al. Scalloped duodenal folds in childhood celiac disease. Gastrointest Endosc 1993; 29: 543-5. 7) Smith AD, Graham I, Rose JD. A prospective endoscopic study of scalloped folds and grooves in the mucosa of the duodenum as sign of villous atrophy. Gastrointest Endosc 1998;47: 461-5. 8) Stevens FM, McCarthy CF. The endoscopic demonstration of coeliac disease. Endoscopy 1976;8: 177-80. 9) Brocchi E, Corazza GR, Brusco G, Mangia L, Gasbarrini G. Unsuspected celiac disease diagnosed by endoscopic visualization of duodenal bulb micronodules. Gastrointest Endosc 1996;4: 610-1. 10) Vogelsang H, Hänel S, Steiner B, Oberhuber G. Diagnostic duodenal bulb biopsy in celiac disease. Endoscopy 2001;33: 336-40. 11) Tursi A, Grandimarte G, Giorgetti GM, Gigliobianco A. Endoscopic features of celiac disease in adults and their correlation with age, histological damage, and clinical form of the disease. Endoscopy 2002;34: 787-92. 12) Niveloni S, Fiorini A, Dezi R et al. Usefulness of videoduodenoscopy and vutal dye staining as indicators of mucosal atrophy of celiac disease: assessment of interobserver agreement. Gastrointest Endosc 1998;47: 223-9. 13) Dickey W, Hughes D. Disappointing sensitivity of endoscopic markers for villous atrophy in a high-risk population: inplication for celiac disease diagnosis during routine endoscopy. Am J Gastroenterol 2001;96: 2126-8. 14) Shah VH, Rotterdam H, Kjotler DP, Fasano A, Green PH. All that scallops is not celiac disease. Gastrointest Endosc 2000;51: 717-20. 15) Dickey W, Hughes D. Prevalence of celiac disease and its endoscopic markers among patients having routine upper gastrointestinal endoscopy. Am J Gastroenterol 1999;94: 2182-6. 16) Cammarota G, Martino A, Pirozzi GA et al. Direct visualization of intestinal villi by high-resolution magnifying upper endoscopy: a validation study. Gastrointest Endosc 2004;60: 732-8. 17) Cammarota G, Cesaro P, Martino A et al. High accuracy and cost-effetciveness of a biopsy-avoiding endoscopic approach in diagnosing celiac disease. Aliment Pharmacol Ther 2006;23: 61-9. 18) Cammarota G, Martino A, Di Caro S et al. High-resolution magnifying upper endoscopy in a patient with patchy celiac disease. Dig Dis Sci 2005;50: 601-4. 19) Badreldin R, Barrett P, Wooff DA, Mansfield J, Yiannakou Y. How good is zoom endoscopy for assessment of villous atrophy in coeliac disease? Endoscopy 2005;37: 994-8. 20) Di Caro S, May A, Heine DG, Fini L et al. The European experience with bouble-balloon enteroscopy: indications, methodology, safety, and clinical impact. Gastrointest Endosc 2005;62: 545-50. 21) MacDonald WC, Brandiborg LL, Flick AL et al. Studies of celiac sprue. IV. The response of the whole length of the small bowel to a gluten-free diet. Gastroenterology 1964;47: 573-89. 22) Dickey W, Hughes DF. Histology of the terminal ileum in coeliac disease. Scand J Gastroenterol 2004;39: 665-7. 23) Eliakim R. Wireless capsule video endoscopy: three years experience. World J Gastroenterol 2004;10: 1238-9. 24) Cellier C, Green PH, Collin P et al. The role of capsule endoscopy in coeliac disease: the way forward. Endoscopy 2005;37: 1055-9. 25) Green PH, Fleichauer AT, Baghat G et al. Risk of malignancy in patients with celiac disease. Am J Med 2003;115: 191-5. 26) Cellier C, Delabasse E, Helmer C et al. Refractory sprue, coeliac disease and enteropathy-associated T-cell lymphoma. French Coeliac Disease Study Group. Lancet 2000;356: 203-8. 27) Green JA, Barkin JS, Gregg PA et al. Ulcerative jejunitis in refractory celiac disease: enteroscopic visualization. Gastrointest Endosc 1993;39: 584-5. 28) Gay G, Delvaux M, Fassler I. Outcome of capsule endosocpy in determining indication and route for push-and-pull enteroscopy. Endoscopy 2006;38: 49-58. 29) Yamamoto H, Kita H, Sunada K et al. Clinical outcomes of double-baloon endoscopy for the diagnosis and treatment of small-intestinal diseases. Clin Gastroenterol Hepatol 2004;2: 1010-6. 30) Tursi A, Brandimarte G, Giorgetti GM. Endoscopic and histological findings in the duodenum of adults with celiac disease before and after changing to a gluten-free diet: a 2-year prospective study. Endoscopy 2006; 38: in press.
-
- celiac disease
- diagnosing celiac disease
- (and 5 more)
-
New here! In short, I’m a 22yo female with chronic nausea/vomiting, loss of appetite, painful diarrhea, 90+ pound weightloss in a bit over a year, tingly hands/feet, awful fatigue, and stomach pains with a history of anxiety/depression dating back to childhood, but absolutly no other previous conditions. I think there’s a possibility I have celiac, but my doctors don’t seem to be too helpful communicating with me the meaning of the tests results. They pretty much just said “hmmmm...it could be, but maybe not” which to me is a lame answer. I was hoping someone could take a look at these results and interprete if it sounds like it could be Celiac or not. igA- 595 mg/dL *went up from 555 three weeks ago if that means anything, they accidentally ordered the same test twice Ttg- 1 U/mL HLA DQ2- positive HLA DQ8- negative Endoscopy/colonoscopy biopsies- Duodenal mucosa with patchy mildly increased intraepithealial lymphocytes, preserved villous architecture Gastric oxyntic mucosa with focal mild chronic inflammation focal active colitis in right colon *I don’t know if this is relavent, but my bilirubin is slightly elevated I’m still waiting on results from deamidated gliadin peptic antibodies igA igG. I was also wondering if anyone here is a cigarette smoker and if that delayed diagnosis, I read that somewhere, and I do smoke maybe a pack and a half a week as I have been for the last 5 years (symptoms started a year and a half ago). What do yas think? Should I cut out the gluten? Right now, while I don’t eat a lot, when I do it’s definilty not gluten free.
- 4 replies
-
- biopsy
- colonoscopy
-
(and 1 more)
Tagged with:
-
This is my second thread within a few days, sorry it is long! My biopsy results came today, exactly 6 weeks after the endoscopy. They were "reported as normal." And I am honestly devastated. I've been crying all day. I needed those samples to come back positive, because I cannot - no, I will not - go on like this anymore. Some background: I had panic attacks in 2011 that eventually had me hospitalised with a heart rate of 170. After leaving the hospital I noticed I had constant indigestion and light headedness, symptoms that they assured me were due to the heart rate. When things calmed down, they said it was the beta blockers. After coming off the beta blockers, I started questioning my doctors why I had indigestion, acid reflux; why I was now light headed in the cinema, squinting and holding my head from the loud noise; why I was now sensitive to the sun, to light, to heat; and why I had symptoms of IBS. To cut a long story short, I've been getting treatment for IBS and especially the reflux since 2012, with absolutely no success. I've had every test and I now have a hiatal hernia and acid/bile in the esophagus constantly. I've also had muscle pain and severe weakness, and joint pain. After writing my doctor a letter last May, he suggested testing for celiac, as all my symptoms fit and my father had actually been found celiac positive in his last blood test, but my dad had no idea about that until very recently. I've had three blood tests - all negative. I've had a biopsy - negative. And I've been eating copious amount of bread and wheat for many months, and have never felt worse. The doctors tell me that the reflux will just stop on its own one day. I don't think that ever happens. I mentioned that my father had been diagnosed with M.E/Chronic fatigue syndrome in 2000, and that for a long time we've wondered if I might have inherited it. They didn't really say anything to that. I know it's not good to have celiac disease, but it has treatment, and it has hope. There are worse things to be diagnosed with, crohns, even M.E. There is no treatment for those. I don't want to have fundoplication surgery for the reflux and hernia, because it sounds awful and scary. The gastroenterologist didn't even think the surgery was necessary when I last spoke to her. But I really cannot go on with it, I refuse, so without a diagnosis of celiac, what's left for me to do? Just fundoplication. I was prepared to replace my food, was planning it. I've been researching for months. I even managed to delude myself into believing I have celiac. When my dad got a letter a couple of weeks ago about his last blood test being "strongly suggestive of coeliac disease," I hoped even harder. I thought it was a sign! I feel so foolish. Now I'll have to wait to see the gastroenterologist again to talk about... What? Fundoplication? She didn't even want to do it. She just shrugged and smiled and said I was a difficult patient. I'm going to see my dad's doctor this week, if I can, to talk about how likely it is that I might have celiac after all, regardless of my results, because of my dad's positive blood test, and to discuss the possibility I might have M.E/Chronic fatigue syndrome. In all honesty, I was prepared to look into M.E, until my dad's letter. Then I was even more certain my problem was gluten. Now they tell me, I have no problem with gluten. I feel SO ill right now, I can only describe it as "malaise." My head is light yet heavy, with pressure. My eyes are begging to close. My gut has been painful for over a week. I can feel acid reflux as always. My nails are cracked and peeling, as always. There is blood in my stools. My muscles are painful and so weak that I couldn't stretch out my arm while holding a mug without my arm feeling weak and wobbly. My legs were wobbling as I walked on Saturday. My gums feel as if there could be an ulcer. And I have acne, pale/yellow skin tone, and a headache is threatening. I just can't go on. Really thinking about giving up. I will try to go gluten free anyway, but my mum doesn't believe gluten is my problem and has been sceptical the whole time, so she is reluctant to learn about cross contamination in the kitchen. She just says it's not the problem and it's something else. I don't want to have NCGS because I don't think my doctors/gastroenterologists believe it exists. Thank you for any help :(.
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8-M):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8-M):