-
Welcome to Celiac.com!
You have found your celiac tribe! Join us and ask questions in our forum, share your story, and connect with others.
-
Celiac.com Sponsor (A1):
Celiac.com Sponsor (A1-M):
-
Get Celiac.com Updates:Support Celiac.com!
Search the Community
Showing results for tags 'sensitivity'.
-
Celiac.com 03/04/2004 - Gluten sensitivity is the process by which the immune system reacts to gluten contained in wheat, barley, rye, and oats. The reaction begins in the intestine because that is where the inciting antigen, gluten, is present (from food). When this immunologic reaction damages the finger-like surface projections, the villi, in the small intestine (a process called villous atrophy), it is called celiac disease (or sometimes celiac sprue or gluten-sensitive enteropathy). The clinical focus of gluten-induced disease has always been on the intestine because that is the only way the syndrome was recognized before screening tests were developed. The intestinal syndrome consists mainly of diarrhea, gas, bloating, nausea, vomiting, fat in the stool, nutrient malabsorption, and even constipation. Although the small intestine is always the portal of the immune response to dietary gluten, it is not always affected in a way that results in villous atrophy. Even though recent research has shown that celiac disease is much more common than previously suspected, affecting 1 in 100-200 Americans and Europeans, past and emerging evidence indicates that it accounts for only a small portion of the broader gluten sensitive clinical spectrum (often referred to as the "Tip of the Gluten Sensitive Iceberg"). With better understanding of how gluten triggers immune and autoimmune reactions in the body under the control of various genes, and advancing techniques of detecting these reactions, it is becoming apparent that the majority of the gluten sensitive population (the submerged "mass of the iceberg") do not manifest villous atrophy in its classic, complete form and therefore do not have celiac disease. In these non-celiac, gluten sensitive individuals, the brunt of the immune reaction either affects the function of the intestine, causing symptoms without structural damage, affects other tissues of the body (and virtually all tissues have been affected in different individuals), or both. This is important because the commonly used diagnostic tests of clinically important gluten sensitivity (blood tests for certain antibodies and intestinal biopsies) are only positive when villous atrophy of the small intestine is present. But if only a small minority of gluten sensitive individuals actually develop celiac disease, the majority, who have not yet or may never develop villous atrophy, with or without symptoms, can remain undiagnosed and untreated for years. This can result in significant immune and nutritional consequences, many of which are irreversible even after treatment with a gluten-free diet. Some of these disorders include loss of hormone secretion by glands (hypothyroidism, diabetes, pancreatic insufficiency, etc), osteoporosis, short stature, cognitive impairment, and other inflammatory bowel, liver, and skin diseases, among others. Only with early diagnosis, can these problems be prevented or reversed. I am here to report on a scientific paradigm shift regarding early diagnosis of gluten sensitivity based on about 30 years of medical research by myself and others. My message is that earlier and more inclusive diagnosis of gluten sensitivity than has been allowed by blood tests and intestinal biopsies must be developed to prevent the nutritional and immune consequences of long-standing gluten sensitivity. Imagine going to a cardiologist because your blood pressure is high or you're having chest pain, and the doctor says he is going to do a biopsy of your heart to see what is wrong. If it "looks" O.K., you are told you have no problem and no treatment is prescribed because you have not yet had a heart attack showing on the biopsy. You would not think very highly of the doctor utilizing this approach because, after all, isn't it damage to the heart that you would want to prevent? But for the intestine and gluten sensitivity, current practice embraces this fallacious idea that until an intestinal biopsy shows structural damage, no diagnosis or therapeutic intervention is offered. This has to change now because with newly developed diagnostic tests, we can diagnose the problem before the end stage tissue damage has occurred, that is "before the villi are gone," with the idea of preventing all the nutritional and immune consequences that go with it. There are many misconceptions regarding the clinical presentation of gluten sensitivity or celiac disease: For example, that you cannot be gluten sensitive if you have not lost weight, are obese, have no intestinal symptoms, or are an adult or elderly. However, the most widely held and clinically troublesome misconception is that a negative screening blood test, or one only showing antigliadin antibodies (without the autoimmune antiendomysial or anti-tissue transglutaminase antibody) rules out any problem caused by gluten at that time or permanently. For some reason, the high "specificity" of these blood tests has been tightly embraced. Specificity means if the test is positive, you surely have the disease being tested for with little chance that the positive is a "false positive." But sadly, a negative test does not mean you do not have the problem. This is the biggest pitfall of all because the only thing a very specific test, like blood testing for celiac disease, can do is "rule in" the disease; it can not "rule it out." If you've got very far advanced and/or long-standing celiac disease, it is likely that the test will be positive. However, several studies have now revealed that it is only those with significant villous atrophy of the small intestine who regularly show a positive antiendomysial or anti-tissue transglutaminase antibody, the specific tests relied upon most heavily for diagnosis of gluten-induced disease. When there was only partial villous atrophy, only 30% had a positive test. More disturbing perhaps, were the results with respect to screening first degree relatives of celiacs with blood tests. Despite some biopsy-proven early inflammatory changes in the small intestine but without villi damage, all blood tests were negative. For some reason, it's been perfectly acceptable to celiac diagnosticians that a patient must have far advanced intestinal gluten sensitivity, i.e., villous atrophy, to be diagnosed and a candidate for treatment with a gluten-free diet. That means from the specific testing standpoint, there's never (or rarely) a false positive. But what about the larger majority of gluten-affected people who do not presently have or may never get this end stage, villous atrophic presentation? They are out of luck as far as blood testing is concerned. So the fact is that we have erroneously relied on specificity (always picks up gluten sensitivity after it has caused villous atrophy, never having a false positive) instead of sensitivity (doesn't miss gluten sensitive people even though they might be picked up early, even before full-blown celiac disease develops). Would a test relying on specificity rather than sensitivity be good enough for you, or your children? Consider the risk of not getting an early diagnosis versus going on a gluten free diet a few months or years prematurely. While I do not recommend anyone to have a biopsy (especially children) for diagnosis because of the shortcomings and invasive nature of this technique, I particularly do not want someone to have a biopsy showing villous atrophy, since by that time, associated bone, brain, growth, and/or gland problems are all but guaranteed. And here is another related problem: You have a positive blood test, but, if a small bowel biopsy comes back normal or nearly normal, you are told that the blood test must have been a "false positive" and that gluten is not your problem. Would you believe that, especially in light of the fact that most such people would have gotten the blood test in the first place because of a specific symptom or problem? Let's hope not. All that means (positive blood test, negative biopsy) is that the gluten sensitivity (evidenced by antibodies to gliadin in the blood) has not yet damaged your intestines severely. Evidence of this comes from a study that I performed. We tested 227 normal volunteers with blood tests for celiac disease. Twenty-five of these people (11%) had either antigliadin IgG or IgA in their blood versus only one (0.4%) that had antiendomysial, anti-tissue transglutaminase, and antigliadin IgA in the blood. So for every one person in a population that has the antibodies that have 100% specificity for celiac disease of the intestine (antiendomysial and anti-tissue transglutaminase), there are 24 that have antibodies to gliadin that may not have celiac disease. So what is going on with the 11% with antigliadin antibodies in blood? Are these false positives (rhetorically)? You're telling me that there is a disease called celiac disease and it is associated with antibodies to gliadin in the blood and sometimes it damages the intestine? But people with antigliadin antibody in their blood but no other antibodies do not have a clinically significant immunologic reaction to gluten? Do you see the problem? How can 11% be false positives? What about the 89% with none of these antibodies? You cannot equate having no antibodies at all (a negative test) with having antigliadin antibodies alone. If you have antibodies to gliadin, something is going on here. Where there's smoke there's fire. The purpose of this study was to test this hypothesis: That an antigliadin antibody alone does indicate the presence of an immune reaction to gluten that may be clinically important. Using tests for intestinal malabsorption and abnormal permeability (i.e., tests of small bowel function, unlike a biopsy which says nothing about function), we found that 45% of people with only an antigliadin IgG or IgA antibody in blood (without either antiendomysial or anti-tissue transglutaminase antibody) already had measurable intestinal dysfunction, compared to only 5% of people with no antibodies to gliadin in their blood. When we did biopsies of these people's intestines, none had villous atrophy with only a few showing some early inflammation. Thus, having an antigliadin antibody in your blood does mean something: That there is nearly a 1 in 2 chance that functional intestinal damage is already present even though it may not be visible structurally at the resolution attained by a light microscope assessment of a biopsy. As mentioned at the outset, not all gluten sensitive individuals develop villous atrophy. Evidence for this has been around for a long time. In 1980, a medical publication titled "Gluten-Sensitive Diarrhea" reported that eight people with chronic diarrhea, sometimes for as long as 20 years, that resolved completely when treated with a gluten-free diet, had mild small bowel inflammation but no villous atrophy. In 1996 in a paper called "Gluten Sensitivity with Mild Enteropathy," ten patients, who were thought to have celiac disease because of a positive antiendomysial antibody blood test, had small bowel biopsies showing no villous atrophy. But amazingly, these biopsies were shown to react to gluten when put in a Petri dish, proving the tissue immunologically reacted to gluten (which was likely anyway from their positive blood tests). Two other reports from Europe published in 2001 showed gluten sensitivity without villous atrophy (and hence without celiac disease). In one of these studies, 30% of patients with abdominal symptoms suggestive of irritable bowel syndrome having the celiac-like HLA-DQ2 gene but no antibodies to gliadin in their blood, had these antibodies detected in intestinal fluid (obtained by placing a tube down into the small intestine). Thus, in these people with intestinal symptoms, but normal blood tests and biopsies, the antigliadin antibodies were only inside the intestine (where they belong if you consider that the immune stimulating gluten also is inside the intestine), not in the blood. This is the theme we have followed in my research, as we are about to see. More proof that patients in these studies were gluten sensitive came from the fact that they all got better on a gluten-free diet, and developed recurrent symptoms when "challenged" with gluten. Although the gluten-sensitive patients in these studies did not have the villous atrophy that would yield a diagnosis of celiac disease, small bowel biopsies in many of them showed some, albeit minimal, inflammatory abnormalities. Yet, when a symptomatic patient in clinical practice is biopsied and found to have only minimal abnormalities on small bowel biopsy, clinicians do not put any stock in the possibility of their having gluten sensitivity. As much as I would like to take credit for the concept, you can see from these studies that I did not invent the idea that not all gluten sensitive patients have villous atrophy. It has been around for at least 23 years, and reported from different parts of the world. For many years there has also been proof that the intestine is not the only tissue targeted by the immune reaction to gluten. The prime example of this a disease called dermatitis herpetiformis where the gluten sensitivity manifests primarily in skin, with only mild or no intestinal involvement. Now from more recent research it seems that the almost endless number of autoimmune diseases of various tissues of the body also may have the immune response to dietary gluten and its consequent autoimmune reaction to tissue transglutaminase as the main immunologic cause. A study from Italy showed that the longer gluten sensitive people eat gluten, the more likely they are to develop autoimmune diseases. They found that in childhood celiacs, the prevalence of autoimmune disease rose from a baseline of 5% at age two to almost 35% by age 20. This is a big deal if you think of how much more complicated one's life is when one is both gluten sensitive AND has an additional autoimmune disease. So preventing autoimmune disease is one very important reason why early diagnosis and treatment of gluten sensitivity is important. Early diagnosis before celiac disease develops also holds the potential of preventing other clinical problems such as malnutrition, osteoporosis, infertility, neurologic and psychiatric disorders, neurotube defects (like spina bifida) in your children, and various forms of gastrointestinal cancer. Another reason for early diagnosis and treatment is very straightforward and that is because many gluten sensitive individuals, even if they have not yet developed celiac disease (villous atrophy), have symptoms that abate when gluten is removed from their diet. Furthermore, from a study done in Finland, a gluten sensitive individual who reports no symptoms at the time of diagnosis can improve both psychological and physical well-being after treatment for one year with a gluten-free diet. Despite the common sense and research evidence that early diagnosis of gluten sensitivity offers many health advantages over a diagnostic scheme that can only detect the minority and end-stage patients, until now, the limitation was still in the tests being employed. As mentioned above, the main tests used for primary (before symptoms develop) and secondary (after symptoms develop) screening for celiac disease, blood tests for antigliadin and antiendomysial/anti-tissue transglutaminase antibodies, are only routinely positive after extensive damage to intestinal villi. As shown in a 1990 publication, this is because unless you have full blown, untreated celiac disease, the IgA antibodies to gliadin are only INSIDE the intestine not in the blood. Measuring antigliadin antibody in blood and intestinal fluid (obtained by the laborious technique of having research subjects swallow a long tube that migrates into the upper small intestine), researchers found that in untreated celiacs, antigliadin antibody was present in the blood and inside the intestine, whereas after villous atrophy healed following a year on a gluten-free diet, the antigliadin antibody was no longer in the blood but was still measurable inside the intestine in those with ongoing mild inflammation. An important conclusion can be drawn from these results, as these researchers and myself have done: Gluten sensitive individuals who do not have villous atrophy (the mass of the iceberg), will only have evidence of their immunologic reaction to gluten by a test that assesses for antigliadin IgA antibodies where that foodstuff is located, inside the intestinal tract, not the blood. This makes sense anyway, because the immune system of the intestine, when fighting an antigen or infection inside the intestine, wages the fight right in that location in an attempt to neutralize the invading antigen, thereby preventing its penetration into the body. It does this with T cells on the surface of the epithelium, the intraepithelial lymphocytes, and with secretory IgA made with a special component called secretory piece that allows its secretion into the intestine. The excellent English researchers that made the discovery that they could detect the immunologic reaction to gluten inside the intestine before it was evident on blood tests or biopsies knew it was a breakthrough, testing it many times over in different ways, and further extending the clinical spectrum of gluten-induced disease to include a phase before the villi are damaged, so-called "latent celiac sprue". Furthermore, they developed this technique of assessing the intestinal contents for antigliadin antibodies into what they viewed as a "noninvasive screening test for early or latent celiac sprue" (what others and I would simply call "gluten sensitivity"). However, this was not exactly noninvasive, nor was it simple. It still required the patient to swallow a tube, followed by a complete lavage of all their gastrointestinal contents with many gallons of nonabsorbable fluid that had to be passed by rectum and collected into a large vat to be analyzed for the presence of antigliadin antibodies. While this was indeed a conceptual breakthrough, it practically went unnoticed by the medical community because the cumbersome procedure of washing out the intestine just could not be done in a normal clinical setting. To this day, I am not sure how many people even know that it was not me, but rather this well known celiac research group, led by the late Dr. Anne Ferguson, who pioneered the assessment of the intestinal contents as a viable and more sensitive source of testing material for the early reactions of the immune system to gluten. What we did in my research was to refine and simplify the method of collecting and measuring these intestinal IgA antigliadin antibodies before they can be detected in blood. That is, instead of washing out the antibodies from the intestine, we allow them to be excreted naturally in the stool (feces). And so with that idea, and our ability to measure these antibodies in stool, as others before us had done for fecal IgE antibodies directed to food antigens, our new gluten (and other food) sensitivity stool testing method was born. It was actually my research of microscopic colitis that led me to discover that stool analysis was the best way of assessing for gluten sensitivity before celiac disease develops. Microscopic colitis is a very common chronic diarrheal syndrome, accounting for 10% of all causes of chronic diarrhea in all patients, and is the most common cause of ongoing chronic diarrhea in a treated celiac, affecting 4% of all celiac patients. However, from my published research, despite the presence of the celiac HLA-DQ2 gene in 64% of patients with microscopic colitis, very few get positive blood tests or biopsies consistent with celiac disease. Yet, small bowel biopsies revealed some degree of inflammation sometimes with mild villous blunting in 70% of cases. According to the facts and previously discussed shortcomings of celiac blood tests, antibodies to gliadin are unlikely to be detected in the blood in these patients because they lack villous atrophy. So negative blood tests for antigliadin antibodies per se did not, in my mind, rule out the possibility that these patients with microscopic colitis, a disease that under the microscope looks like celiac disease (but of the colon), and that affects many celiac patients, were not gluten sensitive themselves. But as Dr. Ferguson's research revealed, these antibodies might be detectable inside the intestine. And since we surely were not going to perform that cumbersome intestinal lavage test in my patients, we decided to see if we could find these antibodies in the stool as a reflection of what is coming through the intestine. Here's the first set of data that we found showing the superior sensitivity of stool testing versus blood tests for antigliadin IgA antibodies. In untreated celiac disease patients, we found a 100% positivity in the stool versus only 76% in blood. In hundreds of microscopic colitis patients since tested, only 9% have antigliadin antibody in blood but 76% have it in stool. And the same is true of 79% of family members of patients with celiac disease; 77% of patients with any autoimmune disease; 57% of people with irritable bowel syndrome-like abdominal symptoms; and 50% of people with chronic diarrhea of unknown origin, all of whom have only about a 10-12% positivity rate for blood tests (like normal volunteers). Thus, when you go to the source of production of these antibodies for testing, the intestine, the percentage of any population at a higher than normal genetic and/or clinical risk of gluten sensitivity showing a positive antigliadin stool test is 5 to 7.5 times higher than would be detected using blood tests. In normal people without specific symptoms or syndromes, the stool test is just under 3 times more likely to be positive than blood (29% vs. 11%, respectively). That's a lot more people reacting to gluten than 1 in 150 who have celiac disease. 29% of the normal population of this country, almost all of whom eat gluten, showing an intestinal immunologic reaction to the most immune-stimulating of dietary proteins really is not so high or far fetched a percentage, especially in light of the fact that 11% of them display this reaction in blood, and 42% carry the HLA-DQ2 or DQ8 celiac genes. Why is this so important? Because some people with microscopic colitis never get better when they're treated, and most autoimmune syndromes only progress with time, requiring harsh and sometimes dangerous immunosuppressive drugs just for disease control. If the immune reaction to gluten is in any way at the cause of these diseases as research suggests, and if we had at our disposal a sensitive test that can diagnose this gluten sensitivity without having to wait for the intestinal villi to be damaged, then treatment with a gluten free diet might allow the affected tissues to return to normal or at least prevent progression. We now have that test in fecal antigliadin antibody. Just a few weeks ago we completed the first follow-up phase of our study: What happens when a gluten sensitive person without villous atrophy goes on a gluten-free diet for one or two years. While I am still gathering and analyzing the data, most of the subjects reported a much improved clinical status (utilizing an objective measure of symptoms and well being). Not everybody gets well, because sadly not everyone stays on a gluten-free diet (as they sometimes admit on the surveys). Some people have the misconception that if they don't have celiac disease, but "I just have gluten sensitivity" then maybe they do not have to be strict with their gluten elimination diet. I do not think that is the case. Although a gluten free diet is like anything: Less gluten is not as damaging as more gluten, but certainly no gluten is optimal if a gluten sensitive person desires optimal health. Of the first 25 people with refractory or relapsing microscopic colitis treated with a gluten-free diet, 19 resolved diarrhea completely, and another five were notably improved. Thus, a gluten-free diet helped these patients with a chronic immune disease of a tissue other than small bowel (in this case the colon), who have been shown to be gluten sensitive by a positive stool test in my lab. The same may be true of patients with chronic autoimmune diseases of any other tissue, but who do not have full-blown celiac disease. Gluten-free dietary treatment, sometimes combined with dairy-free diet as well, has been shown to help diabetes, psoriasis, inflammatory bowel disease, eczema, autism, and others. Thus, my approach (and I believe the most sensitive and most complete approach) for screening for early diagnosis and preventive diagnosis for clinically important gluten sensitivity is a stool test for antigliadin and anti-tissue transglutaminase IgA antibodies (IgG is not detectable in the intestine) and a malabsorption test. The malabsorption test we developed is special, because you no longer have to collect your stool for three days; we can find the same information with just one stool specimen. Stool testing in combination with HLA gene testing, which we do with a cotton-tipped swab rubbed inside the mouth, is the best diagnostic approach available for gluten sensitivity. Who should be screened for gluten sensitivity? Certainly family members of celiacs or gluten sensitive people being at the highest genetic risk. For the most part, all of the following patient groups have been shown to be at higher risk than normal for gluten sensitivity: Chronic diarrhea; microscopic colitis; dermatitis herpetiformis; diabetes mellitus; any autoimmune syndrome (of which there is an almost end-less number like rheumatoid arthritis, multiple sclerosis, lupus, dermatomyositis, psoriasis, thyroiditis, alopecia areata, hepatitis, etc.); Hepatitis C; asthma; chronic liver disease; osteoporosis; iron deficiency anemia; short stature in children; Down's syndrome; female infertility; peripheral neuropathy, seizures, and other neurologic syndromes; depression and other psychiatric syndromes; irritable bowel syndrome; Crohn's Disease; and people with severe gastroesophageal reflux (GERD). Autism and possibly the attention deficit disorders are emerging as syndromes that may improve with a gluten- free (and additionally casein-free) diet. A diagnosed celiac might be interested in our testing to know (after some treatment period no shorter than a year) that there is no on-going damage from malabsorption, for which we have a test. If a celiac is having ongoing symptoms or other problems, a follow-up test should be done just to be sure there's no hidden gluten in the diet, or something else that could be present, like pancreatic enzyme deficiency which often accompanies celiac disease, especially in its early stages of treatment. Historically, with respect to diagnostic methods for celiac disease, from 100 A.D., when celiac disease was first described as an emaciating, incapacitating, intestinal symptom-causing syndrome, to 1950, we had just one diagnostic test: Clinical observation for development of the end stage of the disease. Then in 1940 to 1960, when the discovery of gluten as the cause of celiac disease occurred, the best diagnostic test was removing gluten from the diet and watching for clinical improvement. It was during this period that the 72-hour fecal fat and D-xylose absorption tests were developed as measures of gluten-induced intestinal dysfunction/damage. In the mid- to late1950's, various intestinal biopsy methods were pioneered and utilized, showing total villous atrophy as the diagnostic hallmark of celiac disease. You've heard the intestinal biopsy called the "gold standard"; well as you can see, it is a 50 year-old test, and thus, the "old" standard. It was not until the 1970's and 80's (and improved upon in the 1990's) that blood tests for antigliadin and antiendomysial/anti-tissue transglutaminase were developed, but again these tests like all methods before, can reliably reveal only the "heart attack" equivalent of the intestinal celiac syndrome: Significant villous atrophy or bad celiac disease. We are in a new century, a new millennium, and I have built upon what my research predecessors have started; mostly on the work of researchers who laboriously put down tubes and sucked out intestinal fluid for testing for antigliadin antibody when it was not present in blood. We now know that a stool test for antigliadin antibody is just as good and much simpler. The wide-reaching ramifications of knowing that so many more people and patients are gluten sensitive than have ever been previously known has led me to assume a professional life of medical public service. To do so, I started a 501©3 not-for-profit institute called the Intestinal Health Institute, have brought these new diagnostic tests to the public on the internet (at http://www.enterolab.com), and volunteer my time helping people with health problems by email and by lecturing. With greater awareness and education of both the public and medical community that early diagnosis of gluten sensitivity can be achieved before the villi are gone, more of the gluten sensitive iceberg will be diagnosed and treated early, leading to far fewer gluten-related symptoms and diseases than has ever been experienced before. Dr. Fine has been an intestinal researcher and an academic and clinical gastroenterologist for 15 years. He is the Director of The Intestinal Health Institute and The www.EnteroLab.com Clinical Laboratory in Dallas Texas.
- 38 comments
-
Celiac.com 04/10/2005 - Celiac disease is, by definition, a condition in which the intestinal wall is damaged as a result of eating gluten. It is a chronic illness in which the symptoms wax and wane1 for reasons that are not yet understood. Celiac disease is the result of genetic and environmental factors. We now know two HLA markers (DQ2 and DQ8) for the predisposition for celiac disease2. One environmental factor is, of course, the consumption of gluten, but there may be other environmental contributors. Recent research reveals that about 1% of the population suffers from this condition3 although most remain undiagnosed. On the other hand, gluten sensitivity is characterized by antigliadin antibodies. This condition afflicts at least 12% of the general population4 and is found in patients with a wide variety of autoimmune diseases. In some studies of neurological diseases of unknown origin, a majority of patients show signs of gluten sensitivity4. These patients are mounting an immune response to the most common food in the western diet, yet many practitioners consider gluten sensitivity to be a non-specific finding, frequently counseling patients to ignore these test results. This is particularly unfortunate since a strict gluten-free diet has repeatedly proven helpful to patients who are fortunate enough to consult a practitioner who is versed in gluten sensitivity and its connection with autoimmunity. Untreated celiac disease carries an added risk for a wide variety of additional autoimmune diseases. The most likely cause of this predisposition to additional autoimmune disease is a condition sometimes referred to as leaky gut syndrome. We know that gluten causes intestinal damage. We also know that this damage allows large undigested and partly digested proteins to leak into the bloodstream through the damaged intestinal wall. This leakage results in immune system production of antibodies to attack these foreign proteins as if they were invading microbes. The result is the production of a huge variety of selective antibodies, and each type recognizes a particular short chain of amino acids located somewhere in the proteins structure. Unfortunately, our own tissues can contain very similar or identical sequences of amino acids. Hence, by a process called molecular mimicry, we are producing antibodies that attack both the foreign food proteins that are leaked into our blood through the damaged intestinal wall, and similar amino acid sequences in our own tissues, often resulting in an autoimmune disease5. The supposedly non-specific antigliadin antibodies in gluten sensitivity provide two important pieces of information: 1) That the intestinal wall has been damaged and is permitting leakage of food proteins into the bloodstream, and; 2) That the dynamic contributing to increased autoimmunity in celiac disease may well be an important contributing factor in gluten sensitivity5. The currently common view that celiac disease is a serious illness, while disregarding gluten sensitivity, is dangerous to gluten sensitive patients. This bias is also a divisive element in the gluten-sensitive/celiac community. Whether a person has "biopsy proven" damage to the intestinal wall, if this person gets sick from eating gluten, or mounts an immune response to gluten, we are all in the same leaky boat (please pardon the pun). We need to work together to get a better understanding of gluten sensitivity in all its forms (including celiac disease). As a community, we need to discourage any kind of dismissal of illnesses that are partly or wholly mediated by gluten. If we can stand together in our quest for widespread recognition of the damaging impact of gluten consumption, we can all enjoy a healthier life. Our descendants will also inherit a more gluten-savvy world. Sources: Cooke W, Holmes G. Coeliac Disease. Churchill Livingstone, New York, N.Y. 1984. Fasano A. Celiac disease--how to handle a clinical chameleon. N Engl J Med. 2003 Jun 19;348(25):2568-70. Fasano A, Berti I, Gerarduzzi T, Not T, Colletti RB, Drago S, Elitsur Y, Green PH, Guandalini S, Hill ID, Pietzak M, Ventura A, Thorpe M, Kryszak D, Fornaroli F, Wasserman SS, Murray JA, Horvath K. Prevalence of celiac disease in at-risk and not-at-risk groups in the United States: a large multicenter study. Arch Intern Med. 2003 Feb 10;163(3):286-92. Hadjivassiliou M, Grunewald RA, Davies-Jones GA. Gluten sensitivity as a neurological illness. J Neurol Neurosurg Psychiatry. 2002 May;72(5):560-3. Braly J, Hoggan R.. Dangerous Grains, Penguin-Putnam-Avery, New York, N.Y., 2002.
- 8 comments
-
- celiac
- difference
-
(and 3 more)
Tagged with:
-
Celiac.com 05/04/2021 - Immunoglobulin A tissue transglutaminase gives doctors a noninvasive way to spot celiac disease, but new research suggests that its sensitivity may be lower than estimated, making it a poor screening test, at least in asymptomatic patients. The reason comes down to verification bias, wherein a technique appears to have higher sensitivity and lower specificity than it actually does, because individuals who screen positive are more likely to have their disease confirmed by a follow-up small-bowel biopsy, while those who screen negative are unlikely to have a follow-up biopsy that could reveal missed celiac disease. That matters because the disparity could lead to missed celiac diagnoses, because some of those in the negative group could actually have celiac disease. "What you're missing from when you're calculating sensitivity is, what about the ones that are negative on the index test? Would they have been positive on that reference test? That's not even coming into your calculation because they're not getting that reference test," said Marisa Stahl, MD, a physician and researcher at the Children's Hospital Colorado Center of Celiac Disease in Aurora. Stahl was not involved in the meta-analysis, but commented on it in an interview. To determine whether the studies used by USPSTF may have overestimated sensitivity due to verification bias, Isabel Hujoel, MD, of the Mayo Clinic, Rochester, Minn., and colleagues conducted a meta-analysis, in which they reviewed those same nine studies to see the potential impact of verification bias. They then rated each study as being high, low, or unclear for possible verification bias. In all, they found five studies to be high risk. The only way to fully correct the bias is to run both IgA tissue transglutaminase (tTG) testing and small bowel biopsy on a complete or random sample of patients, and compare the sensitivity and specificity of IgA tTG with the preferred method small-bowel biopsy. But this is almost never done. Instead, when the U.S. Preventive Services Task Force concluded that evidence was insufficient for IgA tTG testing for celiac disease, it relied on a 2016 comparative effectiveness review of nine studies that estimated sensitivity at 92.6% and specificity at 97.6%. USPSTF remained noncommittal because of inadequate evidence surrounding the balance of benefit and harms of screening for celiac disease in asymptomatic individuals. Dr. Stahl was a bit shocked to see that the sensitivity was so much lower than has been traditionally accepted. The data clearly shows that "...the sensitivity is probably lower than what we oftentimes reference, and we should think more about the population of patients that could potentially screen negative and still have celiac disease," she said. Stahl suggests that the problem may be more common in adults, who have a higher incidence of seronegative Celiac disease, though there is no good data on that point, right now. Clearly reduced sensitivity of IgA tissue transglutaminase (tTG) testing is a big deal, and we're likely to hear more on this, so stay tuned. Read the full report in the Journal of Clinical Gastroenterology and the abstract pubmed.ncbi.nlm.nih.gov
- 4 comments
-
- blood test
- celiac disease
- (and 6 more)
-
To All, This for those who have a Sulfite allergy specifically. But I also creating this as a reference article for Molybdenum......and how It is important for us to "Detox" our body. Without it Oxidative Stress builds up in the body leading to inflammation and disease. Here are the references for anyone who has Sulfite Allergy or SIBO or a Candida (Yeast) Problem. https://www.thecandidadiet.com/molybdenum/ https://www.raggeduniversity.co.uk/2019/08/11/prospecting-document-molybdenum-adjunct-to-thiamine-therapy-in-relation-to-alcohol-use/ https://www.eonutrition.co.uk/post/got-sibo-here-s-why-you-need-to-get-your-thiamine-status-checked (And your Molybdenum levels checked) https://www.sciencedirect.com/topics/medicine-and-dentistry/molybdenum-deficiency Here is research on Molybdenum's possible role in Type 2 Diabetes... Entitled "Trace elements status in diabetes mellitus type 2: Possible role of the interaction between molybdenum and copper in the progress of typical complications" https://www.diabetesresearchclinicalpractice.com/article/S0168-8227(10)00604-2/fulltext Another on Molybdenum deficiency in wildlife leading to Diabetes like syndrome... Entitled "A syndrome of molybdenosis, copper deficiency, and type 2 diabetes in the moose population of south-west Sweden" https://pubmed.ncbi.nlm.nih.gov/10813452/ And because the Molybdenum/Copper ratio is important in Type 2 diabetes I am also including this article on Copper deficiency in Diabetes... Entitled "Effect of copper or insulin in diabetic copper-deficient rats" https://pubmed.ncbi.nlm.nih.gov/6344092/ I know I have had these deficiencies and after supplementing with them my health got better. See this Posterboy blog post about these Micronutrient deficiencies in Celiac's.... Every time I found I had a Vitamin deficiency.......the doctor's said it was RARE and I couldn't have one.... And every time I have supplemented with my "Rare" Missing Vitamin Deficiency my health has improved... I have found most Celiac's could be low in as many as 20+ Vitamin/Minerals.... It has been a long and winding road as they say.....but around each curve in the road (or set back in my health) I have found a Vitamin Deficiency going undiagnosed and supplement with it has helped it... See this research entitled "Copper deficiency as a cause of neutropenia in a case of Celiac disease" https://pubmed.ncbi.nlm.nih.gov/27635061/ It wasn't the Celiac disease that was the cause of the Nutropenia...it was the Copper deficiency that occurs in/with a Celiac diagnsois! I will quote the whole abstract because it is short! Abstract "We report a 17 year-old male patient, who presented with chronic diarrhoea, progressive pallor, short stature, anaemia (haemoglobin of 4.9 g/dL) and neutropenia and was diagnosed as coeliac disease. His neutropenia did not respond to 8 months of gluten-free diet, iron, folic acid and vitamin B12 therapy. So we suspected copper deficiency and his serum copper levels were tested, which was low. His neutrophil counts normalised after 2 months of copper supplementation. Hence we concluded that the cause of neutropenia in our case was copper deficiency." I am that "Male Patient" that they don't think could have a Copper deficiency.... My High Iron levels are from my Low Copper Status and probably my Low Molybdenum levels/status too! https://medicalxpress.com/news/2007-07-iron-copper-relationship.html#:~:text=Iron and copper relationship is studied. Hereditary hemochromatosis,body iron levels resulting from any medical condition And because Doctor's are not studying nutrition as a cause....when they see a nutrition problem....they can't understand....or haven't studied...it is pronounced as a "Genetic" Problem instead.... See this Polycythemia Vera thread for more details about why Cooper and Iron are related problems... I hope this is helpful but it is not medical advice. Posterboy,
- 2 replies
-
- candida
- molybdenum
-
(and 6 more)
Tagged with:
-
Hello, I wanted to share my personal experience of what cured my Perioral dermatitis. I hope this will help others find a solution to their Perioral dermatitis problems as well. I know how awful it is and how painful those blistering hives are, so my heart goes out to anyone dealing with it. The steps below are what cleared the devil rash off my face, in addition to cutting gluten completely out of my diet. My PD flared up and got so much worse each time I ate anything with gluten. *Disclaimer*: I am not a medical professional. I'm just a fellow victim of Perioral dermatitis trying to help! I do mention products/brands, but this is not a sponsored post in any way. This is just what has worked for me personally. I tried to make this as detailed as possible, but if anyone has any questions, please feel free to reply to this post or message me. 1). DO NOT PUT ACNE CLEARING PRODUCTS ANYWHERE NEAR IT!!! I had absolutely no clue what Perioral dermatitis even was when it first showed up. I just thought it was acne since it was on my face. I made the massive mistake of putting acne washes that contained alcohols, acne creams, toners, and then finally hydrocortisone all over the bumps. Which caused the rash to viciously spread like wildfire. This is why it is so important to see a dermatologist about your skin problems. 2). Doxycycline. My dermatologist prescribed me doxycycline 100 mg, 1 per day for 6 weeks (Currently still taking it because the 6 weeks aren't up yet.) But after 3 doses, I am not even kidding you, the PD rash/bumps began to disappear. And the inflamed, burning, blistering itch was no more!!! Talk to your dermatologist about the best option for you, but I give doxycycline the most credit for clearing my Perioral dermatitis so fast. The first dose did make me feel nauseous, so I just take it before bed. It also causes increased sun sensitivity, so be mindful of that. 3). Pimecrolimus Cream 1% (Again, must be prescribed. This is not an over the counter medication.) This cream treats dermatitis and eczema. This is NOT a steroid cream. I warn you all... stay FAR, FAR, FAR away from any steroid topical creams!!! Steroids will make the PD incredibly worse. 4). Spectro Jel Cleanser Frangrance Free. I read about this cleanser on a blog for curing Perioral dermatitis. You can buy this cleanser on Amazon. Read the reviews! You will see that almost every person mentions how great it has been for their PD. From my personal experience, this is the only face wash that hasn't felt like I'm rubbing acid onto my skin. It has seriously worked wonders for me! I wash with it twice a day. I don't use any sort of face washing tool, and no toners, scrubs, serums, etc. If you're suffering from PD or have sensitive skin, I highly suggest you do the same. My skin drastically cleared up once I stopped using unnecessary products. I know that doesn't seem glamorous and fun, but neither is the dermatitis... am i right?! --- Here's a link to the cleanser: https://www.amazon.com/Spectro-Cleanser-Fragrance-Free-200ml/dp/B00CUIKYJW/ref=sr_1_1?dchild=1&keywords=spectro&qid=1598559522&sr=8-1 5). Fluoride free toothpaste. My dermatologist told me to throw out my toothpaste if it contained fluoride. She said toothpaste containing fluoride can actually cause or irritate PD. The brand I like and recommend is 'Toms'. It's fluoride free and is made with natural ingredients. 6). Get a gluten free chapstick. I was so surprised to find out how many chapsticks or lip balms actually contain gluten. My lips have always been dry or irritated, regardless of how much water I drink or how much chapstick I use. After discovering my gluten allergy, I realize it's because my lips couldn't handle the ingredients. An amazing, super hydrating option is 'EOS: The Hero Extra Dry Lip Treatment' It is gluten free and hypoallergenic. (but always check labels for ingredients you may be sensitive to) 7). Gluten Free Shampoo and Conditioner. Now obviously, I know (or hope) that no one is ingesting their hair products. However, think about how close they get to your face! Duh it goes all over your scalp, but it also can come in direct contact with your face during a shower. I have been using 'Garnier Fructis Pure Clean' which is free of gluten. I believe it's also free of some other common allergens. Google it and check it out for yourself! 8). All Free Clear Detergent. Oh my gosh... ANYONE with sensitive skin, allergies, eczema, Perioral dermatitis, whatever!!! Please be careful of the detergent you are using to wash your clothes. Detergents have been one of the biggest irritants for my sensitive skin, especially my neck and face. 'All Free Clear' is great and is my go-to. It's the only one that doesn't turn my skin red and make me itch like crazy. 9). Makeup. When my Perioral Dermatitis first happened and was at it's absolute worst, I didn't put any makeup on my face for 2 weeks. Trust me, I know you want to cover it up any way you can. I did too, because I thought I looked like a horrifying monster. But the rash will heal so much faster if you aren't putting foundation or powder on your face. Putting makeup on also means taking it off, and using makeup wipes while I had the rash drove my skin absolutely nuts.
- 1 reply
-
- atopic dermatitis
- dermatitis
- (and 8 more)
-
Celiac.com 03/24/2020 - Many of us have experienced unpleasant symptoms after a meal or snack. The effects might range from mild itching of the mouth, to nausea, or other symptoms, including sneezing, wheezing, skin rash, joint pain, bloating, diarrhea, and more. So is the problem a food allergy, an intolerance, or a sensitivity, and what is the difference? It's not uncommon for people with food sensitivities or intolerances, or even celiac disease, to think they have food allergies. In fact, "food allergy" is a fairly common term that can mean any of these conditions, depending on who is doing the talking. In reality, though, food allergies are more rare and usually more serious than food intolerances or sensitivities. True allergic reactions to foods can range from merely inconvenient to life-threatening. Differences Between Food Allergies, Food Intolerances, and Food Sensitivities Food Intolerances Food intolerance basically means that the body is unable to process or digest certain foods. Food intolerances are very common, and are usually less serious than food sensitivities or food allergies. Lactose intolerance is one of the most common food intolerances. Lactose intolerance happens when people guts don't produce enough of the enzyme lactase to break down the lactose. Lactose intolerance can be inherited, or it can simply happen as some people age and produce less lactase. Research data shows that only about one in three people worldwide can digest lactose past the age of seven or eight. Interestingly, most celiacs with lactose intolerance recover on a gluten-free diet. Once the damaged villi and microvilli to grow back, and the gut heals, the sensitivity to lactose often disappears. This can take time. In most people, full gut healing takes between six months and a year, but it can take up to two years or more. Also, most people who are lactose intolerant can consume goat and sheep cheeses, such as feta or pecorino Romano, without any problems. Some can consume goat or sheep's milk products with no issues. Many people with lactose intolerance can also consume raw, unpasteurized dairy from cows without symptoms. Links to Goat, Sheep, and Raw Cow Milk Products Goat Milk Products Sheep Milk Products Raw Cow Milk Products Lactose intolerance is not a serious medical condition, but symptoms can be quite uncomfortable. Simply avoiding milk and dairy products is the easiest way to avoid symptoms, but over-the-counter lactase enzyme supplements can be helpful for those who wish to consume dairy. Food Sensitivities Food sensitivities are common, and are usually include more serious or debilitating symptoms than food intolerances. Food sensitivities happen when people experience symptoms after eating certain foods. Symptoms are not life-threatening, but can be serious. Symptoms of food sensitivities include joint pain, stomach pain, fatigue, rashes, and brain fog. Gluten is probably the best-known trigger of food sensitivities. When people with celiac disease or certain other medical conditions eat wheat, they provide an immune reaction in the gut that can cause long-term health consequences if left untreated. Researchers currently believe that food sensitivities are the result of an immune reaction that generates a wide rage of symptoms. Food sensitivities can strike at any time, and they can also vanish, sometimes with no apparent explanation. People avoiding certain foods due to sensitivities may want to try small amounts of the food from time to time to see if the situation has changed. Elimination Diet Helps Spot Food Sensitivities The best way to spot food sensitivities is through careful observation and elimination. Removing potential food allergens from the diet for two to four weeks, reintroducing them one at a time, and watching for symptoms is the best way to figure out which food or foods is causing the reaction. Once you've narrowed it down, avoiding the foods that trigger sensitivities can improve both symptoms and quality of life. Food Allergies True food allergies are the body's most serious reaction to food. Food allergies happen when the immune system reacts to certain foods. For example, people with peanut or shellfish allergies can suffer from symptoms including serious difficulty breathing and low blood pressure following exposure to peanuts or seafood. These symptoms can sometimes be fatal. Many people with food allergies carry an epinephrine shot device, such as an Epic-Pen, as a precaution against such episodes. These pens can save lives. Sometimes people have food allergies from very early in life, but they can strike at any time during life, even in old age. If any food causes you to have true allergic reactions, such as significant rashes, dizziness, swelling of the face, or difficulty breathing, it is wise to consider a visit to the doctor for allergy testing and treatment. Celiac Disease Celiac disease is an autoimmune condition that affects about 1% of the Western population. Celiac disease results from a complex inflammatory reaction triggered by gluten consumption in genetically predisposed people. Celiac disease is not a food allergy. Eating gluten a few times does not cause an immediate life-threatening problem. However, when people with celiac disease eat gluten, they often suffer nausea, vomiting, and other symptoms in the short term. Over time, if left untreated, gluten consumption can cause diarrhea, weight loss, and malnutrition, and can lead to many other associated conditions, including certain deadly types of cancer. Avoiding gluten is the only effective treatment for celiac disease. Gluten is found in a variety of grains, including wheat, rye, barley, and in wheat types like kamut, spelt, semolina, bulgur, farro, emmer, einkorn, and farina. Many processed foods also contain gluten in the form of wheat flour. Also, cross-contamination from gluten-containing food is a constant threat, especially when eating out. Conclusion So, food allergies come with strong physical symptoms, such as itching, face swelling, and difficulty breathing. Food allergies can be serious, and even life-threatening, while food intolerances and sensitivities are usually just unpleasant and inconvenient, but some can have long term health consequences. Once you’ve identified the food or foods that trigger your allergy, sensitivity, or intolerance, a nutritionist or a physician can help devise a diet that is safe and nutritious. In the case of allergies, they can also provide you with tools, such as an epinephrine injection, and a plan of attack should a life-threatening reaction occur. Though food intolerances and sensitivities are not unusual, they can be challenging to figure out. Even with an active elimination diet, finding out which foods trigger reactions can be challenging, and time consuming. Ultimately though, tracking down the cause of food intolerances and sensitivities is rewarding, and usually leads to better health and well-being. Resources for Food Allergy, Intolerance, and Sensitivity Mayo Clinic - Food allergy vs. food intolerance: What's the difference? Cleveland Clinic - Allergy or Intolerance: How Can You Tell the Difference? Harvard Medical School - Food allergy, intolerance, or sensitivity: What’s the difference, and why does it matter?
-
Really hoping that someone will be able to help with the situation I’m currently facing. It’s a bit confusing (which seems to be the case with Celiac generally producing lots of strange side effects!) Okay, so I first received a positive celiac blood test via the GP in early 2018 after experiencing a few months of diarrhoea. It was triggered by a stomach virus in work that everyone seemed to get, but mine never quite went away. That’s when I headed to the doctor and got this positive celiac result, completely out of the blue! I have no celiac sufferers or other autoimmune diseases in the family (that we know of), so I couldn’t really understand how this had happened. I then got advice from the doctor to go completely gluten free immediately and she referred me for an endoscopy to confirm diagnosis (no mention of the fact that you need to be eating gluten to get a positive). So surprise surprise I got a negative endoscopy, and the gastro was absolutely certain that I wasn’t celiac for this reason. Despite this, I’d noticed that all of my diarrhoea and gastro symptoms disappeared pretty much immediately after stopping eating gluten. Based on this, I continued to cut gluten out. Also, I understand that a positive blood test alone is pretty much a sure diagnosis of celiac right? Anyway, onto this pesky tingling. A few months after my initial blood test diagnosis I noticed I was getting some very low level tingling in my lower legs. Very low level, easy to miss. I mentioned this to the gastro and he just suggested it could be some nutrient deficiencies still causing issues after the few months of diarrhoea. I stuck to a gluten free diet (with the occasional accidental slip up), hoping that the tingling would go away, but it’s still very much here and I’d say it’s slightly worse. It’s really hard to describe. It’s almost as if my lower legs are buzzing/vibrating. My skin feels really sensitive, so if I brush something against it I get a wave of tingles/shivers. It’s almost that skin sensitivity feeling you get if you have a fever (but I don’t have a fever). Does anyone have this? I was referred to a neurologist to check that there was nothing else going on. They did an MRI and a nerve conduction test, both came back absolutely fine. I also have no weakness/numbness etc. It’s just a sensation. But I don’t know what’s causing it and if it will ever go away. Would love to know if anyone has these sensory issues and how you improved them? I take multivitamins, magnesium and B12 with no change. Could I secretly be ingesting low levels of gluten which continue to cause problems, or could I have other food intolerances which cause systemic inflation. I’ve not yet cut out any food groups. Really hoping someone will be able to shed some light on this.
- 3 replies
-
- neuropathy
- neuropathy pain tingling
-
(and 3 more)
Tagged with:
-
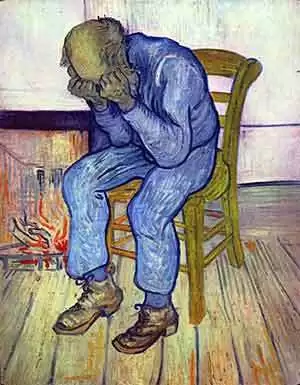
Celiac.com 05/29/2014 - Many people with celiac disease report symptoms of depression, which usually subside upon treatment with a gluten-free diet. But a new study out of Australia suggests that gluten can cause depression in people with non-celiac gluten-sensitivity. Current evidence shows that many patients with self-reported non-celiac gluten sensitivity (NCGS) continue to have gastrointestinal symptoms on a gluten-free diet, but say that avoiding gluten makes them feel ‘better'. So, why do people with non-celiac gluten sensitivity seem to feel better on a gluten-free diet, even if they still have gastrointestinal symptoms? A team of researchers wanted to know if this might be due to gluten’s effects on the mental state of those with NCGS, and not necessarily because of gastrointestinal symptoms. The research team included S. L. Peters, J. R. Biesiekierski, G. W. Yelland, J. G. Muir, and P. R. Gibson. They are affiliated with the Department of Gastroenterology, Central Clinical School of Monash University at The Alfred Hospital in Melbourne, the Department of Gastroenterology at the Eastern Health Clinical School of Monash University in Box Hill, and the School of Health Sciences at RMIT University in Bundoora, Victoria, Australia. For their double-blind cross-over study, they looked at 17 women and five men, aged 24–62 years. All participants suffered from irritable bowel syndrome, but not from celiac disease, and their symptoms were controlled on a gluten-free diet. The team gave the participants one of three random dietary challenges over 3 days, followed by a minimum 3-day washout before moving to the next diet. All participants got all three diets over the course of the study. For each phase, the team supplemented the challenge gluten-free food with gluten, (16 g/day), whey (16 g/day) or nothing at all (placebo). The team assessed mental state as determined by the Spielberger State Trait Personality Inventory (STPI), cortisol secretion and gastrointestinal symptoms. They found that gluten ingestion was associated with higher overall STPI state depression scores compared to placebo [M = 2.03, 95% CI (0.55–3.51), P = 0.010], but not whey [M = 1.48, 95% CI (−0.14 to 3.10), P = 0.07]. They found no differences for other STPI state indices or for any STPI trait measures, and they saw no difference in cortisol secretion between challenges. Gastrointestinal symptoms were similar for each dietary challenge. Short-term exposure to gluten specifically induced current feelings of depression with no effect on other indices or on emotional disposition. Moreover, the team saw no gluten-specific trigger of gastrointestinal symptoms. Such findings might explain why patients with non-coeliac gluten sensitivity feel better on a gluten-free diet despite the continuation of gastrointestinal symptoms. Source: Aliment Pharmacol Ther. 2014;39(10):1104-1112.
-
- causes
- depression
-
(and 5 more)
Tagged with:
-
Celiac.com 03/15/2016 - "Creating health comes down to the food we eat and how we choose to live our lives." – Dr. Terry Wahls Lots of people find it hard to believe that such a common food as wheat/gluten could possibly be implicated in causing skin diseases. They say something like this: "Everyone eats wheat, but not everyone gets skin troubles—so it can't be wheat!" This logic is flawed. I have written this book so that you can read all of the evidence about gluten-related skin disease in one place. "Cutaneous gluten sensitivity" is one of the new terms applied to the group of gluten-related skin diseases. Max belongs to this leg in the photo. He is very itchy and sore. He is 18-years old and not getting any better—in fact he has been getting worse. He came to me seeking help. Mum wrote, "Max has been suffering from debilitating dermatitis over his whole body for the last 3 years. He is withdrawn, self-conscious, covered with sores, and feels he will never get better. Unfortunately, the creams he is putting on just seem to irritate him." So, I am investigating him for gluten-related eczema. It will be a relief for him if the tests come out positive for gluten. What should be the strategy to get him better? I don't want him to go through the rest of his life like Elizabeth Whitesell, from the Gluten Zero Facebook page, who explains: "I was frantic with itching before my celiac diagnosis. The dermatologists never addressed the possibility of celiac, just gave me new treatments for my itching. I cannot name all of the creams, oils, pills and ointments I used, along with a blue-light treatment. Steroid shots, creams and pills were a major part of my treatment." "I received some temporary relief and never traveled without my creams. Itching on my hands was so fierce that I carried a frozen ice block (the kind used in coolers) in my purse. When we were at a public event, I gripped my hands around the ice to ward off a noisy itching attack. Ice was my godsend to keep the itching from following its neurological path. All of my blouses had blood dot stains from clawing my upper arms like I was an ape when into full-time mode." "My best treatment was freezing 2-liter bottles of water and holding them between my knees as I laid down to go to sleep. If I could fall asleep before the freaking stage began, I was on a roll. More frozen bottles were kept in a cooler by my bed for when the thaw came and I was too tired to walk downstairs to replace them." "What a saint of a husband I had. Once I went gluten-free, so many changes came for the better. I did not suddenly notice the absence of itching but, one day, looked back and realized I was not traveling and sleeping with frozen bottles anymore. I hope dermatologists are more informed now." Skin Diseases Associated with Celiac Disease Gluten is known to cause skin disease. Gluten can definitely cause itchy skin. Collectively, these skin-diseases provoked/triggered/caused by gluten can be called "cutaneous gluten sensitivity". This is an umbrella term which includes: Dermatitis Herpetiformis (DH); Celiac associated skin diseases; Non-celiac associated skin diseases. So what is the evidence? 1) Dermatitis Herpetiformis: To summarise the previous chapter, the classic skin complaint is dermatitis herpetiformis. It usually affects the elbows, knees, buttocks, scalp, and back. It begins as little bumps that then change into little blisters. People say that they are driven mad by the itching. It is caused by an immune reaction to gluten in the skin. Microscopic clumps of immune-complexes get deposited just under the skin. This creates the very itchy rash. These tiny particles of immunoglobulins can take years to clear up once you start on a gluten-free diet. It is reported that it can take up to ten years before you make a full recovery. 2) Celiac Associated Skin Diseases: Marzia Caproni and co-workers have detailed the skin diseases that have so far been associated with celiac disease (and perhaps by implication, with gluten). In their paper, "Celiac Disease and Dermatologic Manifestations: Many Skin Clues to Unfold Gluten-Sensitive Enteropathy" they include common skin complaints that most people do not associate with gluten-illness: Dermatitis Herpetiformis Psoriasis Alopecia Areata Chronic Urticaria Hereditary Angioneurotic Edema Cutaneous Vasculitis Atopic Dermatitis Eczema Vitiligo They also remind us that enamel defects, delayed eruption, recurrent aphthous ulcers, cheilitis, and atrophic glossitis are gluten-associate conditions and that "the diagnosis of celiac disease can sometimes be made from a smile!" Their important message is that anyone with any of these conditions should be investigated for celiac disease. 3) Non-celiac Associated Skin Diseases The skin is a frequent target organ in gluten-sensitivity. The skin, hair and teeth can all be disturbed by gluten. However, eczema is a much more common manifestation of gluten-sensitivity. Humbert and his dermatology colleagues (Gluten intolerance and skin diseases, 2006) wrote this about gluten and skin disease: "Gluten sensitivity, with or without celiac disease symptoms and intestinal pathology, has been suggested as a potentially treatable cause of various diseases. There have been numerous reports linking celiac disease with several skin conditions. Dermatitis herpetiformis is actually a skin manifestation of celiac disease. Autoimmune diseases, allergic diseases, psoriasis and miscellaneous diseases have also been described with gluten intolerance." "Dermatologists should be familiar with the appraisal of gluten sensitive enteropathy and should be able to search for an underlying gluten intolerance. Serological screening by means of anti-gliadin, anti-endomysial and tissue-transglutaminase antibodies should be performed. Gluten intolerance gives rise to a variety of dermatological manifestations which may benefit from a gluten-free diet." This is an important statement. In 2010, Korossy reported a skin eruption that he called "gluten-sensitive dermatitis" which he says is clinically indistinguishable from dermatitis herpetiformis but lacks the IgA connection. (Non-dermatitis herpetiformis gluten-sensitive dermatitis: a personal account of an unrecognized entity, Korossy, 2010). Cutaneous Gluten Sensitivity Bonciolini et al (2015) have made a study of the skin manifestations of people with Non-Celiac Gluten Sensitivity (NCGS) Cutaneous Manifestations of Non-Celiac Gluten Sensitivity: Clinical Histological and Immuno-pathological Features, Bonciolini et al 2015 They have adopted the term 'cutaneous gluten sensitivity'. They describe 17 consecutive patients affected by NCGS. They had excluded celiac disease and wheat allergy. They said: "The skin lesions observed were similar both to eczema and psoriasis and did not show a specific histological pattern. Furthermore, no serological marker was useful to identify these patients. The only data common to most of these patients affected by NCGS associated to non-specific skin manifestations are: the itching; the presence of C3 at the dermoepidermal junction; a rapid resolution of lesions when adopting the gluten free diet. Therefore, dermatologists must be familiar with the cutaneous manifestations and symptoms of gastrointestinal disorders. An appropriate understanding, work-up, consultation and management will help to identify the important cutaneous–gastrointestinal connection and ensuring that this important gastroenterological disease in patients with skin manifestations is not ignored. Finally, we suggest an accurate follow-up of all patients who report intense itching and gastrointestinal disorders, even when histology and morphology of the skin lesions do not identify a specific skin disease. We also suggest the adoption of gluten-free diet for at least three months assessing any positive effects." A Family Affected by Cutaneous Gluten Sensitivity Katrina Ojakaar writes this about the severe skin problems in her family that were eventually shown to be related to gluten-harm: "I had terrible eczema on my legs as a child. As an adult I had recurrent eczema on my eyelids and hands in addition to severe dry, itchy skin on my scalp, back, and legs. I also developed rosacea on my face that was treated unsuccessfully with antibiotics and topical ointments. At the age of 44, I had a lab test that showed gluten was making me sick. I immediately stopped eating food that contained gluten and within weeks watched my skin transform. I no longer have raw eczema patches or dry skin; and my rosacea has disappeared." "My daughter, Lila, had horrific diaper rash as an infant and nothing seemed to heal her sore bottom. Even as she grew out of diapers, her bottom was always irritated. Lila's skin was also very dry and irritated. Lotions and even plain bath water caused a sting. But when Lila stopped eating gluten, her skin simply healed. She now has smooth, soft, and moist skin without irritation and enjoys a relaxing bath." "My mother suffered from psoriasis on her legs and scalp until she stopped eating gluten at the age of 72. She is now 75, and the psoriasis has disappeared. Her skin is healthy, and she doesn't eat gluten, dairy, or oats." My father had rosacea on his face and was diagnosed with the autoimmune disease called lichen planus about 12 years ago. He had raw, bleeding sores on his scalp. And his fingernails and toenails disintegrated where he was left with only tender skin. Three years ago my dad stopped eating gluten, and two months later, his fingernails started to grow back. He now has a thin narrow layer of nail at the age of 80. The lesions related to his lichen planus disease on his scalp are gone. And, my father's rosacea, like mine, also healed when he stopped eating gluten." Keratosis Pilaris Keratosis pilaris, or sometimes called 'chicken skin' is blamed on gluten by many people. It is very common, occurring in about 10% of people, and there seems to be a hereditary nature to it. It tends to lessen with age, being prominent in toddlers. Any gluten connection remains speculative. Anne Luther writes: "One of the many pleasant surprises I had when I stopped eating gluten was the disappearance of three different skin rashes. There were non-itchy bumps on my back and arms, non-itchy red bumps on the soles of my feet and a very itchy rash on my legs behind my knees. None of these were ever diagnosed by a doctor but they all disappeared after I had totally eliminated gluten from my life." Keratosis pilaris is skin condition characterized by rough patches of skin caused by small, acne-like bumps. It is found mostly on the upper arms, upper thighs, and cheeks. It can feel a bit like sandpaper or goose-flesh. These little bumps are usually white, but can be red. They do not hurt. Sometimes they can feel a bit itchy. Keratosis pilaris seems to be caused by a build-up of keratin, the protein that helps create the protective skin barrier. Once keratin has formed into a hard plug at the opening of the hair follicle, this can block the oil and sweat glands. Consequently, these substances cannot escape out onto the skin, and results in these patches of rough, bumpy skin. I see a lot of keratosis pilaris in my Clinic. The gluten connection not clear, but many parents report its disappearance on a gluten-free diet. What happened to Max? Remember Max's legs at the beginning of this Chapter? Well it turned out that Max had two copies of the HLA gene DQ2 which gives him a 1-in-7 chance of developing celiac disease. It also increases his likelihood of having gluten sensitivity. However his blood tests for gluten (AGA) and celiac disease (tTG) were negative. But he did have evidence of a wheat allergy from his EAST tests. His total IgE levels were extremely high as well (over 4000), showing his heightened allergic status. So he has now embarked on a trial of a gluten-free diet. Mum says, "I feel that we are starting to get to the bottom of it now." It will be another 6 months before we know his results of his gluten-free diet. It can take a long time to heal. This was an excerpt from Dr Rodney Ford's latest eBook: "Dermatitis Eczema: Gluten Wheat – Solving the Eczema Puzzle." Available at: http://www.GlutenEczema.com
-
Celiac.com 08/29/2019 - Is the popular gluten-free fad dieting trend fueling a rise in mistaken claims of gluten sensitivity? There isn't much data on how overall rates of self-reported gluten sensitivity might be influenced by growing numbers of people who believe the gluten-free diet to be generally healthier, so-called "Life-stylers." A team of researchers recently set out to get some answers by repeating a population survey from 2012 in order to examine how attitudes towards gluten sensitivity have changed over time. The research team included ID Croall, N Trott, A Rej, I Aziz, DJ O'Brien, HA George, MY Hossain, LJS Marks, JI Richardson, R Rigby, M Hadjivassiliou, N Hoggard, and DS Sanders. They are variously affiliated with the University of Sheffield, Academic Unit of Radiology, Royal Hallamshire Hospital, Sheffield, UK., and the Academic Unit of Gastroenterology, Royal Hallamshire Hospital, Sheffield Teaching Hospitals NHS Foundation Trust, in Sheffield, UK. To replicate the 2012 experiment the team surveyed 1,004 subjects in Sheffield (UK) in 2015. The questionnaire included a survey on food frequency, and measured self-reported gluten sensitivity along with associated variables, including prevalence, current diet, and pre-existing conditions. Compared to the previous survey, associated variables and chi-squared analysis results showed rates of self-reported gluten sensitivity increasing from about 13% in 2012 to nearly 33% in 2015. Meanwhile, rates of pre-existing celiac disease increased from 0.8% in 2012 to 1.2% in 2015, while the percentage of people following a gluten-free diet remained 3.7%. People are much more likely to self-report gluten sensitivity if they had certain pre-existing conditions, including anxiety, depression, chronic fatigue, headaches, and other food allergies/intolerances, including irritable bowel syndrome (IBS), with chi-squared analyses, all p < 0.001. Over a 3-year period, the number of people who self-reported gluten sensitivity rose by over 250%. Despite the fact that rates of physiological gluten sensitivity remained about the same. This data suggests that the public perception of gluten as an unhealthy food is causing more and more people to erroneously believe they are gluten-sensitive, when if fact they are likely not sensitive to gluten. What do you think about the popularity of a gluten-free diet, and how it may change public perception of gluten-free foods? Read more in Nutrients. 2019 Jun 5;11(6). pii: E1276. doi: 10.3390/nu11061276.
-
Celiac.com 08/28/2019 - Do people who avoid gluten for lifestyle reasons actually have some sort of underlying health or medical condition that makes a gluten-free diet beneficial? Or, a simpler way to put the question: Who benefits from a gluten-free diet, and who does not? A team of researchers recently set out to see if people without celiac disease or gluten-intolerance, who eat a gluten-free diet, are gaining any benefit. The research team included Iain David Croall, Imran Aziz, Nick Trott, Paola Tosi, Nigel Hoggard, and David S. Sanders. They are variously affiliated with the Academic Unit of Radiology, University of Sheffield, Royal Hallamshire Hospital, Sheffield, United Kingdom; the Academic Unit of Gastroenterology, Royal Hallamshire Hospital, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom; and the University of Reading, School of Agriculture Policy and Development, Reading, United Kingdom. Although the gluten-free diet is necessary for people with celiac disease, non-celiac gluten sensitivity (NCGS), and other types of clinical gluten sensitivity, the scientific consensus is that gluten is safe for most people. Still, numerous celebrity and athlete endorsements of the gluten-free diet have promoted an image of gluten as “unhealthy,” leading numerous people to adopt the gluten-free diet as a lifestyle choice. American market research found that nearly half of all gluten-free food consumers do not have celiac disease or gluten-sensitivity, while nearly two-thirds believe that gluten-free food is generally healthier. This trend is partly responsible for the explosive growth in the worldwide gluten-free industry, which is projected to see revenues of about $4.7 billion in 2020. The researchers feel that the perception of the gluten-free diet as a "fad" has harmed people with celiac disease and gluten intolerance. They feel that clarifying exactly who will benefit from a gluten-free diet, and who will not, will help to inform the public and clinicians on these issues. For this reason, the team conducted that first double-blind randomized controlled trial (DRCT) of gluten in healthy control subjects, under the assumption that the gluten would not cause symptoms in people without gluten sensitivity. Volunteers attended 2 study sessions, and were then educated by a dietitian about a gluten-free diet and asked to follow a supported gluten-free diet for for 2 weeks. The researchers then measured gluten-free diet adherence using the Biagi score. For their study, the research team recruited unpaid adult volunteers with no diagnosed gluten-related disorders, who followed gluten-containing diets. The study aimed to recruit 30 subjects to divide into 2 groups. No previous data in healthy individuals are available, but NCGS DRCTs have reported gastrointestinal symptom changes induced by gluten, which would carry 89.2% power if observed within a group of n = 15. Volunteers received blood screens for celiac disease antibodies. The trial was supported by the personal research funds of Professor Sanders, and sought ethical approval from the Yorkshire and Humber Research. The results of the study show that gluten does not cause gastrointestinal symptoms in healthy people. Basically, people who eat gluten-free absent some clear medical benefit may be falling victim to public misconception of gluten, and likely gaining no health benefit from eating gluten-free. Read more at Science Direct.com
- 9 comments
-
- celiac disease
- gastrointestinal
-
(and 4 more)
Tagged with:
-
Celiac.com 08/27/2019 - Patients with gluten neuropathy often have peripheral neuropathic pain, indicating the involvement of small fibers. The most common types of peripheral neuropathy in people with celiac disease and gluten sensitivity are length-dependent symmetrical sensorimotor neuropathies and sensory ganglionopathies. A team of researchers recently set out to describe the clinical characteristics of patients with celiac disease or gluten sensitivity and pure small fiber neuropathy (SFN). The research team included Pangiotis Zis, PG Sarrigiannis, DG Rao, DS Sanders, and M Hadjivassiliou. They are variously affiliated with the Academic Department of Neurosciences, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, UK; and the Academic Unit of Gastroenterology, Sheffield Teaching Hospitals NHS Foundation Trust in Sheffield, UK. The research team reviewed the records for all patients referred to the Gluten-Related Neurological Disorders clinic with clinical and neurophysiological evidence of small fiber neuropathy. Blood screens indicated that all patients were gluten sensitive prior to starting a gluten-free diet. The team offered duodenal biopsy to all patients, except those patients with conditions that could cause small fiber neuropathy. The researchers found 9 males and 5 females with small fiber neuropathy and gluten sensitivity. Eleven of those patients underwent duodenal biopsy, and ten of those showed evidence of celiac disease enteropathy. Average age at onset of pain was 53.5 ± 11.4 years, while the average age of celiac disease/gluten sensitivity diagnosis was 50.8 ± 10.4 years. More than six out of ten patients reported feeling pain. Neurophysiological assessment suggested a length-dependent small fiber neuropathy in 11 patients, whereas in 2, a non-length dependent pattern was identified, suggesting that the predominant pathology lies in the dorsal root ganglia. This study reveals that small fiber neuropathy can be a feature of celiac disease and gluten sensitivity. The team recommends that patients with idiopathic small fiber neuropathy be screened for celiac disease and gluten sensitivity. Read more in Postgrad Med. 2019 Aug 6:1-5. doi: 10.1080/00325481.2019.1650609.
- 3 comments
-
- celiac disease
- gluten
-
(and 3 more)
Tagged with:
-
Celiac.com 02/15/2016 - Gluten sensitivities have been documented in some dogs, but now researchers have the first solid evidence that gluten is the culprit behind a movement disorder in Border Terriers known as Epileptoid Cramping Syndrome (CECS). There have been anecdotal reports that these dogs might respond to a gluten-free diet, but no clinical studies. This changed recently, when a team of researchers set out to assess the clinical and serological benefits of a gluten-free diet in Bornder Terriers with CECS. The research team included M. Lowrie, O. A. Garden, M. Hadjivassiliou, R.J. Harvey, D.S. Sanders, R. Powell, and L. Garosi. They are variously associated with the Davies Veterinary Specialists in Hitchin, UK, the Department of Clinical Sciences and Services of Royal Veterinary College in Hatfield, UK., the Department of Neurology at Royal Hallamshire Hospital in Sheffield, UK., the Department of Pharmacology, UCL School of Pharmacy in London, UK., the Department of Gastroenterology at Royal Hallamshire Hospital, Sheffield, UK., and with Powell Torrance Diagnostic Services in Higham Gobion, UK. The team evaluated a group of six client-owned Bornder Terriers with clinically confirmed CECS. The dogs all had at least a 6-month history of CECS, with their symptoms observed and confirmed using video, and each had exhibited at least 2 separate episodes on different days. The team tested the dogs for anti-transglutaminase 2 (TG2 IgA) and anti-gliadin (AGA IgG) antibodies at presentation, and 3, 6, and 9 months after the introduction of a gluten-free diet. They performed duodenal biopsy on 1 dog. Their results showed that, upon presentation, 6 of 6 dogs had increased serum TG2 IgA levels (P = .006), and 5 of 6 dogs had increased AGA IgG levels, compared to those of controls (P = .018). After 9 months on a strict gluten-free diet, 5 of the 6 dogs showed clinical and serological improvement with CECS. The one dog that had persistently high antibody levels apparently scavenged local horse manure, which contained gluten. However, this dog, too improved after the introduction of a strict gluten-free diet. So, all of the affected dogs eventually responded favorably to a gluten-free diet. To further demonstrate the connection, two dogs suffered relapses after gluten was reintroduced into their diets. In Border Terriers, canine epileptoid cramping syndrome is caused, and perpetuated by, an adverse reaction to gluten, and thus responds well to a gluten-free diet. The takeaway for owners of Border Terriers is to keep an eye on their dogs, and work with their vets if they suspect canine epileptoid cramping syndrome; which can be effectively treated with a gluten-free diet. Source: J Vet Intern Med. 2015 Nov;29(6):1564-8. doi: 10.1111/jvim.13643. Epub 2015 Oct 25.
- 2 comments
-
Celiac.com 04/10/2017 - Fibromyalgia syndrome is a debilitating condition of unknown cause, and only treatment approaches at present offer only limited relief from symptoms. Some fibromyalgia sufferers seem to benefit from a gluten-free diet, but there's not a great amount of data on the benefits of a gluten-free diet in fibromyalgia sufferers who do not have celiac disease. A team of researchers recently set out to describe 20 selected patients with fibromyalgia, but without celiac disease, whose symptoms improved when they followed a gluten-free diet. The research team included Carlos Isasi, Isabel Colmenero, Fernando Casco, Eva Tejerina, Natalia Fernandez, José I. Serrano-Vela, Maria J. Castro, and Luis F. Villa. They are variously associated with the Department of Rheumatology, Hospital Puerta de Hierro, Majadahonda Madrid, Spain; the Department of Pathology, Hospital Infantil Niño Jesús, Madrid, Spain; the Department of Pathology, Hospital Puerta de Hierro, Majadahonda Madrid, Spain; the Department of Gastroenterology, Hospital Puerta de Hierro, Majadahonda Madrid, Spain; the Celiac and Gluten Sensitive patients Association of Madrid, Madrid, Spain; and with the Department of Immunology, Hospital Doce de Octubre, Madrid, Spain. What researchers now call non-celiac gluten-sensitivity is a daily common, yet treatable condition, with a range of symptoms that dovetail with many symptoms of fibromyalgia, including chronic musculoskeletal pain, asthenia, and irritable bowel syndrome. All patients underwent anti-transglutaminase assay, duodenal biopsy, and HLA typing. To rule out celiac disease in their test subjects, the research team used negative anti-transglutaminase assay results, together with the absence of villous atrophy in the duodenal biopsy. All patients showed signs of intraepithelial lymphocytosis with no villous atrophy. The doctors defined a positive clinical response as the achievement of at least one of the following: remission of fibromyalgia-associated pain, return to work, return to normal life, or the discontinuation of opioids. Doctors followed on the patients from 5 to 31 months, with a follow-up period of 16 months, on average. The level of widespread chronic pain improved dramatically for all patients; for 15 patients, chronic widespread pain was no longer present, indicating remission of FM. Fifteen patients returned to work or normal life. In three patients who had been previously treated in pain units with opioids, these drugs were discontinued. Fatigue, gastrointestinal symptoms, migraine, and depression also improved together with pain. Patients #2 and #3, both with oral aphthae, went into complete remission for psoriatic arthritis and undifferentiated spondyloarthritis. These results strengthen the idea that non-celiac gluten sensitivity may play a key role in the development of fibromyalgia syndrome. Source: Rheumatol Int. 2014; 34(11): 1607–1612. Published online 2014 Apr 12. doi: 10.1007/s00296-014-2990-6
- 5 comments
-
Celiac.com 05/01/2019 - In the last decade, researchers have learned a great deal about gluten and celiac disease. More recently, there's been greater focus on non-celiac gluten-related disorders, especially the role of gluten in non-celiac gluten sensitivity (NCGS) and irritable bowel syndrome (IBS). These conditions share some significant common connections. For example, a low FODMAP diet may help some people with both IBS, and NCGS. For many people the symptoms of IBS, and NCGS can be similar, making it hard to distinguish between the two conditions. Both IBS and NCGS can mimic celiac disease, though there are some key differences. Researchers Anupam Rej and David S. Sanders recently published a review exploring the complex relationship between the two disorders. They point out that recent data shows that gluten triggers symptoms in people with NCGS, and that gluten can trigger celiac-like symptom generation in patients with IBS. Researchers are also increasingly looking at non-gluten components of wheat as possible triggers for symptoms in both conditions. Overall, there appears to be significant overlap between IBS and NCGS. It is likely that a subset of patients presenting with IBS actually have NCGS. It's also likely that people with IBS have symptoms triggered by gluten. Until researchers better understand both conditions, along with the role of wheat components in triggering symptoms, further research is required to help distinguish between both, and to delineate any connections between the two. Read more in Current Opinion in Gastroenterology 2019;35(3):199-205 (login required).
- 1 comment
-
- celiac disease
- gluten
- (and 4 more)
-
Celiac.com 02/15/2019 - Answer this question honestly for yourself. Not for me, or for anyone else, answer this question honestly for yourself. On a scale from 1 to 10, if 10 is the amount of energy you should have in life, and 5 is half as much… now, hold on a minute, one more thing, take your will power out of the equation… what’s your body energy? If you weren’t pushing yourself, motivating yourself to continue on, what is the level of energy your body is operating on? On a 1-10 scale? Most of us have a number we come up with right away as the first part of the question is being asked: “Oh, I’m an eight or a nine”. But when I ask patients to take their will power out of the equation, many will have a look come across their face, almost like a balloon being deflated a little, and they’ll say “three” or “five”. Rarely do I have someone who answers eight or above. Where is this fatigue coming from? Many clinicians will tell you one of the most common symptoms of food allergies and food sensitivities is fatigue. Although the majority of individuals with gluten sensitivity and/or celiac disease experience substantial improvement within the first few weeks of gluten withdrawal, between 7% and 30% continue to have symptoms or clinical manifestations suggestive of celiac disease despite being on a gluten-free diet(1). That’s called non-responsive celiac disease--the body is not responding the way it should. Why is that? And why is it that so many of us do not experience the amount of energy we should feel given that we’re being so careful to avoid exposure to gluten, a food that is toxic to us? We’ll look, in this article, at a common, hidden source of this lack of vitality and lack of response to a gluten-free diet. Non-responsive celiac disease (NRCD) has been defined as: referral to a clinician specializing in celiac disease for the evaluation of a lack of response to a gluten-free diet, failure of clinical symptoms or laboratory abnormalities typical of celiac disease to improve within six months of gluten withdrawal, recurrence of symptoms and/or laboratory abnormalities typical of CD while on a gluten-free diet. In one study, 12 identified causes of NRCD, the most common cause was (inadvertent) gluten exposure, accounting for 36% of patients(2). OK, that’s understandable. But what about the other 64% who did not have an inadvertent exposure to wheat or similar grains? What is the cause of their NRCD? An all-too-common contributor to NRCD is sensitivity to other foods commonly consumed on a gluten-free diet causing a very similar inflammatory cascade in the intestines. Another contributor is cross-reactivity of antibodies against gluten with exposure to other foods. On a gluten-free diet, we may substitute other grains in much larger amounts than we may have eaten when we were on a gluten-containing diet. In some cases, this may initiate an immune response very similar to that caused by eating gluten. Cross-reactivity is the ability of an antibody to bind to similar-looking parts on different proteins called epitopes. This phenomenon is also known as molecular mimicry. In such a case the immune system confuses one food for another. Therefore, certain foods appear, to the immune system, sufficiently similar to a reactive food to initiate an immune response. Patients with gluten sensitivity and celiac disease may be sensitized to a broad range of dietary proteins from different foods due to cross-reactivity. Below is a drawing of what happens when the gliadin protein molecule from wheat (labeled #1) fits into the ‘docking station’ of a wheat antibody. It fits into all three locks of the docking station. This is termed a reactive antibody. And in gluten sensitive individuals, the immune system is activated to make more antibodies to fight this invader. As we all know, that is not a problem unless we eat the offending food so often that it overwhelms the body and begins causing a great deal of damage to the intestines and other tissues (pancakes for breakfast, sandwich for lunch, pasta for dinner, toast for breakfast, sandwich for lunch, croutons on the salad at a dinner, and maybe a cookie or piece of cake,..). Next we see how some foods (such as casein from dairy) can bind to a gliadin antibody. It fits into two of the three ‘docking stations’ and that is enough to trigger an immune response as if this person was eating gluten. This will still trigger an immune response. That food is called a ‘cross-reactive’ food. In the third drawing we see how other foods (such as rice) may bump into a gliadin antibody, but it only fits into one docking station, or no docking station and thus will not bind to it. This is similar to putting a round peg in a square hole - can’t do it. It is ignored by the gliadin antibody. With wheat the estimated prevalence of a cross-reactivity with rye and barley is one out of five (20%) (3). Cross reaction with dairy in different studies varies from 50 to 91%(4,5). Up to 82% of patients with celiac disease have antibodies to other foods including rice flour, milk, beef, sheep and egg(6). Other studies have identified cross-reactivity with chocolate(7), sesame(8,9,10,11,12), hemp(13), rye(14), kamut(15,16), buckwheat (17,18,19,20,21,22,23,24,25), sorghum(26,27,28,29,30), millet(31,32,33,34), spelt(35,36,37,38), amaranth(39,40,41), quinoa(42,43,44), yeast(45,46,47,48,49), tapiocal(50,51,52,53), oats(54,55,56,57,58,59), coffee(60,61,62,63,64), corn(65,66,67), ricel(68,69,70,71,72), potato(73,74,75). The response to some of these food allergens parallels the response to the gluten protein in wheat with increased IgA antibodies and might be relevant to the ongoing immune response of gluten sensitivity and celiac disease without eating gluten(76). Perhaps this is why as many as 40% of children on a well-managed gluten-free diet for at least 1 year still have elevated antibodies to gluten(77). From the diagnostic and therapeutic point of view, it makes sense to define allergen clusters (cross-reactivity)(78). Determination of serum IgA and IgG antibody activities to dietary proteins appears to be a valuable adjunct in the diagnosis and follow-up of celiac disease, both in children and adults. Increased IgA activities to other dietary antigens are likewise relatively characteristic of untreated celiac disease; monitoring of such antibodies may be particularly helpful in evaluating the response of patients on a gluten free diet(79). Foods that may create cross-reactivity with gluten include cow’s milk, casein, casomorphin, American cheese, chocolate, rye, barley, kamut, spelt, yeast, oats, and coffee. Common foods often included on a gluten-free diet that one may be sensitive to that could cause continued inflammation include sesame, rice, corn, potato, hemp, buckwheat, sorghum, millet, amarath, quinoa, and tapioca. This array of 24 different foods (some are possible sensitivities while others are possible cross-reactive foods) is available from CyrexLabs.com. Ask your Health Care Practitioner to look into this array. You might want to consider that, when a gluten-free diet is not producing the results that you had hoped for, the cause may be another common food. If you are working so hard to be in control of the quality and the selection of the foods you eat, this concept of cross-reactivity may be a missing-link that will help you get closer to feeling great and answering that initial question “On a 1-10...” with a passing grade of 7 or higher. Dr. Thomas O’Bryan is a nationally recognized speaker and workshop leader specializing in Gluten Sensitivity and Celiac Disease. He is the Sherlock Holmes for chronic disease and metabolic disorders. He is a clinician par excellence in treating chronic disease and metabolic disorders from a Functional Medicine Perspective. He holds teaching Faculty positions with the Institute for Functional Medicine and The National University of Life Sciences. Dr. O’Bryan is always one of the most respected, highly-appreciated Speakers. Dr. O’Bryan’s passion is in teaching the many manifestations of Gluten Sensitivity and Celiac Disease as they occur inside and outside of the intestines. Dr. O’Bryan welcomes your questions about gluten sensitivity and/or functional medicine. Please send your questions and requests by email to www.theDr.com. References: 1. Green P, Cellier C, Celiac Disease NEJM 357;17 Oct 25, 2007 2. Leffler DA, Dennis M, Hyett B, Kelly E, Schuppan D, Kelly CP., Etiologies and predictors of diagnosis in nonresponsive celiac disease, Clin Gastroenterol Hepatol. 2007 Apr;5(4):445-50 3. Sicherer SH., Clinical implications of cross-reactive food allergens, J Allergy Clin Immunol. 2001 Dec;108(6):881-90 4. Kristjánsson G, Venge P, Hällgren R., Mucosal reactivity to cow’s milk protein in coeliac disease, Clin Exp Immunol. 2007 Mar;147(3):449-55 5. Bürgin-Wolff A, Hernandez R, Just M, Signer E., Immunofluorescent antibodies against gliadin: a screening test for coeliac disease, Helv Paediatr Acta. 1976 Dec;31(4-5):375-80 6. Ferguson A, Carswell F, Precipitins to dietary proteins in serum and upper intestinal secretions of coeliac children, Br Med J. 1972 Jan 8;1(5792):75-7 7. Becker CG, Van Hamont N, Wagner M. Tobacco, cocoa, coffee, and ragweed: cross-reacting allergens that activate factor-XII-dependent pathways. Blood, 1981; 58(5):861-867. 8. Gangur V, Kelly C, Navuluri L. Sesame allergy: a growing food allergy of global proportions? Ann Allergy Asthma Immunol, 2005; 95:4-11. 9. Kagi Mk, Wuthrich B. Falafel burger anaphylaxis due to sesame seed allergy. Ann Allergy, 1993; 71(2):127-129. 10. Keskinen H, Ostman P, Vaheria E, et al. A case of occupational asthma, rhinitis and urticaria due to sesame seed. Clin Exp Allergy, 1991; 21:623-624. 11. Pecquet C, Leynadier F, SaÏag P. Immediate hypersensitivity to sesame in foods and cosmetics. Contact Dermatitis, 1998; 39:313. 12. Perkins MS. Raising awareness of sesame allergy. Pharma J, 2001; 267:757-758 13. Popa V, Gavrilescu N, Preda N, et al. an investigation of allergy in byssinosis: sensitization to cotton, hemp, flax and jute antigens. Brit J Industr Med, 1969; 26:101-108 14. Ciclitiera PJ and Ellis HJ. Relation of antigenic structure of cereal proteins to their toxicity in coeliac patients. Brit J Nutr, 1985; 53:39-45 15. Kasarda DD. Grains in relation to celiac disease. Cereal Foods World, 2001; 46:209-210. 16. Simonato B, Pasini G, Giannattasio M, Curioni A. Allergenic potential of Kamut wheat. Allergy, 2002; 57:653-654. 17. Göhte C-J, Wislander G, Ancker K, Forsbeck M. bucksheat allergy: health food, an inhalation health risk. Allergy, 2007; 38(3):155-159 18. Hekkens WT. The determination of prolamins in gluten-free food. Introductory remarks. Panminerva Med, 1991; 33(2):61-64 19. Kim J-L, Wieslander G, Norbäck D. Allergy/Intolerance to buckwheat and other food products among Swedish subjects with celiac disease. Proc. 9th Int’l Symp Buckwheat, Prague, 2004:705-709 (74) 20. Lee SY, Lee KS, Hong CH, Lee KY. Three cases of childhood nocturnal asthma due to buckwheat allergy. Allergy, 2001; 56:763-766 21. Pomeranz Y, Marshall HG, Robbins Gs, Gilbertson JT. Protein contect and amino acid composition of maturing buckwheat (Fagopyrum esculentim moench). Cereal Chem, 1975; 52:479-484 (76) 22. De Maat-Bleeker F, Stapel SO. Cross-reactivity between buckwheat and latex. Allergy, 1998; 53:538-539 23. Sdepanian VL, Scaletsky ICA, Fagundes-Neto U, de Morais MB. Assessment of gliadin in supposedly gluten-free foods prepared and purchased by celiac patients. J Ped Gastroenterol Nutr, 2001; 32:65-70 24. Skerritt JH, Devery JM, Hill AS. Chemistry, coeliac-toxicity and detection of gluten and related prolamins in foods. Panminerva Med, 1991; 33(2):65-74 25. Wieslander G, Norbäck D. Buckwheat allergy. Allergy, 2001; 56:703-704 26. Bietz JA. Cereal prolamin evolution and homology revealed by sequence analysis. Biochm Gentics, 1982; 20(11/12):1039-1053 27. Cicek M and Esen A. Stucture and expression of a dhurrinase (O-glucosidase) from sorghum. Plant Physiol, 1998; 116:1469-1478 28. Mazhar H, Chandrashekar A, Shetty HS. Isolation and immunochemical characterization of the alcohol-extractabel proteins (kafirins) of Sorghum bicolor (L.) Moench. J Cereal Sci, 1993; 17(1):83-93. 29. Taylor JRN, Sch ssler L, van der Walt WH. Fractionation of proteins from low-tannin sorghum grain. J Agric Food Chem, 1984; 32:149-154. 30. Gaitan E, Cooksey RC, Legan J, Lindsay RH. Antithyroid effects invivo and invitro of vitexin: a C-glucosylflavone in millet. J Clin Endocrinol Metab, 1995; 80(4):114-1147. 31. Monteiro PV, Virupaksha TK, Rao DR. Proteins of Italian millet: amino acid composition, solubility fractionation and electrophoresis of protein fractions. J Sci Food Agric, 1982; 33(11):1072-1079. 32. Monteiro PV, Sudharhsna L, Ramachandra G. Japanese barnyard millet (Echinochloa frumentacea): protein content, quality and SDS-PAGE of protein fractions. J Sci Food Agric, 1988; 43(1):17-25. 33. Parameswaran KP and Thayumanavan B. Homologies between prolamins of different minor millets. Plant Foods Human Nutr, 1995; 48:119-126. 34. Parameswaran KP and Thayumanavan B. Isolation and characterization of a 20 kD prolamin from kodo millet (Paspalum scrobiculatum) (L.): homology with other millets and cereals.. Plant Foods Human Nutr, 1997; 50:359-373. 35. Grela ER. Nutrient composition and content of antinutritional factors in spelt (Triticum spelta L.) cultivars. J Sci Food Agric, 1996; 71(3):399-404. 36. Jones SM, Megnolfi CG, Cooke SK, Sampson HA. Allergens, IgE, mediators, inflammatory mechanisms: immunologic cross-reactivity among cereal grains and grasses in children with food hypersensitivity. J Allergy Clin Immunol, 1995; 96:341-351. 37. Pastorello EA, Farioli L, Robino A, et al. A lipid transfer protein involved in occupational sensitization to spelt. J Allergy Clin Immunol, 2001; 108(1):145-146. 38. Skrabaqnja V, Kovac B, Golob T, et al. Effect of spelt wheat flour and kernel on bread composition and nutritional characteristics. J Agric Food Chem, 2001; 49:497-500. 39. Aphalo P, Castellani OF, Martinez EN, Anón MC. Surface phyusicochemical properties of globulin-P amaranth protein. J Agric Food Chem, 2004; 52:616-622. 40. Gorinstein S, Delgado-Licon E, Pawelzik E, et al. Characterization of soluble amaranth and soybean proteins based on fluorescence, hydrophobicity, electrophoresis, amino acid analysis, circular dichroism, and differential scanning calorimetry measurements. J Agric Food Chem, 2001; 49:5595-5601. 41. Vasco-Méndez NL and Paredes-López O. antigenic homology between amaranth glutelins and other storage proteins. J Food Biochem, 1995; 18(4):227-238. 42. Aluko RE and Monu E. Functional and bioactive properties of quinoa seed protein hydrolysates. J Food Sci, 2003; 68(4):1254-1258. 43. Lee AR, Ng DL, Dave E, et al. The effect of substituting alternative grains in the diet on the nutritional profile of the gluten-free diet. J Hum Nutr Diet, 2009; 22:359-363. 44. Wright KH, Huber KC, Fairbanks DJ, Huber CS. Isolation and characterization of Atriplex hortensis and sweet Chenopodium quinoa starches. Cereal Chem, 2002; 79(5):715-719. 45. Heelan Bt, Allan S, Barnes RMR. Identification of a 200-kDa glycoprotein antigen of Saccharomyces cerevisiae. Immunol Lett, 1991; 28:181-186. 46. Oshitani N, Hato F, Kenishi S, et al. Cross-reactivity of yeast antigens in human colon and peripheral leukocytes. J Pathol, 2003; 199:361-367. 47. Sendid B, Quinton JF, Charrier G, et al. Anti-Saccharomycies cerevisiae mannan antibodies in familial Crohn’s disease. Am J Gastroenterol, 2001; 93(8):1306-1310. 48. Vojdani A, Rahimian P, Kalhor H, Mordechai E. Immunological cross reactivity between candida albicans and human tissue. J Clin Lab Immunol, 1996; 48:1-15. 49. Young Ca, Sonnenberg A, Berns EA. Lymphocyte proliferation response to baker’s yeast in Crohn’s disease. Digestion; 1994:55(1):40-43. 50. Beezhold DH, Sussman GL, Liss GM, Chang NS. Latex allergy can induce clinical reactions to specific foods. Clin Exp Allergy, 1996; 26(4):416-422. 51. Brehler R, Theissen U, Hohr C, Luger T. “Latex-fruit syndrome”: frequency of cross-reacting IgE antibodies. Allergy, 1997; 52:404-410. 52. Ibero M, Castillo MJ, Pineda F. Allergy to cassava: a new allergenic food with cross-reactivity to latex. J Investig Allergol Clin Immunol, 2007; 17(6):409-412. 53. Mikkola JH, Alenius H, Kalkkinen N, et al. Hevein-like protein domains as a possible cause for allergen cross-reactivity between latex and banana. J Allergy Clin Immunol, 1998; 102:1005-1012. 54. Arentz-Hansen H, Fleckenstein B, Molberg Ø, et al. The molecular basis for oat intolerance in patients with celiac disease. PLoS Med, 2004 1(1):084-092. 55. Janatuinen EK, Pekka HP, Kemppainen TA, et al. A comparison of diets with and without oats in adults with celiac disease. N Engl J Med, 1995; 333:1033-1037. 56. Reunala T, Collin P, Holm K, et al. Tolerance to oats in dermatitis herpetiformis. Gut, 1998; 43:490-493. 57. Silano M, Dessì M, De Vincenzi M, Cornell H. In Vitro tests indicate that certain varieties of oats may be harmful to patients with coeliac disease. J Gastroenterol Hematol, 2007; 22:528-531. 58. Srinivasan U, Jones E, Carolan J, Feighery C. Immunohistochemical analysis of coeliac mucosa following ingestion of oats. Clin Exp Immunol, 2006; 144:197-203. 59. Thompson T. Gluten contamination of commercial oat products in the United States. N Engl J Med. 2004; 351(19):2021-2022. 60. Axelsson IG. Allergy to the coffee plant. Allergy, 1994; 49(10):885-887. 61. Caballero Tm, Garcia-Ara C, Pascual C, et al. Urticaria induced by caffeine. J Investig Allergol Clin Immunol, 1993; 3(3):160-162. 62. Moneret-Vautrin DA, Kanny G, Faller JP, et al. [Severe anaphylactic shock with heart arrest caused by coffee and gum Arabic, potentiated by beta-blocking eyedrops].[Article in French] Rev Med Interne, 1993; 14(2):107-111. 63. Osterman K, Johansson SG, Zetterström O. Diagnostic tests in allergy to green coffee. Allergy, 1995; 40(5):336-343. 64. Treudler R, Tebbe B, Orfanos CE. Coexistence of type I and type IV sensitization in occupational coffee allergy. Contact Dermatitis, 1997; 36:109. 65. Davidson IW, Lloyd RS, Whorwell PJ, Wright R. Antibodies to maize in patients with Crohn’s disease, ulcerative colitis and coelic disease. Clin Exp Immunol, 1979, 35:147-148. 66. Lehrer SB, Reese G, Malo J-L, et al. Corn Allergens: IgE antibody reactivity and crossreactivity with rice, soy, and peanut. Int Arch Allergy Immunol, 1999; 118:298-299. 67. Paulis JW and Bietz JA. Separation of alcohol-soluble maize proteins by reversed-phase high performance liquid chromatography. J Cereal Sci, 4986; 4:205-216. 68. Asero R, Amato S, Alfieri B, et al. Rice: another potential cause of food allergy in patients sensitized to lipid transfer protein. Int Arch Allergy Immunol, 2007; 143:69-74. 69. Horikoshi M, Kobayashi H, Yamazoe Y, et al. Purification and complete amino acid sequence of a major prolamin of rice endosperm. J Cereal Sci, 1991; 14(1):1-14. 70. Urisu A, Yamada K, Masuda S, et al. 16-kilodalton rice protein is one of the major allergens in rice grain extract and responsible for cross-allergenicity between cereal grains in the poaceae family. Int Arch Allergy Immunol, 1991; 96(3):244-252. 71. Wen T-N and Luthe DS. Biochemical characterization of rice glutelin. Plant Physiol, 1985; 78:172-177. 72. Yamada K, Urisu A, Komada H, et al. [Involvement of rice protein 16KD in crossallergenicity between antigens in rice, wheat, corn, Japanese millet, Italian millet].[Article in Japanese] Arerugi, 1991; 40(12):1485-1495. 73. Racusen D and Foote M. A major soluble glycoprotein of potato tubers. J Food Biochem, 1980; 4(1):43-52. 74. Vos-Scheperkeuter GH, De Boer W, Visser RGF, et al. Identification of granule-bound starch synthase in potato tubers. Plant Physiol, 1986; 82:411-416. 75. Vos-Scheperkeuter GH, de Wit JG, Ponstein AS, et al. Immunological comparison of the starch branching enzymes from potato tubers and maize kernels. Plant Physiol, 1989; 90:75-84. 76. Hvatum M, Scott H, Brandtzaeg P., Serum IgG subclass antibodies to a variety of food antigens in patients with coeliac disease, Gut. 1992 May;33(5):632-8. 77. Husby S, Foged N, Oxelius VA, Svehag SE,Serum IgG subclass antibodies to gliadin and other dietary antigens in children with coeliac disease,Clin Exp Immunol. 1986 Jun;64(3):526-35. 78. Breiteneder H, Ebner C., Molecular and biochemical classification of plant-derived food allergens, J Allergy Clin Immunol. 2000 Jul;106(1 Pt 1):27-36. Review. 79. Scott H, Fausa O, Ek J, Brandtzaeg P., Immune response patterns in coeliac disease. Serum antibodies to dietary antigens measured by an enzyme linked immunosorbent assay (ELISA), Clin Exp Immunol. 1984 Jul;57(1):25-32.
- 2 comments
-
- cross reactive
- cross-reactivity
- (and 3 more)
-
Celiac.com 06/13/2012 - In general, doctors and researchers know a good deal about how celiac disease works, and they are finding out more all the time. However, they know very little about non-celiac gluten sensitivity (NCGS). In an effort to learn more about non-celiac gluten sensitivity, a team of researchers recently carried out a study to measure the presence of somatization, personality traits, anxiety, depression, and health-related quality of life in NCGS individuals, and to compare the results with celiac disease patients and healthy control subjects. They also compared the response to gluten challenge between patients with non-celiac gluten sensitivity and those with celiac disease. The research team included M. Brottveit, P.O. Vandvik, S. Wojniusz, A. Løvik, K.E. Lundin, and B. Boye, of the Department of Gastroenterology at Oslo University Hospital, Ullevål in Oslo, Norway. In all, the team looked at 22 patients with celiac disease and 31 HLA-DQ2+ NCGS patients without celiac disease. All patients were following a gluten-free diet. Over a three day period, the team challenged 17 of the celiac disease patients with orally ingested gluten. They then recorded the symptoms reported by those patients. They did the same with a group of 40 healthy control subjects. The team then had both patients and healthy control subjects complete questionnaires regarding anxiety, depression, neuroticism and lie, hostility and aggression, alexithymia and health locus of control, physical complaints, and health-related quality of life. Interestingly, patients with non-celiac gluten sensitivity reported more abdominal (p = 0.01) and non-abdominal (p < 0.01) symptoms after the gluten challenge than patients with celiac disease. The increase in symptoms in non-celiac gluten sensitivity patients was not related to personality. However, the two groups both reported similar responses regarding personality traits, level of somatization, quality of life, anxiety, and depressive symptoms. Responses for both groups were about the same as for healthy controls. The results showed that patients with non-celiac gluten sensitivity did not show any tendencies toward general somatization, as both celiac disease patients and those with non-celiac gluten sensitivity showed low somatization levels. Source: Scand J Gastroenterol. 2012 Apr 23.
-
Celiac.com 02/20/2017 - Nickel is the most common cause of contact allergy, and nickel exposure can result in systemic nickel allergy syndrome, which mimics irritable bowel syndrome (IBS). Nickel is also found in wheat, which invites questions about possible nickel exposure from wheat in some cases of contact dermatitis. However, nickel hasn't really been studied in relation to glutenâ€related diseases. A research team recently set out to evaluate the frequency of contact dermatitis due to nickel allergy in NCWS patients diagnosed by a doubleâ€blind placeboâ€controlled(DBPC) challenge, and to identify the characteristics of NCWS patients with nickel allergy. The research team included Alberto D'Alcamo, Pasquale Mansueto, Maurizio Soresi, Rosario Iacobucci, Francesco La Blasca, Girolamo Geraci, Francesca Cavataio, Francesca Fayer, Andrea Arini, Laura Di Stefano, Giuseppe Iacono, Liana Bosco, and Antonio Carroccio. The are variously affiliated with the Dipartimento di Biologia e Medicina Interna e Specialistica (DiBiMIS), Internal Medicine Unit, University Hospital, Palermo, Italy; the Surgery Department, University Hospital, Palermo, Italy; Pediatric Unit, "Giovanni Paolo II" Hospital, Sciacca (ASP Agrigento), Italy; DiBiMIS, Gastroenterology Unit, University Hospital, Palermo, Italy; Pediatric Gastroenterology Unit, "ARNAS Di Cristina" Hospital, Palermo, Italy; Dipartimento di Scienze e Tecnologie Biologiche Chimiche e Farmaceutiche (Ste.Bi.CeF), University of Palermo, Palermo, Italy. Their team conducted a prospective study of 54 women and 6 men, with an average age of 34.1 year, and diagnosed with NCWS from December 2014 to November 2016. They also included a control group of 80 age†and sexâ€matched subjects with functional gastrointestinal symptoms. Patients reporting contact dermatitis related to nickelâ€containing objects were given a nickel patch sensitivity test. The tests showed that six out of sixty patients (10%) with NCWS suffered from contact dermatitis and nickel allergy, and this frequency was statistically higher than observed in the 5 percent seen in the control group. Compared to NCWS patients who did not suffer from nickel allergy, NCWS patients with nickel allergy commonly showed a higher rates of skin symptoms after wheat consumption. Contact dermatitis and nickel allergy are more frequent in NCWS patients than in subjects with functional gastrointestinal disorders. Moreover, large numbers of these patients showed cutaneous manifestations after wheat ingestion. Nickel allergy should be evaluated in NCWS patients who have cutaneous manifestations after wheat ingestion. More study is needed to determine the relationship between nickel sensitivity and NCWS. Source: Nutrients 2017, 9(2), 103; doi:10.3390/nu9020103
- 3 comments
-
- contact
- dermatitis
-
(and 5 more)
Tagged with:
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8-M):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8-M):