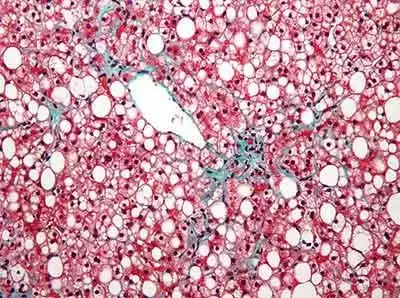
Celiac.com 06/29/2015 - Non-alcoholic fatty liver disease is a common cause of chronic liver disease. There's good data showing that celiac disease changes intestinal permeability, and that treatment with a gluten-free diet often causes weight gain, but so far there is scant documentation of non-alcoholic fatty liver disease in patients with celiac disease.
A team of researchers recently set out to assess increased risk of non-alcoholic fatty liver disease following diagnosis of celiac disease. The research team include Norelle R. Reilly, Benjamin Lebwohl, Rolf Hultcrantz, Peter H.R. Green, and Jonas F. Ludvigsson. They are affiliated with the Department Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden, and the Department of Pediatrics at Örebro University Hospital, Örebro University in Örebro, Sweden.
Celiac.com Sponsor (A12):
The team assessed the for risk of non-alcoholic fatty liver disease diagnosed from 1997 to 2009 in 26,816 individuals with celiac disease to 130,051 matched reference individuals.
The team excluded patients with any liver disease prior to celiac disease. They also excluded individuals with a lifetime diagnosis of alcohol-related disorder to minimize misclassification of non-alcoholic fatty liver disease. They used Cox regression estimated hazard ratios for non-alcoholic fatty liver disease.
Their results showed that over 246,559 person-years of follow-up, 53 individuals with celiac disease had a diagnosis of non-alcoholic fatty liver disease (21/100,000 person-years).
In comparison, in the reference group showed 85 individuals diagnosed with non-alcoholic fatty liver disease during 1,488,413 person-years (6/100,000 person-years).
This corresponded to a hazard ratio of 2.8 in the celiac group (95% CI), with the highest risk estimates of 4.6 seen in children (95% CI).
The risk increase in the first year after celiac disease diagnosis was 13.3 (95% CI), but remained significantly elevated at 2.5 even beyond 15 years after celiac diagnosis of celiac disease (95% CI).
Individuals with celiac disease do have an increased risk of non-alcoholic fatty liver disease compared to the general population.
Excess risks were highest in the first year after celiac disease diagnosis, but continued at least 15 years after celiac diagnosis. This much more comprehensive study provides much clearer and convincing data than any of the previous studies, and will likely serve as a baseline that clinicians have been lacking to this point.
Source:
- Open Original Shared Link




.thumb.jpg.7bad51ed6a943bd2a58c19e3dee802d5.jpg)


Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now