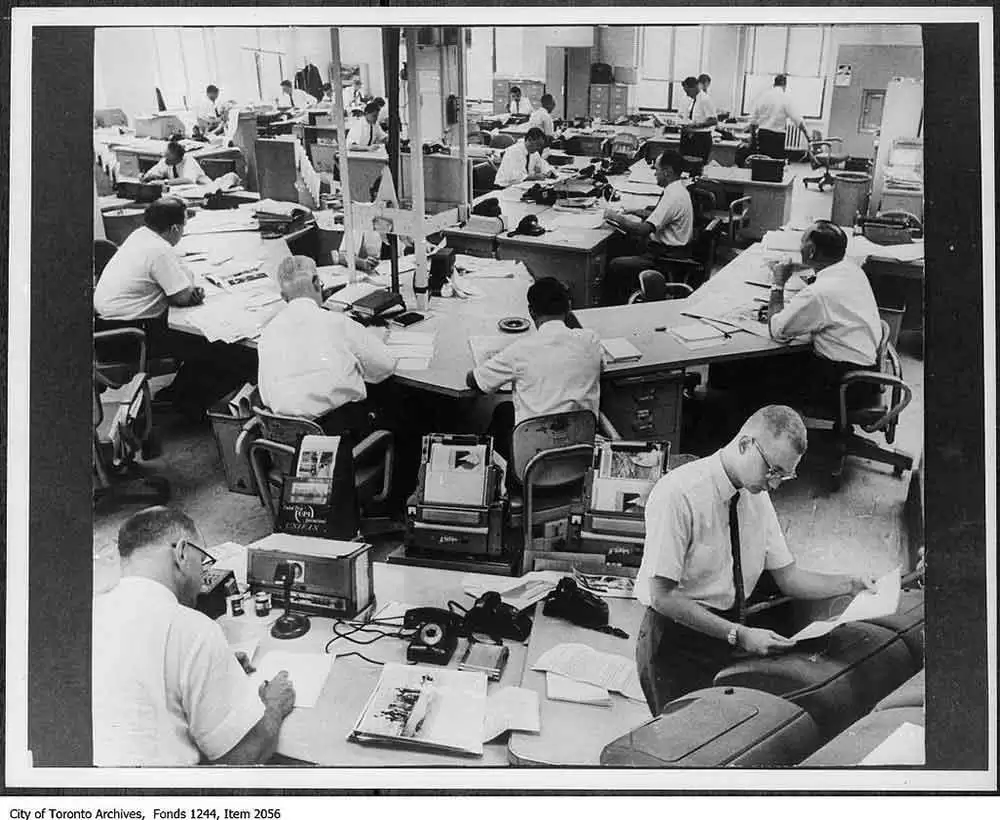
Celiac.com 03/02/2019 - Feedback from readers is increasing. We are therefore establishing a “letters” column where readers can provide commentary on what they have read or what they consider important to the gluten sensitive community for publication in The Journal of Gluten Sensitivity. We will choose some of these comments for publication in the journal.
Rheumatoid Arthritis and Gliadin Antibodies (Author’s name withheld at their request):
Celiac.com Sponsor (A12):
I purchased and read Dangerous Grains over the Christmas break, and I wanted to say thank you for all of your efforts to share information regarding gluten intolerance.
Reading your book made me realize what a classic case I am and it made me so sorry that I wasn’t aware it existed sooner. I’ve been anaemic all my life. I went to a gastroenterologist when I was thirty complaining of severe stomach aches. (I had been eating lots of shredded wheat and drinking orange juice as part of a health kick to try to avoid getting colds that I might pass along to my 3 young children.) That is probably the closest I’ve ever come to actual celiac symptoms, but the doctor’s response was that I was not that young anymore and may need to avoid eating certain foods, especially spicy ones.
I was diagnosed with an underactive thyroid when I was 34. At the time, I asked the doctor if there were any dietary changes that might help, and he told me no. I believed that my thyroid problems were inevitable since my mother also had them. Her whole family has a strong history of allergies, asthma, skin conditions, and diabetes as well as the cancer that killed her and one of her sisters.
About 5 or 6 years later, I tested positive for gliadin antibodies and was sent for an endoscopy, which was negative. I had never heard of celiac disease before that, but fully expected the test to be positive since I thought it might explain the frequent, if not severe, stomach aches I seemed to get. The endoscopy showed no damage to the villi, and when I expressed surprise the gastroenterologist said I did have a little irritation, maybe some mild gastritis, but definitely not celiac disease.
I asked if I should follow the diet anyway, just in case. He said the diet is very difficult and that there is absolutely no reason to follow it if you don’t have celiac disease. I remember feeling uneasy about it, and thinking it was odd that I had antibodies against a specific food but it wasn’t a problem. However, I mistakenly believed that if I had any intolerance to gluten it must obviously be a slight one, and I figured if it really was a problem my digestive symptoms would get worse. They didn’t.
I was diagnosed with rheumatoid arthritis last October, and made an appointment with a rheumatologist. During the 3 weeks I had to wait to get an appointment I spent some time on the Internet trying to understand how I could suddenly have something so awful when I thought I was doing everything I could to take good care of myself. I googled “anti-gliadin rheumatoid arthritis” and was surprised at how many hits I got. The first of the most interesting was a paper by Ron Hoggan saying that there is enough anecdotal evidence that every rheumatoid arthritis patient should try going gluten free. My sister is a nurse who has RA and is on Remicade and Methotrexate, and she was not enthused about the diet idea. However, my symptoms got so bad that I could barely button my clothes and the pain was keeping me up at night. The week before the appointment I decided I had to try something. I found the diet not nearly as difficult as predicted and within a few days the pain was starting to lessen so I could sleep.
The rheumatologist was not enthused about the diet idea, and prescribed some strong pain medication even though I told him I wasn’t taking anything for pain and I wanted to avoid it as much as possible to try to heal my stomach - I never went back. It’s been a little over a year now and although I’m not completely back to normal, I’m close. I’ve been seeing an MD who treats people with vitamins and supplements for the last 6 months.
I plan to get genetic testing done. Assuming that I have the celiac gene, I want to have my children tested. I have a son (healthy, although he struggled through school with symptoms of ADD but I never had him tested because we didn’t want to medicate him) and 3 daughters - the oldest has a long history of stomach aches, the second one has asthma, and the third had elevated ANA and was tested for lupus and juvenile rheumatoid arthritis last year around the time I was diagnosed with RA. Fortunately, her tests came back okay. I told the pediatric rheumatologist that I had been gluten free for a month at that time and was improving, and that if my daughter tested positive, I wanted to treat her with diet rather than medication.
Her response was “why would you ever put that child on a gluten free diet”. I really wanted to ask why she would ever put a child on Methotrexate and immune suppressants, but figured there was no point.
I’m really angry that this information has been available for some time now and I was in the dark for so long - angry at myself for not spending more time doing reading about my health, and at my doctors who were supposed to be experts and handed out useless and misleading information with confidence. They get such respect in our society, and I don’t care how many body parts and diseases they are able to memorize, if they can’t or won’t look at new information and understand the implications, they aren’t much use to us. The problem is convincing others of that.
Thanks for the paper that gave me hope that maybe there was a better way to treat this than immune suppressant (1, 2, 3).
- http://donwiss.com/gluten-free/Hoggan/ra.htm
- https://www.amazon.com/dp/B0090QVTLY
- http://ourgffamily.com/2010/04/nytimes-q-on-gluten-and-gluttony.html/
POST Cereals are Self-Certified as Gluten-Free by Angry Parent in NY (Author’s name withheld at their request):
The news on Dec. 22 was exciting! According to a recent announcement by POST FOODS, their Fruit and Cocoa Pebble cereals are “Certified as Gluten Free”. The press release states, “In response to increased concerns over celiac disease and products containing wheat gluten, the brand went through a rigorous process to achieve Gluten Free status on both Fruity and Cocoa Pebbles products.”
This is great! My son is going to be excited to have Pebbles cereal. As a parent of a sensitive celiac child, I am very careful about the products I feed to him. I trust products that have third party gluten-free certification because I know those products have to meet stricter standards than those set by the FDA. Once in a while, a special treat in the form of a cereal like Pebbles would be a nice treat for my son.
I thought that congratulations were in order for the certifying agency. But when I congratulated the Gluten-Free Certification Organization, I was told they did not work with POST. Something wasn’t right. I could not find out who had certified POST cereals. I am part of a parents group for celiac children and we wanted to thank the organization that made this happen. So we wrote to POST to thank them for certifying their products and to ask who they were working with for their gluten free certification.
Jennifer Brain-Mennes, Director of Media and Public Relations for POST made the following reply: “Post followed a gluten free validation procedure that included certification from all ingredient suppliers, outside laboratory testing of all ingredients, testing the production line, and outside laboratory testing of the finished product. In addition, Post has instituted process controls to ensure there is no cross-contact with gluten containing products. We do not have third party verification symbols on the product boxes.”
I was upset when I saw this response from POST. I felt cheated by this cereal giant. The same thing happened when Betty Crocker launched their gluten-free mixes. It was very clear that General Mills, their parent company, knew the market potential and their press releases made it sound like they cared more about potential profits and little about my family or me. Now POST has joined in, only POST must also have seen reports that celiacs trust gluten-free certification so they used those words in their advertising. I was excited about giving my son Fruity Pebbles, but now I am not so sure I want to risk it. I was convinced POST was thinking about the celiac children until I saw the response from Ms. Brain-Mennes. Now I feel duped and I don’t trust them. POST tried to gain my trust by feeding me the words I want to hear “certified as gluten-free”. Our little group of parents was also confused by this. We heard another parent got a similar letter in response to the certified Pebbles.
He shared the letter he wrote and the response he got from POST:
While I deeply appreciate these steps to make sure that your cereals are gluten free, your use of the word certification is confusing and misleading to consumers with gluten intolerance and celiac disease.
Certification is interpreted by consumers as an indication that an independent third party has reviewed the facility, production procedures and ingredients. You wouldn’t write that a product is certified organic if you didn’t have independent certification. The gluten free certification procedures and standards from an independent group like The Gluten Free Certification Organization run by the Gluten Intolerance Group of North America is clearly detailed on their web site: gfco.org
Although your use of the word certification in your press release should be corrected and withdrawn, I would encourage Post to consider another path - adopting independent certification. To give you an indication of consumers of gluten free products view of independently certified products Vs. manufacturers’ own gluten free claims, I have copied some recent comments from the Gluten Intolerance Group of North America Facebook page. Gluten free consumers are very savvy shoppers who spend many hours every week reading labels and calling food companies to ensure that they are avoiding gluten. As you can see, they recognize and deeply appreciate the value of independent certification. [Gluten Intolerance Group Face Book quotes inserted].
Thanks again for your response. (Eric, NY)
POST RESPONSE:
“Post stands by its statement and had implemented rigorous procedures and testing to insure our Pebbles products are gluten free. Thank you for your inquiry, we value our consumer feedback.”
Clearly POST knows celiacs trust the words “Certified Gluten Free”. Even though they have implemented the processes that should keep their products safe, they have not revealed what their testing standard is. And since the FDA has no definition of gluten free, I don’t know if I can trust this product any more than I can trust others who are jumping at the chance to add gluten-free to their label and make a buck. Gluten Free is everywhere and continues to grow. I have heard that when the big companies are labeling gluten-free, the price of gluten-free food will come down. The way that POST is going about advertising the Pebbles as being certified as gluten free makes me angry. They are lining their pockets at the expense of my trust and possibly my child’s health. For me, this announcement by POST bends the truth quite a lot – to the point where it appears to be deceptive advertising. I don’t think we should support products or companies that use this type of misleading advertising. I wonder if the Federal Trade Commission would agree with me that this is not truth in advertising.








Recommended Comments
There are no comments to display.
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now