Celiac.com 10/02/2014 - Most people have heard about kidney stones, or gall stones, due to calcium build up. Others may know that calcium deposits can affect the heart, and even the brain. However, until now, it was not known that, in certain cases, celiac disease can trigger calcification in the brain.
 Doctors examining a 24-year-old Brazilian man with a history of recurrent headaches revealed a rare condition known as the CEC syndrome, a combination of celiac disease, epilepsy, and cerebral calcification, commonly referred to as ‘brain stones.’
Doctors examining a 24-year-old Brazilian man with a history of recurrent headaches revealed a rare condition known as the CEC syndrome, a combination of celiac disease, epilepsy, and cerebral calcification, commonly referred to as ‘brain stones.’
Celiac.com Sponsor (A12):
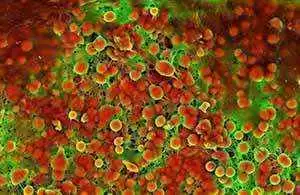
The man had been treated for migraine headaches over a period of 10 years, with little response. Standard blood tests showed a mildly decreased folate level (2.2 ng per milliliter [5.0 nmol per liter]; compared to a reference range of 3.1 to 17.5 ng per milliliter [7.0 to 39.0 nmol per liter]). A computed tomographic scan of his brain showed bilateral occipital calcification, or ‘brain stones.’ Laboratory testing showed normal cerebrospinal fluid and elevated levels of serum IgA antitransglutaminase antibodies (45 U per milliliter).
The man received an endoscopy, and his jejunal-biopsy specimen showed crypt hyperplasia, villous atrophy of the jejunal mucosa, and an increased number of intraepithelial lymphocytes; all classic indications of celiac disease. Doctors started treatment with a gluten-free diet, folic acid supplementation, and carbamazepine, and the patient's symptoms disappeared and his condition improved.
In this case, there was no indication that the man suffered from epilepsy. The likely culprit is folate malabsorption, because cerebral calcification has been seen in other conditions related to folate deficiency, such as treatment with methotrexate, congenital folate malabsorption, and the Sturge–Weber syndrome.
So, physicians treating celiac patients with low folate levels may want to keep an eye out for any indications of cerebral calcification, and to make sure that patients receive appropriate supplemental folate.
Source:
- Open Original Shared Link






Recommended Comments
There are no comments to display.