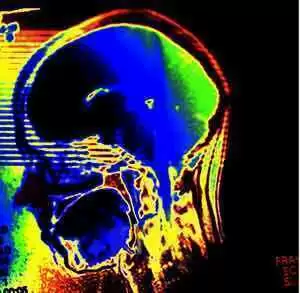
Can going gluten-free boost your brain power? Dr. David Perlmutter, neurologist, and author of Grain Brain, published by Little Brown and Company, thinks there's a good reason why we may want to go gluten-free a try. Dr. Perlmutter gives three basic reasons for people to avoid gluten in their diets:
 1. Avoiding Gluten Reduces Brain Degredation
1. Avoiding Gluten Reduces Brain Degredation
While the majority of individuals suffering from gluten sensitivity experience intestinal discomfort, Perlmutter says an increasing number are experiencing neurological challenges including difficulty staying on task, poor memory function, brain fog and severe headaches that result from inflammation; a common reaction to gluten in those with a sensitivity to the protein. "The brain responds really badly to inflammation," says Perlmutter.
Celiac.com Sponsor (A12):
Another reason for the loss of cognitive function is that some of our brain proteins look similar to gliadin, a protein found in gluten-containing foods, says Perlmutter.
Anti-gliadin antibodies produced by individuals with gluten sensitivity can't tell the difference between these two proteins and eat up the brain proteins that are required for normal cognitive function.
Going gluten-free likely won't make you any smarter, but Perlmutter says it may help protect your cognitive function from weakening.
2. Avoiding Gluten Strengthens the Immune system
Perlmutter says gluten stimulates the cells of the intestine to secrete a protein called zonulin, which regulates the absorbency of the intestine.
The increased production of zonulin erodes the walls of the intestine, allowing various proteins to leave the gut and enter our blood stream.
This poses many challenges to the immune system, weakening our ability to fight off diseases. According to Perlmutter, avoiding gluten, strengthens the immune system.
A healthy immune system is essential for optimal brain function.
3. Avoiding Gluten Improves Brain Fueling
According to Perlmutter, a healthy brain needs generous amounts of healthy fats. Because our brains are 70 percent fat, food loaded with carbs and sugar rob them of the fuel they need to function well.
In place of gluten and carb-laden breakfast food such as a bagel and orange juice, Perlmutter recommends a high-fat breakfast rich in omega 3 fatty acids that protect the brain, including eggs, nuts, seeds or avocado.
The verdict is out as to whether or not people without gluten sensitivity experience the same cognitive decline as those with gluten sensitivity, However, Perlmutter urges anyone experiencing poor cognitive function, chronic headaches or inflammatory illnesses, including joint or abdominal pain, to avoid gluten for few months and see if there is any positive change.
What do you think? Has going gluten-free helped improve your brain function, along with your other celiac symptoms? Share your comments below.
Source:
- Open Original Shared Link










Recommended Comments