
Celiac.com 04/10/2020 - There is a growing epidemic of obesity, type II diabetes, cardiovascular disease, and predictions that 15,000,000 people in the United States alone will have Alzheimer’s Disease by the year 2050.
In 2001, Dr. Richard L. Veech of the NIH, and others, published an article entitled, “Ketone bodies, potential therapeutic uses.”(1) In 2003, George F. Cahill, Jr. and Richard Veech authored, “Ketoacids? Good Medicine?”(2) and in 2004, Richard Veech published a review of the therapeutic implications of ketone bodies.(3) These articles are not found in journals that the average physician would read, much less the lay public. Unless you are researching the topic, it is unlikely that you would ever randomly come across this information.
Celiac.com Sponsor (A12):
My husband Steve, age 58, has had progressive dementia for at least five years. He had an MRI in May 2008 showing a diffuse involutional change of the frontal and parietal lobes and moderate left-sided and severe right-sided amygdala and hippocampal atrophy with no ischemic change, which would support a clinical diagnosis of Alzheimer’s Disease. For non-medical people, this means that he has shrunken areas of the brain. Many days, often for several days in a row, he was in a fog; couldn’t find a spoon or remember how to get water out of the refrigerator. Some days were not so bad; he almost seemed like his former self, happy, with his unique sense of humor, creative, full of ideas. One day I would ask if a certain call came that I was expecting and he would say, “No.” Two days later he would remember the message from so-and-so from a couple of days earlier and what they said. Strange to have no short-term memory and yet the information was filed somewhere in his brain. My gut feeling is that diet has something to do with the fluctuation, but what. I knew that he was locked up in there somewhere, if only there was a key to open up the areas of his brain that he didn’t have access to.
Steve has a BSBA in accounting, and did billing, bookkeeping and accounting for my neonatology practice from home, so that he could stay with our girls. He loved computers and was a fast typist. He could open computers up to repair them and fix practically anything else without ever having instruction. If he did not have a tool to do something he would “invent” it and make a usable prototype. He loved to kayak and made an attachment to keep his kayak moving in a straight line. About five years ago he began to have trouble organizing to do his accounting work. He would procrastinate as much as possible. He made mistakes with the payroll and I began to sit with him to help him get it right. I thought it was just that our practice had gotten more complicated with more employees. He knew that something was wrong and depression set in. We took him to a neurologist about 4 years ago, who did a Mini Mental Status Exam (MMSE,) and Steve scored a 23 out of 30, putting him into the mild range of dementia. On this test, the lower the score is, the worse the dementia. His MRI was reported as normal at that time.
About three years ago, Steve started taking Aricept and two years ago Namenda. We were hopeful that, if we could slow his decline enough, a treatment would come along that would turn things around for him. He was changed over from Aricept to Exelon in August 2007 after losing ten pounds over several weeks. In the past 12 months there was a noticeable change. He can no longer cook for himself, remember to eat a good meal, use a calculator or even perform the simplest addition, however he still keeps busy all day working in the yard or in his garage and he is still in good physical condition. I now do all the cooking for a man who used to cook for his family regularly. I give him the medications because he can’t remember to take them, much less take the right pills. Every night, we hold each other before we go to sleep and I wonder how many more times we will get to do this. It has been a nightmare to watch his decline and feel helpless to do anything but watch it happen. He is fully aware of his dementia, and we talk about it frequently. He is no longer depressed, probably with the help of counseling, Lexipro and Wellbutrin, or maybe worsening of his disease.
I subscribe to various alerts and check the website clinicaltrials.gov periodically to look for drug studies that he may qualify for. Two years ago we tried to get him into a study for a promising anti-inflammatory drug, Flurizan, but he did not qualify because he had a history of depression within the previous two years. Wouldn’t you be depressed if you knew you had Alzheimer’s? In fact, depression may be a symptom or precursor of Alzheimer’s.
Until very recently, I didn’t see anything regarding the potential use of medium chain triglycerides (MCT oil), or ketone bodies (also called ketoacids,) the end product of their metabolism, which may not only treat, but also prevent Alzheimer’s disease. Further, this is a potential treatment for Parkinson’s disease, Huntington’s disease, multiple sclerosis and amyotrophic lateral sclerosis (ALS or Lou Gehrig’s disease), drug resistant epilepsy, brittle type I diabetes, and diabetes type II, where there is insulin resistance. Ketone bodies may help the brain recover after a loss of oxygen in newborns through adults, may help the heart recover after an acute attack, and may shrink cancerous tumors. Children with drug resistant epilepsy sometimes respond to an extremely low carbohydrate ketogenic diet. MCT oil appears to be useful as an aid in weight loss and body builders use it already to improve their lean body mass (MCT oil can be easily purchased on the internet.) Athletes and soldiers could use MCT oil as a source of fuel when the body runs out of carbohydrates, which occurs rather quickly when food is not readily available.
What do these entities have in common? Our cells can use ketone bodies as an alternative fuel when glucose is not available. Brain cells, specifically neurons, are very limited, more limited than other cells, in what kinds of fuel they can use to function and to stay alive. Normally, they require glucose (sugar), but they can also use ketone bodies. Humans do not normally have ketone bodies circulating and available to the brain unless they have been starving for a couple of days or longer, or are consuming a ketogenic (very low carbohydrate) diet, such as Atkins. In Alzheimer’s disease, the neurons in certain areas of the brain are unable to take in glucose (4), (5) due to insulin resistance and slowly die off, a process that appears to happen one or more decades before the symptoms become apparent. If these cells had access to ketone bodies, they could potentially stay alive and continue to function. It appears that persons with Parkinson’s disease, (6) Huntington’s disease, (7) multiple and ALS (9) have a similar defect in utilizing glucose but in different areas of the brain or spinal cord.
MCT oil is digested differently by the body than other fats. Instead of storing all MCTs as fat, the liver converts them directly to ketone bodies, which are then available for use as energy. Oral and intravenous administration of MCT oil produces hyperketonemia, (10) or circulating ketone bodies, which are then available to the brain for energy, in the absence of glucose (19) and even in the presence of glucose. (22) In addition, hyperketonemia results in a substantial (39%) increase in cerebral blood flow, (18) and appears to reduce cognitive dysfunction associated with systemic hypoglycemia in normal humans. (19)
About 2 months ago, we took Steve to the Johnny B. Byrd, Jr. Alzheimer’s Institute at University of South Florida (USF) in Tampa, Florida for an annual evaluation and screening for a vaccine study (Elan). He was fasting for blood work and had an MMSE of 12, much too low to qualify for the vaccine study – a minimum score of 16 was required. We were very disappointed, but were advised that we could come back another time to try again, since he met all of the other criteria.
We made an appointment in mid-May 2008 in St. Petersburg, Florida to screen Steve for an Eli Lilly gamma-secretase inhibitor and made another appointment for Steve to be screened for entry into the Elan study at USF the following day. The evening before the first screening in St. Pete, I researched the two drugs to help us decide which drug to choose, should he qualify for both studies. I came across another drug, Ketasyn, or AC-1202, that was also recruiting healthy older people to test the tolerability of three different formulations. Investigating further, I learned that this treatment brought about significant improvement over a 90-day period in about half of the subjects who had a certain genetic profile (APOE2 or APOE3.) The APOE4 group remained about the same, whereas the controls (people taking the placebo) continued to show decline. The results were even more impressive for people who were already taking certain Alzheimer’s medications. In a pilot study, some people improved on memory testing with the very first dose. Upon doing an internet search for Ketasyn, I found a January 2008 patent application (see freepatentsonline.com) (10) a continuation of a 2000 application, 75 pages long, with a well-written and thorough description of the science of Alzheimer’s disease and description of the “invention,” including these study results and numerous potential formulations in combination with other substances that may enhance its effect.
I learned that the promising “ingredient” in Ketasyn is simply MCT oil, and that a dose of 20 grams (about 20 ml or 4 teaspoons) was used to produce these results. The MCT oil that these researchers used was obtained from Stepan Company and consists of primarily 6 and 8 carbon chains, however they state that MCT of any combination of medium chains (6 to 12 carbon chains are medium chain) would also be effective. Just once in this application, the author mentions that MCT oil is derived from coconut or palm oil (this is incorrect, the author should have stated palm kernel oil.)
I didn’t know at that point that I could easily purchase MCT oil online, so I researched coconut oil and found out that coconut oil is about 60% medium chain fatty acids (MCFA), contains no cholesterol and also contains omega-6 fatty acids and some other short and long chain fatty acids of up to 18 carbon chains. (11) Coconut oil can be found in many health food stores and even some grocery stores. Wal-Mart sells a non-hydrogenated (no transfat) brand of coconut oil in a one-liter size (almost 32 ounce containers) for about $7 in our area of Florida. It can be purchased in quantities as small as a pint and up to five gallons online. It is important to use coconut oil that is non-hydrogenated and contains no transfat. There is a widely held misconception that coconut oil is the “artery clogging oil,” a term coined in the mid-1900’s by the president of Proctor and Gamble, the manufacturer of Crisco and other hydrogenated vegetable oils. The early studies in animals used hydrogenated coconut oil, which we now know produces the notorious trans-fats, and the essential fatty acids were excluded from the diet. (13)
The largest producer of coconut oil is the Philippines, where coconut and its oil are food staples, and it is also produced in India, Thailand and other parts of Southeast Asia, the Caribbean islands and even in south Florida. The Philippines has one of the lowest incidences of cardiovascular disease in the world. Studies have shown that total cholesterol to HDL ratio improves with non-hydrogenated coconut oil. (14, 15, 16, 17) The people in this part of the world also eat fish regularly, providing them with omega-3 fatty acids, which probably contributes as well to the lack of cardiovascular disease. My nurse friends from the Philippines tell me that many of their relatives back home cook everything in coconut oil and have coconut in one form or another at nearly every meal.
I have also learned that after coconut and palm kernel oil, the food that medium chain triglycerides are most concentrated in is human breast milk. (12) It is also found in smaller concentrations in goat and cow’s milk, as well as the butters from these milks. In fact, we used to add MCT oil 20-25 years ago to premature formulas to add calories, and MCT, coconut and palm oils are currently added to premature and full term infant formulas, along with ARA and DHA to mimic breast milk.
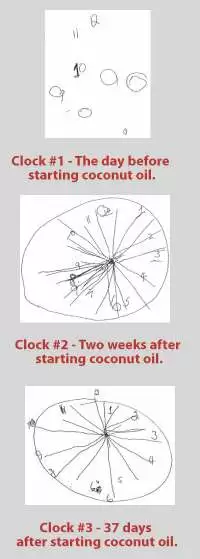 Back to Steve, it was too late to find coconut oil before the first screening. On the way, I reminded him repeatedly that we were in St. Petersburg, in Pinellas County. On the MMSE, he remembered the city but not the county, and he couldn’t remember the season, the month or day of the week, much less the date, even though he had to initial and date numerous pages of consent forms before the MMSE. He had to be reminded on every single page where to initial and what the date was and even how to write out the date. He scored a 14, too low for entry into the study. Dr. Margarita Nunez spent considerable time with us and asked Steve to draw a clock (see clock #1), which she said was a specific test for Alzheimer’s. She took me aside and told me that his “clock” indicated he was leaning more towards severe than moderate AD, a devastating, but not surprising revelation to me, considering that I am his wife of 36 years and now his caretaker.
Back to Steve, it was too late to find coconut oil before the first screening. On the way, I reminded him repeatedly that we were in St. Petersburg, in Pinellas County. On the MMSE, he remembered the city but not the county, and he couldn’t remember the season, the month or day of the week, much less the date, even though he had to initial and date numerous pages of consent forms before the MMSE. He had to be reminded on every single page where to initial and what the date was and even how to write out the date. He scored a 14, too low for entry into the study. Dr. Margarita Nunez spent considerable time with us and asked Steve to draw a clock (see clock #1), which she said was a specific test for Alzheimer’s. She took me aside and told me that his “clock” indicated he was leaning more towards severe than moderate AD, a devastating, but not surprising revelation to me, considering that I am his wife of 36 years and now his caretaker.
Thinking, what have we got to lose, we stopped at a health food store on the way home and picked up a quart of 100% “virgin” coconut oil. I calculated that in order to provide 20 gm of MCT, he would need to take 35 grams or just over two tablespoons (about 35 ml or 7 level teaspoons) of coconut oil. The following morning, around 9 A.M., I made oatmeal for breakfast and stirred two tablespoons, plus more for “good luck,” into his portion. I had some as well, since I cannot expect him to eat something that I won’t eat.
On the way to the 1:00 P.M. screening, I tried to prepare Steve by asking him the season, the month, the day of the week, reminding him that we were going to Tampa, in Hillsborough county. He couldn’t remember the word “spring,” came up with April instead of May for the month every time I asked him and he couldn’t remember it was Wednesday. During the hour-long drive, we went through these facts at least 10 times, but he still couldn’t remember. Shortly after we arrived he was whisked away for the test, about 4 ½ hours after consuming the coconut oil. When he returned, he was very unhappy about his performance. Laura, the research coordinator, returned shortly thereafter and began to take his vital signs and blood pressure, and, suspecting that we were continuing with the screening process, I asked her if she could share his score with us. She said, “Didn’t he tell you? He scored an 18!” more than he needed to qualify for the vaccine study. He remembered it was spring, it was May, it was Wednesday, that he was in Tampa, in Hillsborough County and that we were at the Byrd Institute, all points that he missed on the previous attempt at USF. As a result of the screening, we learned that he is positive for APOE4, but do not know at this time if he has one or two copies.
According to the Ketasyn studies, Steve should not have improved, but rather he should have stayed about the same. Since then he has retested for the Eli Lilly study drug, now available closer to home and scored an MMSE of 17 - he even remembered the date of July 2, 2008 this time. We have decided, after looking at the potential side effects of the vaccine for APOE4+ people, to go with the Eli Lilly drug.
At the time of this writing it has been 60 days since he started taking coconut oil (May 21, 2008.) He walks into the kitchen every morning alert and happy, talkative, making jokes. His gait is still a little weird. His tremor is no longer very noticeable. He is able to concentrate on things that he wants to do around the house and in the yard and stay on task, whereas before coconut oil he was easily distractible and rarely accomplished anything unless I supervised him directly, a source of some contention between us!
After about two weeks, and again at 37 days, after starting the coconut oil, I asked him to draw a clock (see Clocks #2 and #3.) There is an obvious marked improvement. I promise that I did not help him. He tells me that he could not even picture a clock at the St. Pete screening, but with the last two attempts, he was very concerned that the 6 was opposite the 12 and the 9 opposite the 3 on the face of the clock. He drew “spokes” to help them line up. I did not ask him to try to put in a time, the next part of that test.
Steve has not been able to type for at least two years, but he feels that he can picture the position of the letters on the keyboard. At this point he is afraid to sit down and try to type, worried that he will be discouraged if it doesn’t come back right away. We are considering trying occupational therapy to see if he can relearn some of the skills he has lost. I cannot explain why he has improved, except that perhaps the 10 and 12 carbon chains are important, or the APOE4 people in the Ketasyn studies were not taking omega-3 fatty acids. We eat salmon at least twice a week and take fish oil supplements twice a day and have for at least the past two years.
I have been researching on the internet everything I can find about coconut oil, MCT oil, fatty acids, ketone bodies, fatty acid composition of breast milk, ketones and various disease states. When I researched ketone bodies, I came across the name of Dr. Richard Veech of the National Institutes of Health. I contacted him to ask questions about all of this and he very kindly spoke with me and emailed me articles he had written on the subject. I have had numerous questions and ideas, and he has continued to provide me with answers and more papers to read. I am thinking not only about people with neurodegenerative diseases like my husband, but also the sick and premature newborns that I take care of, and potential uses for those at both ends of the spectrum of life and everyone in between. I wonder about autism and whether something very important is missing in infant formulas and in the diets of women who are breastfeeding. (23)
Beta-hydroxybutyrate is the primary ketone body that is the end product of fatty acid metabolism and appears to protect neurons when glucose is not available. (20) Dr. Veech can make an ester form of beta-hydroxybutyrate in his lab from MCT oil that can be taken orally and converted to energy by neurons and other cells. Potentially, higher levels of ketone bodies could be obtained by ingesting beta-hydroxybutyrate directly. He has done studies on animals, but needs to produce this in quantity to be able to do human studies. He could start testing this year, if only he had the funding. He needs $15 million to build a plant to produce his beta-hydroxybutyrate. That is a lot of money, but not so much if you consider that it is $1.00 for every person that is expected to have Alzheimer’s disease by the year 2050.
We visited Cincinnati at the end of June and all of my family and Steve’s family noticed a very significant difference in how he interacted with them socially compared to a year ago. Instead of looking lost, he was involved and interested in what they had to say. He recognized relatives (brothers-in-law, nieces and nephews) by name immediately that were unfamiliar to him a year ago. His facial expression was more animated. He participated actively in conversations, understood jokes immediately and even came up with his own humorous comments. He still had difficulty finding some words, but he was talking in sentences and even stringing sentences together. In the morning he would come to the kitchen and ask me to walk the “big hill” with him before breakfast to get some exercise. He is a very different person than he was a year ago and perhaps even two or three years ago. He has serious atrophy of his brain and will never be “normal,” but for now we are very pleased with where he is at and, should coconut oil stop or slow down the progress of his disease, it will be worth every drop that he takes.
My sister Lois told a lady she works with about the coconut oil and Steve’s response to it. Her father began to give this to her mother, who has Alzheimer’s and she has had a similar response, with more alertness, conversation and sense of humor.
On July 9, 2008, Steve had blood samples drawn at various times before and following breakfast and dinner. He received 35 ml of coconut oil at each of those meals. He did not receive any other coconut oil or other coconut products during the rest of that day. Normally, he receives more coconut oil than that on the average day. Steve’s ketone body levels began to increase after breakfast over 3 hours, but at relatively low levels, dropped again before dinner and were steadily rising about 3 hours after dinner. We do not know when his levels peaked because we did not draw any further levels thereafter. Dr. Veech stated that it is surprising that Steve would improve with these relatively low levels of ketones. This study reaffirms his belief that it is necessary to go forward with the production and testing of his ketone body b-hydroxy butyrate esters, since considerably higher levels of ketone bodies, timed and controlled could be achieved, and more ketones would be available for the neurons to use, and therefore greater improvement could be expected.
It is urgent that funding become available to move forward for the sake of the millions who currently suffer, and will in the future suffer, from Alzheimer’s disease, Parkinson’s disease, Huntington’s chorea, multiple sclerosis, ALS, type I and type II diabetes, as well as any number of other conditions that involve a defect in transport of glucose into neurons and other cells.
Until Dr. Veech’s beta-hydroxybutyrate is tested and available for use, a simple dietary change to coconut oil could make a difference for people who believe they are at risk and for those who already have one of these diseases.
To duplicate the dose of MCT taken in the Ketasyn study, about 7 level teaspoons should be taken at one time, once a day, which should circulate ketone bodies for about 24 hours. I do not know if it is necessary to take this much at one time or if the dosage could be spread out over the course of the day. Studies obviously need to be done to determine this. We actually give this amount to Steve at least twice a day to make sure that there are no periods without ketone bodies circulating. Many days he receives at least 50% more than this. The amounts we are taking would not be excessive in areas of the world where coconut is a staple. If a person can tolerate more, or can work up to tolerating more, it may be a good idea to do so. As an alternative, one could take 4 teaspoons of MCT oil once or twice a day, or more often as tolerated.
Some people may experience a sense of “fullness” or even have diarrhea after taking this much to start, but this problem can be reduced by starting with one or two teaspoons and increasing over a week or so to the full amount. We put it in oatmeal, combine it with salad dressings, use it to cook with, and put it on anything that one would normally put butter on, such as potatoes, sweet potatoes, rice, pasta or noodles. Coconut ice cream can be purchased at Asian stores, contains coconut oil and is the most pleasant way I can think of to make ketone bodies. Likewise, coconut milk is a combination of coconut oil and coconut water and can be found in the Asian and condensed milk sections of many grocery stores. It is a pleasant substitute for milk, and can be added instead of milk, for example, to make scrambled eggs, French toast and mashed potatoes. You can figure out portion sizes of various combinations of foods containing coconut and coconut oil equivalent to at least 35 grams of fat from coconut oil.
If you are using any type of hydrogenated vegetable oil or any oil with transfat, do not use any more and get rid of it! Extra virgin olive oil, butter and other natural, non-hydrogenated oils are okay to use along with the coconut oil. It is possible to use coconut oil in place of all other oils, however, since it contains no omega-3 fatty acids, it is very important to eat salmon twice a week or get enough omega-3 fatty acid from other rich sources such as fish oil capsules, flax meal, flax oil (not for cooking) or walnuts.
It is inconceivable that a potential dietary prevention and cure for Alzheimer’s disease, and other neurodegenerative diseases, has been out there for so many years, and yet has gone unnoticed. It is very likely that these diseases are becoming more prevalent due our current diet. The American diet has changed drastically from what it was before the 1950’s, when our parents and grandparents used lard and coconut oil to cook. Cardiovascular disease was rare at the beginning of the 20th century, and has skyrocketed, along with other devastating diseases, such as Alzheimer’s, diabetes type II, obesity, since mass produced hydrogenated vegetable oils containing trans fats were introduced into our diets and replaced these other natural fats. Sadly, the incidences of cardiovascular and other serious diseases are becoming more and more common among people in other areas of the world who have changed over from their indigenous foods to the “western” diet.
I plan to tell everyone I can and get this information to persons in positions to investigate this with the hope that Dr. Veech and other MCT oil and ketone body researchers get the funding they need. Feel free to make copies and pass this write-up on.
If you have a loved one or a patient with Alzheimer’s or one of these other degenerative neurologic diseases, consider trying coconut oil. Dr. Veech suggests that, if possible, a videotape of the person before starting and at various points after starting the coconut oil would be very useful to document change. He suggests including segments of the persons face, speech and gait (walking). He also advises to have ketone bodies
measured. What have you got to lose?
References:
- “Ketone bodies, potential therapeutic uses,” RL Veech, B Chance, Y Kashiwaya, HA Lardy, GC Cahill, Jr., IUBMB Life, 2001, Vol. 51 No.4, 241-247
- “Ketoacids? Good Medicine?” George F. Cahill, Jr., Richard L. Veech, Transactions of the American Clinical and Climatological Association, Vol. 114, 2003.
- “The therapaeutic implications of ketone bodies: the effects of ketone bodies in pathological conditions: ketosis, ketogenic diet, redox states, insulin resistance, and mitochondrial metabolism,” Richard L. Veech, Prostaglandins, Leukotrienes and Essential Fatty Acids, 70 (2004) 309-319.
- "Diminished glucose transport and phosphorylation in Alzheimer’s Disease determined by dynamic FDG-PET,” M Piert, et.al., The Journal of Nuclear Medicine, Vol.37 No.2, February 1996, 201-208.
- “Glucose metabolism in early onset versus late onset Alzheimer’s Disease: an SPM analysis of 120 patients,” EJ Kim, et. al., Brain, 2005, Vol. 128, 1790-1801.
- “Cerebral glucose metabolism in Parkinson’s disease with and without dementia,” RF Peppard, et.al., Archives of Neurology, Vol. 49 No.12, December 1992.
- “Cortical and subcortical glucose consumption measured by PET in patients with Huntington’s disease,” Brain, October 1990, Vol 113, part 5, 1405-23.
- “Reduced glucose metabolism in the frontal cortex and basal ganglia of multiple sclerosis patients with fatigue: a 18F-fluorodeoxyglucose positron emission tomography study,” U Roelcke, et. al., Neurology, 1997, Vol. 48, Issue 6, 1566-1571.
- “ALS-linked Cu/Zn-SOD mutation impairs cerebral synaptic glucose and glutamate transport and exacerbates ischemic brain injury,” Z Guo, et. al., Journal of Cerebral Blood Flow Metabolism, March 2000, Vol. 20 No. 3, 463-8.
- “Combinations of medium chain triglycerides and therapeutic agents for the treatment and prevention of Alzheimer’s disease and other diseases resulting from reduced neuronal metabolism,” United States Patent 20080009467, Inventor Samuel T. Henderson, Accera, Inc., Broomfield, Colorado (Ketasyn).
- Nutrient analysis of coconut oil (vegetable), NDB No: 04047 – www.nal.usda.gov/fnic/foodcomp .
- “Lipids in (human) milk and the first steps in their digestion,” M Hamosh, et. al., Pediatrics, 1985, Vol. 75, 146-150.
- “Nutritional factors and serum lipid levels,” EH Ahrens, American Journal of Medicine, 1957, vol. 23, 928 (used hydrogenated coconut oil).
- “Trans fatty acids and coronary artery disease,” NEJM, 1999, Vol. 340, 1994-1998.
- “Effect of mixed fat formula feeding on serum cholesterol level in man,” SA Hashim, American Journal of Clinical Nutrition, 1959, Vol. 7, 30-34.
- “Modified-fat dietary management of the young male with coronary disease: a five-year report,” JL Bierenbaum, JAMA, 1967, Vol. 202, 1119-1123.
- “Cholesterol, coconuts and diet in Polynesian atolls-a natural experiment; the Pukapuka and Toklau island studies,” IA Prior, American Journal of Clinical Nutrition, 1981, Vol. 34, 1552-1561.
- “Changes in cerebral blood flow and carbohydrate metabolism during acute hyperketonemia,” S.G. Hasselbalch, et.al, Am J Physiol, 1996, Vol. 270, E746-51.
- “Effect of hyperketonemia and hyperlacticacidemia on symptoms, cognitive dysfunction, and counterregulatory hormone responses during hypoglycemia in normal humans,” T. Veneman, et. al., Diabetes 43:1311-7 (1994).
- “D-b-Hydroxybutyrate protects neurons in models of Alzheimer’s and Parkinson’s disease,” Y Kashiwaya, et. al. including RL Veech, PNAS, May 9, 2000, Vol. 97 No. 10, 5440-5444.
- “High carbohydrate diets and Alzheimer’s disease,” Samuel T. Henderson, Medical Hypotheses, 2004, Vol 62, 689-700 (Another article of interest).
- “Effects of b-Hydroxybutyrate on cognition in memory-impaired adults,” MA Reger, ST Henderson, et. al., Neurobiology of Aging, 2004, Vol. 25, 311-314.
- “Breastfeeding, infant formula supplementation, and Autistic Disorder: the results of a parent survey,” ST Schultz, et. al., International Breastfeeding Journal, 2006, Vol. 1 No. 16.
Other Important Resources
- “Ketones: Metabolism’s Ugly Duckling,” TB VanItallie, TH Nufert, Nutrition Reviews, Vol 61, No 10, 327-341.
- • “Fuel Metabolism in Starvation,” GF Cahill, Jr., Annual Reviews in Nutrition, 2006, 26:1-22. “Ketone Bodies as a Therapeutic for Alzheimer’s Disease,” ST Henderson, Journal of the American Society for Experimental NeuroTherapeutics, Vol 5, 470-480, July 2008.









Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now