-
Welcome to Celiac.com!
You have found your celiac tribe! Join us and ask questions in our forum, share your story, and connect with others.
-
Celiac.com Sponsor (A1):
Celiac.com Sponsor (A1-M):
-
Get Celiac.com Updates:Support Celiac.com!
Search the Community
Showing results for tags 'blood'.
-
Celiac.com 04/22/2023 - Celiac disease is an autoimmune disorder that may occur in genetically susceptible individuals. It is initiated by ingestion of gluten present in cereals, primarily wheat and to a much lesser extent other cereal proteins such as prolamines of barley and rye. Celiac disease is characterized by malabsorption resulting from inflammatory injury to the small intestinal mucosa. The classical symptoms of celiac disease include diarrhea, weight loss and malnutrition, however, only a small percentage of patients with celiac disease present with classical symptoms. Such patients represent the tip of the iceberg of gluten sensitivity. Many patients with celiac disease may present with short stature, iron and folate deficiency, anemia, bone loss, aphthous stomatitis, arthralgia, and dental enamel defects. Because of the varying and mild clinical presentations, celiac disease is often diagnosed when the patient has grown to adulthood rather than as a child. Adults may present with iron deficiency, anemia, macrocytic anemia and hypocalcemia. /* DivTable.com */ .divTable{ display: table; width: 100%; } .divTableRow { display: table-row; } .divTableHeading { background-color: #EEE; display: table-header-group; } .divTableCell, .divTableHead { border: 1px solid #999999; display: table-cell; padding: 3px 10px; } .divTableHeading { background-color: #EEE; display: table-header-group; font-weight: bold; } .divTableFoot { background-color: #EEE; display: table-footer-group; font-weight: bold; } .divTableBody { display: table-row-group; } Clinical Presentations of Celiac Disease Classical Features Atypical Chronic Diarrhea Iron-deficiency anemia Failure to thrive Dental enamel defecs Abdominal distension Short stature Osteoporosis/osteopenia Coexistence with other autoimmune disorders Diagnosis based solely on clinical criteria can be misleading and may lead to improper diagnosis and treatment as a result of the variety of clinical presentations often seen in other conditions. Problems with diagnosis has a serious impact on the patient. Delays in diagnosis commonly extend 10-13 years from the first presentation of clinical symptoms, leaving the patient subject to chronic symptoms while searching for proper diagnosis. Failure to diagnose this condition in the short term may predispose an individual to long term complications such as splenic atrophy and intestinal lymphoma. On the other hand, attempts to diagnosis a patient based primarily on clinical criteria may unnecessarily place the individuals on life long gluten-free diet as several transient conditions may mimic celiac disease clinically. /* DivTable.com */ .divTable{ display: table; width: 100%; } .divTableRow { display: table-row; } .divTableHeading { background-color: #EEE; display: table-header-group; } .divTableCell, .divTableHead { border: 1px solid #999999; display: table-cell; padding: 3px 10px; } .divTableHeading { background-color: #EEE; display: table-header-group; font-weight: bold; } .divTableFoot { background-color: #EEE; display: table-footer-group; font-weight: bold; } .divTableBody { display: table-row-group; } Cancer Morbidity on Normal, Reduced-Gluten and Gluten-Free Diet in Celiac Disease Diet Group Number Observed Malignancies Expected Malignancies Observed/ Expected Excess Morbidity Rate Normal 46 7 0.19 36.8 10.7 Reduced Gluten 56 5 0.12 41.7 5.0 Gluten-free 108 3 0.46 6.5 1.2 (Howelle PD, Is Coeliac Disease a Pre-Malignant Condition? Gastrointestinal Immunology and Gluten-Sensitive Disease, 1994. p.185) The true prevalence of celiac disease is difficult to ascertain. However, with the advent of serum antibody methods, incidences as high as one in 300 have been described in the general population, both in Western Europe and in the U.S. celiac disease is prevalent worldwide, but may be rare in individuals of Chinese and Japanese descent. /* DivTable.com */ .divTable{ display: table; width: 100%; } .divTableRow { display: table-row; } .divTableHeading { background-color: #EEE; display: table-header-group; } .divTableCell, .divTableHead { border: 1px solid #999999; display: table-cell; padding: 3px 10px; } .divTableHeading { background-color: #EEE; display: table-header-group; font-weight: bold; } .divTableFoot { background-color: #EEE; display: table-footer-group; font-weight: bold; } .divTableBody { display: table-row-group; } Prevalence of Celiac Disease Country Prevalence based upon Clinical Prevalence based upon Laboratory Finland 1:1000 1:330 Italy 1:1000 1:184 Germany 1:2300 1:500 Netherlands 1:4500 1:250 Denmark 1:10,000 1:330 USA 1:10,000 1:250 Guandalini S & Gupta P Clin appl Immun Rev 2:293-305, 2002 Historically, the diagnosis of celiac disease was based primarily on histological studies of the Jejunal biopsy characterized by villous atrophy, crypt hyperplasia, and lymphocytic and plasma cell infiltrate in the lamina propria. Histological examination of the small intestinal biopsy remains the gold standard for diagnosing celiac disease, but has its limitations. Many patients with celiac disease are small children and histological studies may be viewed by many, especially a child’s parents, to be a great discomfort. There may also be problems with accuracy. Occasionally, a biopsy with abnormally high density of intraepithelial lymphocytes with a normal villous architecture may be reported as normal. It has also been reported that some patients with latent or even active celiac disease show normal histopathology (Gastroenterlogy 104:1263-72, 1993). Celiac disease might also be confused with other disorders when diagnosed histologically. Parasitic infections (giardia lamblia) and malabsorption syndrome, for example, may mimic celiac disease histology. As these limitations have been recognized, serum antibody tests have gained acceptance in screening for celiac disease and in follow-up of patients with celiac disease to determine their compliance to a gluten-free diet. The various serological tests employed in the work-up of patients suspected to have celiac disease include anti-gliadin antibody (AGA), anti-endomysial antibody (EMA), anti-reticulin antibody (ARA) and anti-tissue transglutaminase (tTG) antibody tests. Antibodies to gliadin and tTG are detected by ELISA, whereas endomysium and reticulin antibodies are detected by indirect immunofluorescence. Of the serum antibody tests, EMA and tTG antibody primarily detects antibodies of IgA immunoglobulin isotype, whereas the AGA test detects both IgG and IgA isotypes. No IgM class antibodies to these antigens are detected in patients with celiac disease, hence there is no need to test for IgM class antibodies in the work-up of patients with celiac disease. Of these tests, AGA was the first to be described in the literature and has been evaluated most extensively. AGA of IgG are more sensitive but less specific then IgA-AGA. The major utility of IgGAGA is in celiac disease patients who are IgA deficient. In a study conducted recently in our laboratory, all of the 15 IgA-deficient celiac disease patients were found positive for IgG-AGA and negative for IgA-AGA and other autoantibodies (Celiac Disease and IgA deficiency: How effective are the serological methods of diagnosis? Clinical diagnostic lab Immunology 9:1295-1300, 2002). EMA and ARA are very specific indicators of celiac disease. These assays are immuno-histochemical methods and require experience in reading immunofluorescence reactions. Some investigators suggest that they are less sensitive. However, in all the studies conducted since our laboratory first described EMA back in 1983, we find the EMA assay to be 100% specific and sensitive for celiac disease. Other investigators may find EMA to be less sensitive due to the selection of the substrate, fixation of tissue sections, specificity of conjugate employed or serum screening dilution. Internally, we find that testing for EMA at dilutions of 1:2.5 or 1:5 yield 5% of patients positive for EMA yet negative at 1:10 or 1: 20. It could be that some of the investigators who have reported low sensitivity might be screening the patients at high serum dilutions. Since the identification of tTG as the endomyisal antigen, ELISA methods have been described for detecting antibodies in the sera of patients with celiac disease. The advantage of the anti-tTG antibody assay is that it is an automatable assay that is less subjective than EMA and it is more sensitive and specific than AGA. For these reasons, many laboratories have opted to use the tTG antibody method as the screening method. In these laboratories, it may be the only assay used for detection of celiac disease cases. In the majority of studies of the tTG antibody method, the specificity and sensitivity were found to be between 90-95%. Table 4 on page 15 summarizes the specificity of the AGA, EMA and tTG antibody methods most commonly employed by laboratories performing tests for celiac disease. /* DivTable.com */ .divTable{ display: table; width: 100%; } .divTableRow { display: table-row; } .divTableHeading { background-color: #EEE; display: table-header-group; } .divTableCell, .divTableHead { border: 1px solid #999999; display: table-cell; padding: 3px 10px; } .divTableHeading { background-color: #EEE; display: table-header-group; font-weight: bold; } .divTableFoot { background-color: #EEE; display: table-footer-group; font-weight: bold; } .divTableBody { display: table-row-group; } Diagnostic Specificity of Serological Markers for Celiac Disease Assay Specificity Sensitivity Anti-gliadin Antibody IgG 78% 88% Anti-gliadin Antibody IgA 86% 52% Anti-endomysial Antibody 100% 100% Anti-tissue transglutaminase 98% 90-95% If the prevalence of undiagnosed celiac disease is 4.8 per thousand as reported by Lagerqvist et al (J Intern Med 250:241-48, 2001) then of all the serological methods, EMA is the only method that provides 100% positive and negative predictive value for celiac disease. This raises the question of the optimum method of screening for celiac disease. The answer will vary according to the likelihood of celiac disease in the population studied and upon the experience of the laboratory performing the test. Some investigators may use the AGA or tTG antibody methods for screening and, if positive, confirm using the EMA test. We recommend this approach as it also helps to identify all celiac disease patients, whether IgA-deficient or not. Celiac disease patients are prescribed a gluten free diet for life. Serological tests are useful in monitoring a patient’s response and adherence to the gluten free diet. The levels of the various antibodies (AGA, EMA, ARA and tTG) decrease and eventually disappear in the majority of the patients on a complete gluten free diet. Similarly, these antibodies either appear or rise in level when the patient is on a gluten containing diet. Serological methods, therefore, play a significant role in both diagnosis and follow-up of celiac disease patients. Celiac disease has been associated with many other autoimmune disorders such as type 1 diabetes, thyroid autoimmunity and other autoimmune disorders. Approximately five percent of patients with type 1 diabetes have celiac disease. Similarly, approximately the same percentage of patients with celiac disease have type 1 diabetes. It has been proposed that early detection of celiac disease may be beneficial in such cases as it is believed that adherence to a gluten-free diet may delay the onset of diabetes. If true, this further emphasizes the utility of and need for serum antibody tests in the screening of population genetically susceptible for celiac disease. In conclusion, clinical symptoms of celiac disease are variable and often mild, resulting in significant delays in diagnosis. The use of serological tests has improved the ease of detection, monitoring, and hence— the continuing care of celiac disease patients.
- 9 comments
-
- blood
- blood test
-
(and 6 more)
Tagged with:
-

Interpretation of Celiac Disease Blood Test Results
Scott Adams posted an article in Diagnosis, Testing & Treatment
The following detailed explanation of serological tests for celiac disease was written by Tom Ryan, Technical Service Specialist, INOVA Diagnostics, Inc. There has been a lot of discussion about serological testing for celiac disease recently, specifically regarding tTG (tissue Transglutaminase) testing. I will try to answer some of the many questions that have appeared on this list about all of the tests. First, and this applies to any of the blood tests, you must currently be on a gluten containing diet for the tests to be accurate. Antibodies are produced by the immune system in response to substances that the body perceives as threatening. The immune response that your body produces is its response to being exposed to gluten in the diet and its subsequent effect on the intestinal mucosa. If there is no gluten in the diet, then there is no response that we can measure. A brief change in diet will not have a noticeable effect. If you have been gluten free for a week or so, it will not make any great difference. The response might be marginally less but the difference is insignificant because the body has not had time to respond to the change. Conversely, if you have been gluten free for a protracted period of time and decide to be tested, a brief challenge of a couple of weeks is not enough to elicit a response and get an accurate test. There are several steps that take place to generate an immune response and it takes time both for the positive reaction when gluten is present and to clear the antibodies when gluten is eliminated. There has been a great deal of discussion about how much and how long a challenge should be and there is no consensus. Talk with your Doctor. My personal feeling is that the minimum is 2 slices of bread per day for 6 weeks to get an accurate test but I would not try to second-guess the Doctor. There are basically four tests that can be performed to aid in diagnosing celiac disease. Notice that I say they will aid in diagnosing celiac disease. Immunology is fairly accurate but it is far from being an exact science. All of the lab tests, regardless of the type or source, are presented as aids to diagnosis. They should not be used alone as a basis for diagnosis but rather are intended to be considered in conjunction with the physical examination of the patient as well as the reported symptoms, etc. by a trained physician. There has been a great deal of confusion about what the tests are and I hope to alleviate some of the misunderstandings. There are many terms that we hear. tTG, IgA, IgG, ELISA, etc. What are all of these? Some contributors to the list make reference to the IgA or IgG test or to the ELISA test. These labels are incomplete for our purposes and could be referring to any number of different tests. We all have, within our bodies, a family of closely related although not identical proteins which are capable of acting as antibodies. These are collectively referred to as immunoglobulins. Five major types of immunoglobulins are normally present in the human adult. They are IgG, IgA, IgM, IgE and IgD. Each of these is a shorthand way of writing immunoglobulin gamma G (or A or M, etc.) and they each perform a different function in our systems. IgG is the principal immunoglobulin in human serum. It is important in providing immunity in a developing fetus because it will pass across the placental barrier. IgA is the principal immunoglobulin in secretions from respiratory and intestinal mucosa. IgE is a gamma globulin produced by cells lining the intestinal and respiratory tracts. It produces the antibodies associated with most hypersensitivity (allergic) responses. It is associated with asthma, hay fever, etc. IgM is a globulin formed in almost every immune response in the early part of the reaction. IgD is a rare protein present in normal sera in a tiny amount. These designations refer to the type of protein that is carrying the antibody in question. Both IgG and IgA subtypes of anti-gliadin antibody are produced, hence we refer to them as IgG gliadin or IgA gliadin. Collectively they are anti-gliadin antibodies. Anti-Gliadin Antibodies: Both IgA and IgG anti-gliadin antibodies (AGA) are detected in sera of patients with gluten sensitive enteropathy (celiac disease). IgG anti-gliadin antibodies are more sensitive but are less specific markers for disease compared with IgA class antibodies. IgA anti-gliadin antibodies are less sensitive but are more specific. In clinical trials, the IgA antibodies have a specificity of 97% but the sensitivity is only 71%. That means that, if a patient is IgA positive, there is a 97% probability that they have celiac disease. Conversely, if the patient is IgA negative, there is only a 71% probability that the patient is truly negative for celiac disease. Therefore, a positive result is a strong indication that the patient has the disease but a negative result does not necessarily mean that they don not have it. False positive results are rather uncommon but false negative results can occur. On the other hand, the IgG anti-gliadin antibodies are 91% specific and have an 87% sensitivity. This means that they will show positive results more readily but there is not as strong a correlation with celiac disease. It is less specific. Patients with other conditions but not afflicted with celiac disease will occasionally show positive results. IgG anti-gliadin antibodies are detectable in approximately 21% of patients with other gastrointestinal disorders. This test might yield false positive results but is less likely to yield false negative results. A sensitive testing protocol includes testing for both IgA and IgG anti-gliadin antibodies since a significant portion of celiac patients (approx. 2-5%) are IgA deficient. This combined IgA and IgG anti-gliadin antibody assay has an overall sensitivity of 95% with a specificity of 90%. The type of test used to detect the anti-gliadin antibodies is called an ELISA. This is an acronym and it stands for Enzyme Linked Immuno-Sorbent Assay. ELISA is not a test in itself. It is a method of testing and it is a relatively simple test to perform. It involves putting a measured amount of diluted patient serum into the wells of a specially constructed and prepared plate and incubating it for a period of time with various chemicals. The end result is a color change, the intensity of which is dependent upon the concentration of anti-gliadin antibody (or other protein being measured) in the patient serum. The ability of this colored solution to absorb light at a particular wavelength can be measured on a laboratory instrument and mathematically compared with solutions that contain a known amount of anti-gliadin antibody to arrive at a number for the amount of antibody present. The sample can then be classified as negative, (0-20 units); weak positive, (21-30 units); or moderate to strong positive if greater than 30 units. The purpose of testing for anti-gliadin antibodies includes, in addition to diagnosis of gluten sensitive enteropathy, monitoring for compliance to a gluten free diet. IgA gliadin antibodies increase rapidly in response to gluten in the diet and decrease rapidly when gluten is absent from the diet. The IgA anti-gliadin antibodies can totally disappear in 2-6 months on a gluten free diet, so they are useful as a diet control. By contrast, IgG anti-gliadin antibodies need a long time, sometimes more than a year, to become negative. The reverse is also true. That is, a patient with celiac disease who has been on a gluten free diet and tests negative for IgA anti-gliadin antibodies, will show a rapid increase in antibody production when challenged by gluten in the diet. Approximately 90% of challenged patients will yield a positive IgA anti-gliadin result within 14-35 days after being challenged. The IgG antibodies are somewhat slower. Endomysial Antibodies: IgA class anti-endomysial antibodies (AEA) are very specific, occurring only in celiac disease and DH. These antibodies are found in approximately 80% of patients with DH and in essentially 100% of patients with active celiac disease. IgA endomysial antibodies are more sensitive and specific than gliadin antibodies for diagnosis of celiac disease. Antibody titers (dilutions) are found to parallel morphological changes in the jejunum and can also be used to reflect compliance with gluten-free diets. Titers decrease or become negative in patients on gluten free diets and reappear upon gluten challenge. The test for anti-endomysial antibodies is more subjective and more complicated for the lab to perform than the anti-gliadin assays. It involves serially diluting some of the patients serum, that is, diluting it by ½ then ¼, 1/8, 1/16, etc. and putting these dilutions on a glass slide that has some sort of tissue affixed to it. The slide is then processed with various solutions and examined under a fluorescent microscope to determine if any of that serum binds to any of the proteins in the tissue. If so, then that patient is confirmed as having antibodies to that particular protein. This method of testing is called an IFA or sometimes IIFA. It stands for Indirect Immuno-Fluorescent Assay. The selection of which tissue slide to use is determined by what specific protein, hence which antibody, you are specifically looking for. Endomysial antibodies react with the endomysium, which is a sheath of reticular fibrils that surround each muscle fiber. Therefore, to detect endomysial antibodies, you would want to use a tissue substrate that contains a lot of muscle tissue. The substrate used most often for this assay is distal sections of the esophagus. These are very thinly sliced and fixed to the slide. They contain muscle fibers and not much else so there is a lot of endomysium available to react with the anti-endomysial antibodies. Reading this test involves viewing the reacted slides with a fluorescent microscope to make the determination. This requires a highly skilled and trained eye and, of necessity, is somewhat subjective. You are looking for a green fluorescence in the endomysium covering the muscle fibers. The test is reported as the titer or final dilution in which the fluorescence can still clearly be seen. As you can imagine, this is very subjective. There are no standardized values and it is up to the judgment of the particular technician what the endpoint titer is. Recently, (1998) the endomysial antigen targeted by the anti-endomysial antibodies was identified as the protein cross-linking enzyme known as tissue transglutaminase (tTG). This has enabled the production of an antigen specific ELISA assay incorporating tTG as a reliable and objective alternative to the traditional and subjective Immunofluorescence based assays. In clinical trials, the correlation with the endomysial IFA assay has been shown to be close to 100%. This is a test that has been very well received in the professional community. It is an ELISA, like the anti-gliadin antibody test and, as such, is not subject to interpretation like the IFA. That is the greatest advantage to this new test! With this or any ELISA, the response is measured on an instrument that calculates the amount of light of a particular wavelength that is absorbed by the solution and prints out a numerical result. There is no chance of human error skewing the results because there is no judgment call involved. The ELISA plate, regardless of what you are testing for, is processed with at least three control sera (sometimes as many as eight) in addition to the unknown sample being tested. There is a negative serum and at least two positive sera containing different levels of the antibody being tested. There are specific requirements for the absorption levels of these three controls. That is, each of them has a minimum or maximum (or both) number that must be seen by the instrument in order for it to be a valid test. If there is any variance from these expected numbers, it is an indication that something went wrong and the test results are discarded and the test repeated. There is therefore no way the technician could report inaccurate results, (assuming they diluted the sample correctly). Either the test was valid, and you can rely upon the accuracy of the result, or the test is invalid, and the entire result discarded. If any error was made during the processing of the ELISA plate, it would result in the control sera numbers being out of range and the entire test result would be thrown out. In summary, the tTG ELISA is measuring the same thing that the endomysial IFA is measuring but with a method that is more sensitive and specific and not subject to interpretation. IgA class Reticulin antibodies are found only in Celiac disease and dermatitis herpetiformis. These antibodies are found in approximately 60% of celiac disease patients and 25% of DH patients. This test is falling into disuse because of the limited utility and the availability of better tests. It is an IFA performed on a tissue substrate with all the attendant problems that go along with it. The development of all of these serum assays has tremendously simplified the diagnosis of celiac disease and improved the accuracy as well. The original criteria for diagnosis according to the European Society for Pediatric Gastroenterology and Nutrition, (ESPGAN), involved a year of arduous studies with: An initial positive gut biopsy; 6 months on a gluten free diet; A second, negative gut biopsy; A gluten challenge for 6 months and; A third, positive gut biopsy. The revised ESPGAN criteria call for positive results in two of the serological tests confirmed by a single positive biopsy. In practice, many gastroenterologists are utilizing the serologies in conjunction with a controlled diet and the clinical presentation to form a basis for diagnosis without the need for the invasive procedure. Through the auspices of the Celiac Disease Foundation and others, a professional symposium and workshop was organized earlier this year in Marina Del Rey, California with participants from Europe as well as the U.S. to establish standards for reporting test results. This should improve testing and diagnosis even more. At the conclusion of this conference a Celiac Disease Standardization Committee was formed to investigate and make recommendations on a standardized method of reporting results.- 88 comments
-
Celiac.com 02/05/2023 - If you have celiac disease symptoms, for example chronic diarrhea, anemia, bloating, abdominal pain, rashes, are in a higher risk group, etc., your doctor may order a blood test for celiac disease. Note that before doing any blood tests for celiac disease you must be eating gluten for a while beforehand, and the amount and length of time can vary, but is somewhere between 2 slices of wheat bread daily for 6-8 weeks and 1/2 slice of wheat bread or 1 wheat cracker for 12 weeks, otherwise you may end up with false negative results. For a celiac disease antibody test, a clinician collects a small amount of the patient's blood. The sample is then sent to a lab, where the blood cells are then removed, and the test is conducted. Celiac Disease Blood Tests Note that the accuracy and specificity of each test can vary depending on the laboratory performing the test, the specific method used, and the population being tested. Sensitivity refers to the ability of a test to correctly identify individuals with the condition (true positive rate), while specificity refers to the ability of a test to correctly identify individuals without the condition (true negative rate). tTG-IgA (tissue transglutaminase IgA) Blood Test for Celiac Disease This test measures the levels of IgA antibodies to tissue transglutaminase, an enzyme that is involved in the immune response to gluten in those who have celiac disease. The test is estimated to have a sensitivity of approximately 90%, which means that it correctly identifies 90% of people with celiac disease. It also has a high specificity of around 95%, which means that it correctly identifies 95% of people who do not have celiac disease. Other Names for the tTG-IgA Test: Tissue Transglutaminase IgA Test Anti-Tissue Transglutaminase IgA Test tTG-IgA Blood Test tTG-IgA Serology Test IgA-tTG Antibody Test Tissue Transglutaminase Antibody IgA Assay tTG-IgG (tissue transglutaminase IgG) Blood Test for Celiac Disease This test measures the levels of antibodies to tissue transglutaminase, but it specifically measures IgG antibodies rather than IgA antibodies which are produced in people who eat gluten and have celiac disease. It is not as sensitive or specific as the tTG-IgA test, but it may be useful in cases where a person has an IgA deficiency, which can occur in approximately 2-3% of people with celiac disease. In these cases, the tTG-IgG test may be positive while the tTG-IgA test is negative. However, the tTG-IgG test is not recommended as a first-line screening test for celiac disease. The sensitivity of the tTG-IgG blood test is generally high, ranging from 85% to 98%. This means that the test can accurately detect celiac disease in a significant percentage of people who have the condition. The specificity of the tTG-IgG blood test is also high, typically around 90% to 98%. This indicates that the test can effectively rule out celiac disease in individuals who do not have the condition. Other Names for the tTG-IgG Test: Tissue Transglutaminase IgG Test Anti-Tissue Transglutaminase IgG Test tTG-IgG Blood Test tTG-IgG Serology Test IgG-tTG Antibody Test Tissue Transglutaminase Antibody IgG Assay EMA-IgA (endomysial antibodies IgA) Blood Test for Celiac Disease This is a highly accurate test for celiac disease, that requires specialized expertise to perform and interpret, and it is more expensive than other blood tests. It is generally used as a last test to confirm celiac disease after a positive tTG-IgA test. The sensitivity of a test refers to its ability to correctly identify individuals with the condition. For the EMA-IgA blood test, the sensitivity is generally very high, ranging from 90% to 98%. This means that the test can accurately detect celiac disease in a significant percentage of people who have the condition. The specificity of a test refers to its ability to correctly identify individuals without the condition. For the EMA-IgA blood test, the specificity is also high, typically around 95% to 100%. This indicates that the test can effectively rule out celiac disease in individuals who do not have the condition. Other Names for the EMA-IgA Test: Endomysial Antibodies IgA Test Anti-Endomysium Antibodies IgA Test Endomysial Antibody IgA Assay EMA IgA Blood Test EMA-IgA Serology Test Endomysium IgA Ab DGP-IgA and DGP-IgG (Deamidated Gliadin Peptide) Blood Tests for Celiac Disease These tests measure the levels of antibodies in the blood, but specifically targets deamidated gliadin peptides, which are a type of gluten protein that can trigger an immune response in people with celiac disease. The test is not always included in adults, but should be in cases with IgA deficiency. The test should always be included when screening children, especially if they are under 2 years old. The DGP test was created to detect celiac disease in those with IgA deficiency, as it tests for both IgA and IgG antibodies. The DGP-IgA test is considered to have high sensitivity and specificity. In general, the DGP-IgA test has been reported to have a sensitivity ranging from 75% to 95% and a specificity ranging from 90% to 100%. The DGP tests have been found to have a sensitivity of around 85-95% and a specificity of around 95-98%. Other Names for the DGP-IgA Test: Gliadin Peptide Antibody IgG (Immunoglobulin G) Anti-Gliadin Antibody IgA (AGA IgA) Anti-Gliadin IgA Antibody (AGA IgA) Anti-Gliadin IgA (AGA IgA) Anti-Gliadin Immunoglobulin A Antibody (AGA IgA) Anti-Deamidated Gliadin Peptide IgA (DGP IgA) Anti-Deamidated Gliadin Antibody IgA (DGP IgA) The sensitivity of the DGP-IgG test is reported to range from 75% to 85%, which means it can correctly identify individuals with the condition in about 75% to 85% of cases. The specificity of the DGP-IgG test is reported to range from 75% to 95%, which means it can correctly identify individuals without the condition in about 75% to 95% of cases. Other Names for the DGP-IgG Test: Gliadin Peptide Antibody IgG (Immunoglobulin G) Anti-Gliadin Antibody IgG (AGA IgG) Anti-Gliadin IgG Antibody (AGA IgG) Anti-Gliadin IgG (AGA IgG) Anti-Gliadin Immunoglobulin G Antibody (AGA IgG) Anti-Deamidated Gliadin Peptide IgG (DGP IgG) Anti-Deamidated Gliadin Antibody IgG (DGP IgG) IgA Levels/Deficiency Blood Test This should always be included in any blood panel for celiac disease, but it does not test directly for celiac disease, and is done to determine the accuracy of the other blood tests. People who are IgA deficient may score lower, of have no measurable levels on certain celiac disease blood tests. This test measures the levels of Immunoglobulin A (IgA) in the bloodstream. IgA is an important antibody that plays a significant role in the immune system, particularly in protecting the body's mucosal surfaces (e.g., respiratory and digestive tracts). Low IgA levels can indicate IgA deficiency, a condition where the body does not produce enough IgA, leading to an increased risk of infections and other health issues. The IgA Levels/Deficiency Test helps healthcare providers diagnose and monitor IgA-related conditions. Other Names for the IgA Levels/Deficiency Test: Immunoglobulin A (IgA) Test Total IgA Test Serum IgA Test IgA Serum Levels Test IgA Blood Test IgA Quantitative Test IgA Antibody Test IgA Immunodeficiency Test Celiac Disease Blood Antibody Screening is ~98% Accurate in Adults Using the Mayo Clinic Protocol A celiac disease blood panel includes several tests to determine whether someone has celiac disease. These tests are very specific because certain antibodies only appear in those with gluten sensitivity, celiac disease and/or dermatitis herpetiformis. Testing begins with a test called Immunoglobulin A (IgA). If the results are normal, then a Tissue transglutaminase, antibody, IgA test is given. A weak positive should lead to the following tests: Endomysial antibodies (IgA) and; Gliadin (deamidated) antibody, IgA. If the initial Immunoglobulin A (IgA) test is lower than normal, then these two tests should be done: Tissue transglutaminase antibodies, IgA and IgG profle. Gliadin (deamidated) antibodies evaluation, IgG and IgA. If the initial Immunoglobulin A (IgA) test is below the level of detection (<1.0 mg/dL), then these two tests should be done: Tissue transglutaminase (tTG) antibody, IgG. Gliadin (deamidated) antibody, IgG. It sounds complicated, but it's pretty standard procedure now, and when blood screening is done this way the results for celiac disease are ~98% accurate. Many People Can Be Diagnosed Using Only Blood Tests and No Biopsy According to the latest research, if the blood test results are at certain high levels that range between 5-10 times the reference range for a positive celiac disease diagnosis, it may not be necessary to confirm the results using an endoscopy/biopsy: Blood Test Alone Can Diagnose Celiac Disease in Most Children and Adults TGA-IgA at or Above Five Times Normal Limit in Kids Indicates Celiac Disease in Nearly All Cases No More Biopsies to Diagnose Celiac Disease in Children! Biopsy Still Standard in Adult Celiac Diagnosis After positive blood tests some doctors still require a biopsy to confirm the diagnosis. However, this is changing, as new techniques allow doctors to accurately detect celiac disease in adults without a biopsy. Remember, nearly all tests and screening for celiac disease require the patient to be eating a gluten-containing diet before testing, usually you should be eating at least 1/2 slice of wheat bread or 1 wheat cracker daily for at least 2 weeks before the endoscopy. Be sure to check with your doctor for the latest protocol. Blood Tests for Follow Up Care Blood tests may also be useful in follow up care in those with celiac disease to confirm that their diet is indeed free of gluten. Also, because of the lack of standardization, keep in mind that blood test results may not be directly comparable from one lab to the next. More Celiac Disease Testing Resources What is a Gluten Challenge and How Long Must it Last? Interpretation of Celiac Disease Blood Test Results Ten Facts About Celiac Disease Genetic Testing Blood Test Questions on the Celiac Disease and Gluten-Free Forum Test results and question about gluten challenge How Long To Eat Gluten For Accurate Blood Test Read more at mayocliniclabs.com
- 59 comments
-
- accurate
- antibodies
-
(and 4 more)
Tagged with:
-
Celiac.com 06/06/2022 - Researchers have shown that tissue-transglutaminase antibodies (TGA) can be used to diagnose celiac disease without biopsy, but there's no good data on how accurate it is in real life conditions. A team of researchers recently set out to investigate real-life performance of a Bioplex2200 automated celiac serology analyzer, and to explore the correlation between tissue-transglutaminase antibody levels and intestinal biopsies in children. The research team included Anat Guz-Mark; Michal Kori; Chani Topf-Olivestone; Ronit Weinberger; Sara Morgenstern; Nadya Ziv-Sokolovskaya; and Raanan Shamir. They are variously affiliated with the Institute of Gastroenterology, Nutrition and Liver Diseases, Schneider Children's Medical Center of Israel, Petach Tikva; the Sackler Faculty of Medicine, Tel-Aviv University, Tel-Aviv; the Pediatric Gastroenterology, Kaplan Medical Center, Rehovot; the Faculty of Medicine, Hebrew University of Jerusalem, Jerusalem; the Immunology Laboratory, Clalit Health Services, Tel Aviv; the Institute of Pathology, Rabin Medical Center, Pitach-Tikva; and the Institute of Pathology, Kaplan Medical Center, Rehovot, Israel. The team conducted a retrospective review in two pediatric gastroenterological centers, between November 1, 2018 and April 1, 2020. They included patients with both tissue-transglutaminase antibody serology testing and duodenal biopsies. They gathered data including patient demographics, medical background, TGA levels, and biopsy results. In all, the team looked at 538 children. They found 256 with positive tissue-transglutaminase antibodies, and 282 with negative tissue-transglutaminase antibodies. Among patients with positive tissue-transglutaminase antibodies, intestinal biopsies confirmed celiac disease in 219, or nearly 86% of cases. The team found positive serology with normal histology in about fifteen percent of the cases. In more than half, they found tissue-transglutaminase antibody ranges of 1 to 3 times upper limit of normal. About twenty percent had tissue-transglutaminase antibody ranges 3 to 5 times upper limit of normal; about twenty percent had tissue-transglutaminase antibody ranges 5 to 10 times upper limit of normal; and just over 4% had tissue-transglutaminase antibody ranges above 10 times upper limit of normal, respectively. Nearly eighty-five percent of patients with positive tissue-transglutaminase antibodies also had positive anti-endomysial antibodies. However, overall diagnostic performance in these patients was inferior. The team found that the Multiplex tissue-transglutaminase antibody assay accurately diagnosed celiac disease in real world conditions. EMA screening did not improve the diagnostic accuracy in patients with positive tissue-transglutaminase antibodies. Meanwhile, false-positives varied depending on tissue-transglutaminase antibody range, but were low in patients with tissue-transglutaminase antibody levels above 10 times upper limit of normal. The ability to use multiplex tissue-transglutaminase antibodies for accurate celiac diagnosis offers clinicians another cheap and easy tool for catching celiac disease early. The easier and cheaper it becomes to diagnose celiac disease, and the earlier it can be caught, the more long term damage can be avoided for celiac sufferers. Read more in the Journal of Pediatric Gastroenterology and Nutrition
-
- blood
- blood tests
- (and 8 more)
-
Celiac.com 07/06/2021 - People who have celiac disease have to eat a gluten-free diet, otherwise, they risk physical discomfort, intestinal damage, and potentially increased risks for numerous related conditions, and even deadly types of cancer. Most tests that screen for celiac disease work by detecting the antibodies that indicate the presence of celiac disease. One of the big drawbacks about celiac disease blood screening is that people usually have to eat gluten for 6-12 weeks in order for the tests to be accurate, and sometimes wait a couple of weeks more before the final results are known. This is often followed by a biopsy where you need to continue eating gluten for even longer periods. That can mean weeks or months of feeling very bad, followed by weeks of uncertainty for many people who are trying to figure out if they have celiac disease. But what if we could screen for celiac disease in a quick, reliable and accurate way? That's been an elusive goal for researchers for many years. That may be set to change, with the recent discovery by Anna Nguyen, a biochemistry student from at Metropolitan State University of Denver. Ngyuen has discovered a faster, easier way to detect celiac disease. The discovery arose as part of Nguyen's 2016 undergraduate research project. “I was really passionate about learning nutrition and diet, but eventually I got to the point where I was more interested in the science behind nutrition,” Nguyen said. “And it led me down this biochemistry route and wanting to get my Ph.D., which requires you to do undergrad research.” The method developed by Nguyen, and her fellow undergraduate researchers, would be faster and easier, and require a simple finger prick. “What we wanted to do was just do make a quick blood test that, maybe just after a day of eating gluten, you could be able to go to your doctor, get a pinprick blood test, and it would just tell you immediately.” The only problem is that Ngyuen's test uses an electrochemical biosensor. Even though electrochemical biosensor technology is currently not laboratory approved, the team is hopeful that it can be developed into a fast, convenient, and reliable test that will be used widely by both clinicians and patients. Keep an eye out over the next few years for more on this and other improvements in celiac blood testing. Read more at: 9news.com
- 1 comment
-
- antibodies
- blood
-
(and 5 more)
Tagged with:
-
Celiac.com 09/24/2020 - Celiac disease is an autoimmune condition in which eating wheat, rye, or barley triggers an adverse immune reaction in the gut. Celiac disease affects about one percent of the population. Diagnosis can be a long and arduous process. In the United States, the average person with celiac disease can wait up to ten years from the time of first symptoms to diagnosis. Left undiagnosed, autoimmune disease can cause organ damage and bowel cancer. Anyone who has ever had to suffer through a long, convoluted process to get their celiac disease diagnosis can now rejoice for any new celiacs going forward. That's because researchers have developed a single blood test that can diagnose celiac disease without biopsy. Until now, the "gold standard" for celiac diagnosis was the duodenal biopsy, which is normally performed by a gastroenterologist in the days or weeks after a positive blood test, during which time the patient needs to keep consuming gluten. However, nearly half of patients did not need to undergo a more risky biopsy procedure at all. This data, coupled with the need to catch up with a backlog of endoscopies created during the Covid-19 pandemic, has provoked a change in guidance from the British Society of Gastroenterology and The National Institute for Health and Care Excellence (NICE). An upcoming report by British researchers for the leading gastroenterology journal Gut, shows that the standard tTG blood test alone is 95 percent accurate for diagnosing celiac disease. Trials show the tTG blood test to be 95 percent sensitive (meaning it detects celiac disease 95 times out of 100), and 95 percent specific (meaning it gives a false positive result just 5 times out of 100). The test measures blood levels of anti-transglutaminase antibodies, or tTG2, which are higher in people with celiac disease. TTG2 proteins are among the proteins trigger the immune reaction the causes inflammation when celiac eat wheat, rye, or barley. Celiacs have hundreds times more tTG proteins than non-celiacs. Being able to diagnose celiac disease quickly and accurately, via blood test alone, is a huge game-changer for celiac patients. Tens of thousands of people with suspected celiac disease can now get a diagnosis with a simple blood test, sparing them from the more risky biopsy procedure. Not only will many be spared the prolonged side-effects, and invasive, drawn-out diagnosis, they will also be spared the long-term damage that come with undiagnosed celiac disease. Read more at DailyMail, news-medical.net, and bmj.com.
- 35 comments
-
Celiac.com 05/27/2020 - Recurrent aphthous stomatitis (RAS), or canker sores, is one of the most common oral mucosa conditions, and may be related to vitamin deficiencies or immune conditions such as celiac disease. A team of researchers Turkish Republic Health Ministry recently set out to determine rates of hematinic deficiency and celiac disease in children with RAS. The research team included Songül Yılmaz, Ceyda Tuna Kırsaçlıoğlu, and Tülin Revide Şaylı. They are variously affiliated with the Department of Pediatric Gastroenterology, and the Department of Pediatrics at the Turkish Republic Health Ministry, Ankara Child Health Diseases, Hematology and Oncology Training and Research Hospital, Ankara, Turkey. The study included patients from 6 months to 18 years in age, who were diagnosed with RAS at the study institution from 2010–2011, and who had experienced at least three or more episodes of aphthous stomatitis in the prior year. The research team excluded patients with chronic illness, acute infection, or those receiving immunosuppressant drug treatment. The team also included a control group of similarly aged children without RAS, who were being seen in pediatric outpatient clinics. The research team reviewed medical records of RAS patients, looking for the evidence of celiac disease, and also hematinic deficiencies, including hemoglobin, mean corpuscular volume, ferritin, vitamin B12, and folic acid. In all, the team reviewed records for 108 children with RAS, and nearly 60 healthy children assessed for hematological abnormalities during regular examination. Nearly 35% of the RAS group patients had a family history of RAS, compared with just 7% for the control group. The data showed hematological abnormalities in nearly one-third of the RAS group, compared with 10.5% for the control group, along with significantly higher rates of iron deficiency anaemia for the RAS group. Three patients, about 3% of RAS patients were diagnosed with celiac disease, which is much higher than rates seen in healthy children in Turkey. The children also commonly showed mild malnutrition, iron deficiency and iron deficiency anaemia. Based on their data, the researchers are recommending nutritional and hematological assessment for children with RAS. They also recommend the doctors consider celiac disease screening for children with hematological abnormalities and malnutrition. Read more in Pediatrics International; 2020 19 January
- 7 comments
-
- aphthous stomatitis
- blood
- (and 5 more)
-
Celiac.com 11/25/2010 - Are you are interested in getting tested for celiac disease but would like to use an affordable and reliable company—perhaps one that even offers the option of confidential celiac disease blood screening? If your answer is yes to any part of this question I would highly recommend ClickMDLab.com. ClickMDLab.com is an online company that offers celiac disease testing via certified LabCorp laboratories, which are conveniently located throughout the USA. ClickMDLab.com offers a confidential screening service that allows you to completely bypass a trip to your doctor’s office—which means that your test results will not end up in your medical records (should you choose this option). My sister recently used their service to be screened for celiac disease via their celiac disease complete panel blood test. Within a few days my sister received her results via e-mail, and she didn't have to deal with a trip to the doctor's office and long wait times associated with the normal screening process. Her results were well-documented and easy to read, and on top of this the staff at CickMDLab.com were available and willing to assist her with any additional questions that she had. My sister had a wonderful first-time experience and we feel it's necessary to spread the word about this great new service.
-
- affordable
- blood
-
(and 5 more)
Tagged with:
-
Celiac.com 04/06/2020 - Celiac disease is an autoimmune disease driven by exposure to gluten in people who carry certain genes. Despite better awareness, easier testing, and rising rates of celiac disease, many patients remain undiagnosed. The expense, inconvenience, and invasiveness of standardization blood tests has led to the development of several point-of-care tests (POC) for celiac disease. A team of researchers recently set out to assess celiac disease rates in first-grade pupils in Primorje-Gorski Kotar County, Croatia, using a POC test. The research team included Kristina Baraba Dekanić, Ivona Butorac Ahel, Lucija Ružman, Jasmina Dolinšek, Jernej Dolinšek, and Goran Palčevski. They are variously affiliated with the Department of Pediatrics, University Hospital Center Rijeka, Istarska 43, 51 000 Rijeka, Croatia; the Office of Project Development-Project Office, Municipality of Maribor, Ulica Heroja Staneta 1, Slovenia; and the Department of Pediatrics, University Medical Center Maribor, Ljubljanska 5, 2 000 Maribor, Slovenia. The team used a Biocard celiac test that detects IgA antibodies to tissue transglutaminase in whole blood on a group of healthy first-grade children born in 2011 and 2012 who freely consumed dietary gluten. In all, the team tested 1,478 children, none of whom tested positive with a rapid test. Researchers suspected IgA deficiency in ten children, only four of whom agreed to be tested further for total IgA, anti-tTG, and anti-DGP antibodies. Those further tests confirmed IgA deficiency in three patients, while celiac disease was excluded in all four children. Based on these results, current POC tests were not useful in screening for celiac disease in the general population of first-grade schoolchildren. The team notes that more research is needed to catch all cases of celiac disease in Primorje-Gorski Kotar County, and to establish the usefulness of rapid celiac testing against standard celiac antibody testing. So, don't look to finger-prick tests or other point-of-care tests to revolutionize celiac diagnosis, at least in the short to near-term. Read more in Gastroenterology Research and Practice / 2019
-
I had a celiac blood "screen" ordered through a GI consultant at a hospital last Friday (23rd November) and was wondering how long you recon it would take for the results to come back. As this was done through a consultant the results won't go straight back to my GP and I can't ring up. The hospital seems to mainly communicate through letters so I was wondering if they'd send a letter with the results it may take a bit longer to come back (I only just got a letter summarising the consultation I had before my test today). I'm just very anxious waiting for the results. (This was done on the NHS in the UK) Please does anyone remember how long it took for their blood results to come back? I'm really desperate.
-
Celiac.com 10/21/2019 - Parents, siblings and children of people with celiac disease are not only more likely to develop the autoimmune disease, they are more likely to develop a "silent" version, which presents few or no obvious symptoms, according to the results of a recent study. Because of this, Mayo Clinic researchers are now recommending that these first-degree relatives of celiac patients undergo celiac screening. Celiac disease is an autoimmune condition that causes gut damage when those affected consume gluten, a protein in wheat, barley and rye. A strict gluten-free diet is currently the only treatment for celiac disease. The study of celiac patients and their families showed that nearly half of close relatives who received celiac blood tests were later diagnosed with the condition. Nearly all of them had atypical symptoms or no symptoms at all. These results are startling, as are the recommendations to test people who show no symptoms, just based on their close relation to known celiac patients. That's unusual, because researchers usually keep their screening efforts restricted to those who show symptoms. Current guidelines call for testing family members when children are diagnosed with celiac disease, but, until now, when adults are diagnosed, called for testing only those close relatives who show symptoms. However, the study shows a clear likelihood of celiac risk in close relatives, which led to the Mayo Clinic's recommendation to extend testing to all close family members of known celiac patients. It's important to diagnosed celiac disease as quickly as possible. Untreated celiac disease patients face an elevated risk of developing other conditions like nutritional deficiencies, anemia, osteoporosis and even lymphoma. This is really huge news, as it means that large numbers of people likely have celiac disease without even knowing it. So, if you or your loved ones know anyone with celiac disease, pass along this information. Their immediate family members should probably get screened for celiac disease. Hopefully, this study and will trigger more like it, and increase testing of asymptomatic people who are at high risk for undiagnosed celiac disease. Read more in the Mayo Clinic Proceedings, online August 22, 2019, and at Reuters.com
- 1 comment
-
- blood
- celiac disease
-
(and 7 more)
Tagged with:
-
Has anyone had high blood protein at or before diagnosis? Specifically, "polyclonal hypergammaglobulinemia" or "polyclonal gammopathy," caused by inflammation. My gamma globulin is high, putting total protein at 9. I've had every test short of a scope & dr's can't find an obvious source. For 3 yrs I've had difficultly maintaining weight & lost 15 lbs, only recently gaining it back on a very unhealthy high-fat diet. The symptom pointing to celiac is occasional shredded/mushy stools, with stringy mucus-like stuff in it, sometimes white fuzzy stuff. Honestly it looks like candida from googling. If tTG IgA & IgA celiac panels are normal, can it still be celiac? *POOP PICS* (for those willing) ?: Shredded poop: https://imgur.com/a/qoLH8a4 Stringy mucus: https://imgur.com/a/kvLLFGi Soft w/ stringy mucous: https://imgur.com/a/5XwQBr9
- 4 replies
-
- blood
- gammopathy
-
(and 5 more)
Tagged with:
-
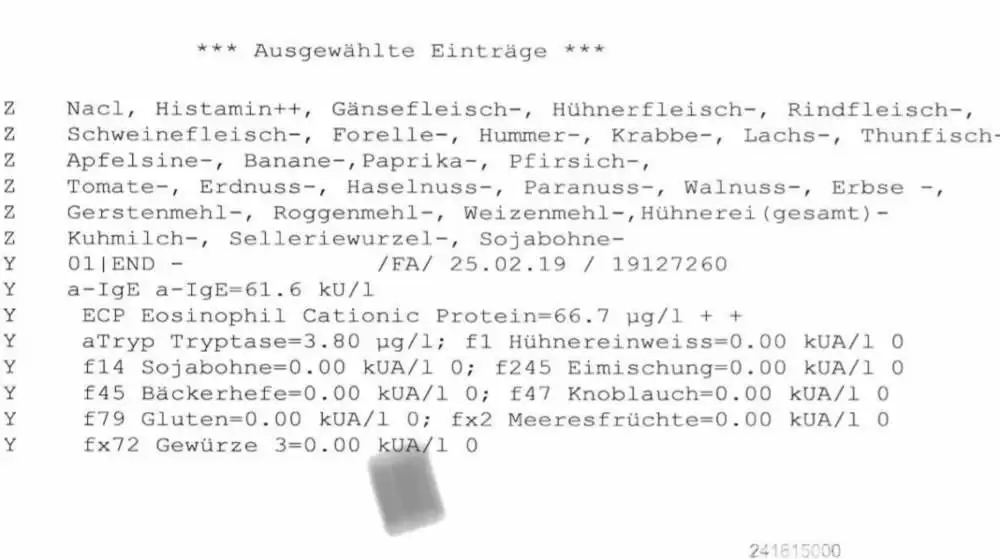
I had a blood test from an allergist and my ECP levels were 3x normal range. ECP differs from standard eosinophil percentage that is common in a CBC blood test. Levels are 66.7ug/l normal is <20ug/l. From what I read this is pretty dangerous and is also a marker for tumours or can cause organ damage. It is also termed as eosinophilia which is quite scary. I couldn’t find anything related to this on the forum which also makes me wonder what is going on. Any advice?
-
How long did it take you to get your blood test results? How were you notified of the results (letter, phone call etc.)?
- 3 replies
-
- blood
- blood test
- (and 4 more)
-
Celiac.com 09/03/2018 - Can an office-based point of care test (POCT) improve celiac disease detection and diagnosis? A team of researchers recently set out to measure the diagnostic performance of an IgA/IgG-deamidated gliadin peptide (DGP)-based POCT for celiac disease detection, patient acceptability, and inter-observer variability of the POCT results. The research team included Michelle S. Lau MBChB, Peter D. Mooney MD, William L. White MBChB, Michael A. Rees BMedSci, Simon H. Wong MBChB, Marios Hadjivassiliou FRCP, Peter H. R. Green MD, Benjamin Lebwohl MD & David S. Sanders FRCP. They are variously affiliated with the Academic Department of Gastroenterology, the Academic Department of Neurosciences and University of Sheffield, Royal Hallamshire Hospital, Sheffield Teaching Hospitals, Sheffield, UK, and with the Celiac Disease Centre at Columbia University Medical Centre in New York, NY, USA. Beginning in 2013, and running through 2017, the team recruited patients who had been referred for secondary care with gastrointestinal symptoms, anemia and/or weight loss (group 1), along with a group of patients with self-reported gluten sensitivity, but unknown celiac disease status (group 2). Every patient in the study received a POCT, tests for IgA-tissue transglutaminase (IgA-TTG), IgA-endomysial antibodies (IgA-EMA), total IgA levels, and a duodenal biopsy. A total of 500 patients completed acceptability questionnaires, and the team compared inter-observer variability of the POCT results among five clinical staff for 400 cases. Group 1 included 1,000 patients. The team saw forty-one patients (4.1%) diagnosed with celiac disease. The sensitivities of the POCT, IgA-TTG, and IgA-EMA were 82.9, 78.1, and 70.7%; the specificities were 85.4, 96.3, and 99.8%. Group 2 included 61 patients. The POCT showed 100% sensitivity, but negative predictive value in detecting celiac disease in group 2. A majority of patients preferred the POCT to a blood draw (90.4% to 2.8%). A Fleiss Kappa coefficient of 0.895 reflected good inter-observer agreement on the POCT results. The POCT had comparable sensitivity to a blood test, and accurately spotted all celiac disease cases in a gluten sensitive group. But, because its low specificity may could cause further unnecessary tests, it’s not good enough to take the place of blood testing. It turns out that spotting celiac disease is only part of the battle. Making sure to rule out people who don’t have celiac disease is equally important. That’s why it’s important that any diagnostic test be both sensitive, to spot celiac disease, and specific, to rule out celiac disease in those who don’t have it. Until we get a PCOT with high enough sensitivity and specificity to make accurate celiac diagnosis and accurate elimination of those without celiac disease, the current blood testing regime will continue. Read more at: The American Journal of Gastroenterology; volume 113, pages1238–1246 (2018)
- 4 comments
-
- blood
- blood test
-
(and 4 more)
Tagged with:
-
A week ago Johnny Rockets mistakenly served us regular gluten buns, not thinking of the miscoloring, I ate it. I had EXTREME gas pain, bowel movements and blood the night after and have been suffering through tons of blood when having a bowel movement ever since. Tonight though.. I had the weirdest looking poop like seperated in weird ways and I don’t know if it should be a concern? I’m sorry for any graphic images but I need to know asap!
-
If anyone could clear this up for me it would be really helpful. My primary care doctor wasn’t able to get me in for months and my insurance isn’t very good so I found a lab online to do blood work. i only did the gluten allergy IGg blood test. I got my results online today and I don’t understand them fully. From what it says I’m ‘in range’ but my range is exactly what the range number is. Therefor is it higher than average just not high enough to be out of range? This is the results I have. In range <2.0 Reference range <2.0 mcg/mL so technically I’m not over the range but there’s nothing to reference, as in do most people that aren’t gluten sensitive have a 0? Because I feel awful most days with serious brain fog, anxiety and depression and massive headaches that never go away and stomach cramps and I can’t see what else could be causing this. I already had an ultrasound from my gynecologist and I don’t have anything visably wrong on the ultra sound causing the stomach cramping. Any insight would be helpful since I can’t get a doctor to fully interpret this. Thank you!!
-
Hi, im just wondering how long you all waited for your results for endoscopy biopsy? I rang the lab today and apparently they have already been sent to my gp! That seems really quick to me! Also what were your symptoms? i went gluten free about 10 years ago. Was having stomach issues. Did every test but the endoscopy (I chickened out). Fast forward stomach issues returned. So return for a bunch of tests. Got diagnosed with Hashimotos. So Doc recommended confirming celiac. Gluten challenged. Omg that really sucked! Crippling pain, tired all the time. Toilet drama, I looked pregnant, so much so that people actually asked! So bloated! Gong to Gp tomorrow...
-
So a couple years ago I was tested for celiac... Ttg IgG/IgA were all negative DGA IgG/IgA were all negative AGA IgG: Positive AGA IgA Negative HLADQB1*02 Negative HLADQB1*03:02 Negative HLADQA1*05 Positive Biopsies have all been negative. I suffer from Hashimoto's thyroiditis and I just feel miserable with all the body aches and brain fog. My son was born back in July and I'm just so tired of not feeling well and I really want to finally feel good and enjoy life to the fullest. I'm thinking of asking for my labs to be repeated again and see. I'm just wondering if it is possible for me to still have celiac or if I'm just looking for something that just isn't there because I'm desperate for answers... Appreciate any input!! Thank you
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8-M):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8-M):








.webp.0b9a356d292386241ecc4ffb1e3697ee.webp)