-
Welcome to Celiac.com!
You have found your celiac tribe! Join us and ask questions in our forum, share your story, and connect with others.
-
Celiac.com Sponsor (A1):
Celiac.com Sponsor (A1-M):
-
Get Celiac.com Updates:Support Celiac.com!
Search the Community
Showing results for tags 'brain'.
-
Celiac.com 08/15/2023 - Researchers from the University of Otago in New Zealand recently studied the effects of dietary wheat gluten on the hypothalamus of male mice. The researchers include Mohammed Z. Rizwan, Romy Kerbus, Kaj Kamstra, Pramuk Keerthisinghe, and Alexander Tups. Their findings are intriguing. The researchers are variously affiliated with the Centre for Neuroendocrinology and Department of Physiology at the University of Otago School of Biomedical Sciences in Dunedin, New Zealand; the Centre for Neuroendocrinology and Department of Anatomy at the University of Otago School of Biomedical Sciences in Dunedin, New Zealand, and the Maurice Wilkins Centre for Molecular Biodiscovery in Auckland, New Zealand. Gluten is commonly found in wheat, rye, and barley, and is a major dietary component in many western countries. Gluten has been linked to weight gain and peripheral inflammation in mice. This research aimed to understand its impact on central inflammation, particularly in relation to diet-induced obesity. Low-fat Diet vs. High-fat Diet with Gluten The study observed that adding gluten to a low-fat diet had no discernible effect, but male mice fed a high-fat diet enriched with gluten exhibited increased body mass and adiposity compared to those on an high-fat diet without gluten. Additionally, when gluten was introduced to the low-fat diet, it led to higher levels of circulating C-reactive protein. Interestingly, it made no difference whether gluten was added to a low-fat or a high-fat diet. Either way, it triggered a significant increase in the number of microglia and astrocytes in the arcuate nucleus of the hypothalamus. These changes were identified using specific markers through immunohistochemistry. Even on an low-fat diet, gluten appeared to replicate the immunogenic effects seen with an high-fat diet, and its inclusion in the latter led to a further rise in the number of reactive immune cells. Gluten Triggers an Obesity and Injury to the Hypothalamus Overall, the findings suggested that gluten had a moderate obeso-genic effect, when given to mice exposed to an high-fat diet. Moreover, the study reported that gluten triggered the presence of astrocytes and microglia in the hypothalamus, indicating a potential injury to the hypothalamus in rodents. Mice are used in studies to model human disease risk due to genetic similarities, allowing researchers to investigate potential factors and develop treatments in controlled, ethically manageable settings. This research contributes to our understanding the complex relationship between dietary components, like gluten, and obesity-related inflammation in the brain. It also offers up some exciting areas of further research inquiry into the brain's response to gluten in both mice and humans. Read more in the Journal of Neuroendocrinology
- 2 comments
-
Celiac.com 10/22/2008 - The Gluten Syndrome refers to the cluster of symptoms that you experience if you react to gluten. Gluten can affect your gut, your skin, and your brain. It applies to any reaction that is caused by gluten. It includes celiac disease, along with the myriad symptoms that can be experienced throughout your gastro-intestinal tract in response to gluten. It also includes many other symptoms that do not stem from your gut. These include brain and behavior disorders, irritability and tiredness, skin problems, muscular aches and pains and joint problems. The effects of gluten are wide ranging and are now brought together under the term Gluten Syndrome. In most instances, a simple blood test (the IgG-gliadin antibody test) can identify those people who are affected. 10% Affected by Gluten The Gluten Syndrome affects about one in ten people. However, most people who are affected are unaware that their life is being hindered by gluten. The gluten symptoms are most likely to be caused by damage to the nerves and brain. The earlier the problem is identified, the better the response to a gluten-free diet will be. Tummy Pains and not Growing Jonti is 3 years old. His gluten story is typical. His mother brought him to see me because she was concerned about his poor growth, and his distressing abdominal pains. His blood tests showed a high gluten test (His IgG gliadin was 94 units. This test result is usually less than15 at this age). Other tests, including the gene test for celiacs, showed that he did not have celiac disease. I suggested that he go on a gluten-free diet. Within days he began to eat better, and his tummy pains went. He is now growing again on a gluten-free diet. His mum wrote: “I really haven’t found the gluten-free diet that difficult. I found people to be incredibly helpful actually, both in the supermarket and in restaurants. In the supermarket there is a lot of normal type food that is gluten-free and it is all clearly labeled that it is gluten-free. Even if you go to the delicatessen department they will tell you which luncheon sausage is gluten-free. There are gluten-free sausages all labeled and it’s normal food that tastes great. For the baking mixes and bread mixes, you don’t even have to go to the specialist health food shops. I go to no other shops other than the supermarket to get food for him and I haven’t really found it that difficult.” Amazed how Jonti has Adapted I have been amazed, actually, by how easily Jonti has adapted to the gluten-free diet. I tell him it is special food for him and that it won’t hurt his tummy. We have got nice biscuits from a bakery and he is allowed to choose which one he wants for morning tea. He still has normal foods like chips and sweets. He is not missing out and the other biscuits he hasn’t even really asked for. The only thing is the bread! I have yet to perfect the making of the bread. Toast is about the only thing he asked for. You can get specialist cornflakes and cereals, porridge he loves, again, at the supermarket. It has been surprisingly easy actually I’m so pleased that he is now well again. Gluten-free has made such a huge difference.” The Main Points: The Gluten Syndrome refers to the cluster of symptoms that you experience if you react to gluten. It can affect your gut, skin and nerves. Medical practitioners accept that gluten causes celiac disease(gut damage) but often resist the notion that gluten can cause a wider spectrum of illness. Celiac disease, gluten intolerance and gluten sensitivity are all part of The Gluten Syndrome. Rapidly accumulating medical evidence shows that gluten is now creating a massive health problem throughout the Western world. However, woefully few people are aware of the catalogue of harm that gluten is causing. About one in ten people—that is millions of people—are affected by The Gluten Syndrome. Gluten could be responsible for one-third of all cases of chronic illness and fatigue. People suffering from these conditions are currently just tolerating their symptoms, unaware that gluten is the culprit. This is because the link to gluten is not yet recognized by the medical community. Gluten-containing products are being added to our food chain in increasing amounts. Our wheat is being engineered to have even higher gluten content. This gluten overload is occurring without our communities being unaware of the harm that this is causing. Gluten can cause malfunctions of the brain and neural networks of susceptible people. The incidence of mental, neurological and brain disorders is on the rise. However, the diagnosis of gluten-sensitivity is seldom made. The community is already embracing the notion of gluten-sensitivity. More and more people are opting for a gluten-free lifestyle. These people are looking for a term to identify their illness. Their search is over. They have been affected by The Gluten Syndrome. A strong gluten-free movement is developing globally in response to the knowledge that going gluten-free can be so beneficial to so many people. What has been missing up until now is a name that captures the gluten problem. The missing name is The Gluten Syndrome. Get Your Blood Tests The Gluten Tests Gluten is a protein that is found in wheat grains. This protein has a number of components, one of which is called gliadin. People who get sick from gluten are usually reacting to the gliadin component. You are a Long Tube To understand what the blood tests mean, first you need to know a little more about your immune system. It is the job of your immune system to protect you from the outside world. It protects you from the invasion of microbes (viruses and bacteria), and it also protects you from the toxins and poisons in the food that passes through your gut. Your gut is a long tube inside you that travels from your mouth to your anus. This is your gastrointestinal tract, also called your bowel. Even though it is inside your body, the contents of this tube are still on the ‘outside’ from your body’s point of view. Lots of your immune cells coat the skin (called the mucosa) of this tube and work hard to protect you from anything that might prove to be harmful. Gluten (Gliadin) can be Toxic Gliadin, the toxic component of the gluten protein, is one such harmful substance. Your immune system defends your body strongly against gliadin using weapons called antibodies and the gliadin is repelled. The outcome of your immune system’s fight against gliadin is the production of antibodies that are specifically targeted towards gliadin: these are called anti-gliadin antibodies. Gliadin Antibodies Anti-gliadin Antibodies (commonly called the IgG-gliadin antibody) are weapons that have been made specifically to fight against gluten in the diet. Remember, gliadin is a component of the gluten protein. This antibody is very sensitive. It is made very specifically by your immune system to fight against gliadin. However, a high level of this antibody does not necessarily mean that you have any gut damage, so it is not very accurate in assisting the identification of patients with celiac gut damage. On the other hand, tests for this antibody are nearly always strongly positive in people with celiac disease who are not on a gluten-free diet. Once people are placed on a strict diet, these antibodies will fall to normal levels within a period ranging from few months to a year or two. Gluten Tests Not Getting Done There is a problem. Unfortunately, this gluten blood test (the IgG-gliadin antibody test) is no longer available from most community laboratories. This year many laboratories have decided to discontinue this test. Their opinion is that it is worthless (for detecting celiac disease). I disagree with their decision. My latest data shows that huge numbers of people remain undiagnosed with serious symptoms because of the misinterpretation of this gluten test result. At the moment it is difficult to get the medical labs to do your gluten test. They are unwilling to consider that gluten causes a wide spectrum of illness that has been written up in the international medical literature. They have turned a blind eye to the problem. If you can’t test for gluten reactions, then you will not be able to make the diagnosis! A Diagnosis at Last! Mandy wrote this letter to me: “Hi Dr Rodney Ford, for many, many, years I have been to doctors complaining of a bloated tummy, extreme cramping pains, and diarrhea (to the point I had no time to get to the toilet). I have recently had some blood test for celiacs done by my GP. My results showed: the tTG was negative; and the IgG-Gliadin result strongly positive. He could not explain it to me, but he said that Idid not have celiac disease.” “I have no idea what these tests mean. Although I got no answers, I had to try something. I was at the end of my nerves! My bad health has always been upsetting my social and working life. I often have to rush home to the toilet.” Amazing on a Gluten-free Diet “So I decided to try a gluten-free diet! I have now been gluten-free for a month. It is amazing! Already I feel like a different person! No more bloating, just the odd stomach cramp. Also, all my headaches have gone. But I still feel really tired and not sure how to overcome this. Can you help me please by explaining my blood test results—and should I have anymore tests? What else I can do to help myself? I hope you can help me Dr Ford. Gluten, up to now, seems to have made my life a misery. Even though I feel so much better already, I want to get even better. Kind regards, Mandy.” The Gluten Syndrome I replied: “Thanks. I am glad that you are feeling a lot better off gluten. From your story and your blood test results, you have gluten-sensitivity. You do not have celiac disease (your low tTG level shows that you do not have any gut damage from gluten). But you are still getting sick from gluten (your high IgG-gliadin level shows that your body reacts to gluten). The good news is that it takes many months to get the full benefits of a gluten-free diet. I expect that you will continue to feel better over the next few months. You should be taking some additional iron and a multivitamin supplements because you will be relatively iron deficient—that will be making you tired.” The Time has Come The history of science and medicine is littered with vehement arguments against any new idea that runs contrary to traditional beliefs. Ironically however, it takes new ideas to make progress. It was George Bernard Shaw who said that “The reasonable man adapts himself to the world: the unreasonable one persists in trying to adapt the world to himself. Therefore, all progress depends on the unreasonable man.” Thousands Convinced Many people are joining the ranks of the gluten-free. There are thousands of people like you who have read this information and who are concerned about how gluten might be affecting them; there a millions of people who are sick and tired of being ignored and who are looking for more energy and vitality; there are the practitioners in the field of complementary medicine who are aware of the concept of gluten-sensitivity; there are the laboratories who have developed the gliadin antibody test and know that their tests are specific for gluten reactions; there are the gluten-free food manufacturers who have recognised that there is an ever-increasing demand for gluten-free products; there are the networks of people in the health food industry who appreciate the value of high-quality food and a gluten-free diet; and there are the supermarkets and grocery stores that are sensitive to the demands of their customers. Who Might Oppose this Trend? As previously discussed, medical practitioners are wary of overturning tradition. They do not want to be seen as alternative and want to avoid acting outside of the recommended clinical guidelines. In addition, there are the grain-growers and the bread-makers who make their living from gluten, and the pharmaceutical companies who make their living from the sick and unwell. Bad Behavior on Gluten Kimberley is 12 years old. She has The Gluten Syndrome and her behavior gets disturbed with gluten. She does not have celiac disease but she does have a high gluten test. (Her IgG-gliadin level was 55 units—It should be less than 20.) Her mum said: “It is interesting about how behavior troubles are linked to gluten! Our youngest, Kimberley, is now 12 years old. She had her IgG-gliadin measured and it was high. She was clearly a lot better when she was off gluten. However then she decided to ‘try’ gluten again. Rodney suggested a small amount but she went for it—big time!” By the end of a week, two other parents had asked what was wrong with her. Another parent asked “what on earth’s the matter with her” she seemed so different and stroppy. She admitted she felt “absolutely awful” but really didn’t want to admit it as she knew it meant she’d have to completely give up gluten.” Anyway, after a lot of talking, she agreed it wasn’t in her best interests to eat gluten. From that day she has been gluten-free ever since, with the odd very long envious glance at French bread! With our support she’s very compliant with being gluten-free now, which I think is remarkable for her age. Clearly she now understands and gets the benefits of gluten-free. But I was really shocked at how affected her behavior was after are introduction of gluten.” Could You Have The Gluten Syndrome? One in every ten people is affected by gluten. If you have chronic symptom(feeling sick, tired and grumpy) then you should get checked for The Gluten Syndrome.
- 18 comments
-
Celiac.com 12/11/2006 - Yes, that's what I think. Gluten-sensitivity is a disease of your brain and nerves. The gluten puzzle I have come to this conclusion after studying the effects of gluten on my patients for over a decade. I am a pediatric gastroenterologist and allergist. I run a busy clinic for children and their parents. I have been increasingly concerned by the large numbers of my patients who are affected by gluten. I was perplexed by their wide-ranging symptoms. The puzzle was to explain how gluten could cause so much ill health to so many people in so many different ways, including celiac disease. Faulty brain control Eureka! The solution came when deep in discussion with my friend and colleague, Ron Harper, Professor of Neurobiology, UCLA. We were both struggling with the concept of multiple symptoms that needed to be explained. The answer appeared absurdly simple: disturbed "brain control". It suddenly seemed obvious—gluten could disturb the neural pathways of the body. Gluten was gradually damaging the brain and the nerves of susceptible people. It was the brain that was the common pathway for the manifestations of all of the gluten symptoms. So I set out to research what the world medical literature had to say. Is gluten a neurotoxin? I felt excited. I reviewed my patients in this new light—I began looking for a brain-grain connection. I began to see gluten as a neurotoxin—this could provide a universal model of gluten-sensitivity. This toxicity might act through inflammatory mechanisms or cross-reactivity with neurons. I began accumulating the evidence for my proposal that gluten-sensitivity is a brain and nerve disease. "Full Of It!" The concept of "Full of it" developed from the stories from my patients. I wrote my hypothesis down in a book now called Full of it! It refers to our diets being full of gluten; to the world being full of gluten-sensitive people; to the medical practitioners who are so skeptical of adverse reactions to gluten; to the enthusiasm of people who are feeling vibrant again on a gluten-free diet; and to those who are brimming with hope that the problem of gluten has now been recognized. Food allergy skeptics As a junior doctor I decided to formally research the food allergy phenomenon. I was awarded a research post and carried out the first comprehensive food allergy studies in New Zealand. I triumphantly demonstrated that food allergy was both a real entity and that it was common. But, to my disappointment, my colleagues were reluctant to believe me or my data. They professed a "disbelief" in food allergy. This surprised me as I had the research data. My next step was to conduct four more years of investigation of food allergy in Australia (at the Royal Childrens Hospital, Melbourne). This was a bigger and more elaborate study. My Doctoral Thesis (1982) based on this work is called: Food hypersensitivity in children: diagnostic approaches to milk and egg hypersensitivity. Since then I have continued my investigations into food allergy—but still today (25 years later) medical skepticism abounds. This "disbelief" is held despite the vast body of research describing food allergy. There seems to be an underlying unwillingness for doctors to consider food allergy as a possibility. Unfortunately, this also applies to gluten reactions. The shocking truth The shocking truth about gluten is that gluten foods are causing tremendous damage—but currently this is going mostly unrecognized. Unfortunately, gluten grains have become our staple diet. The quantity of gluten in our food supply has been steadily increasing. Yet worse, official Health Policies endorse gluten grains as the foundation of our food pyramid. Medics turn a blind eye Gluten is sapping the energy and wellbeing of countless millions. To date, the medical profession has turned a blind eye to glutens wider problems whilst focusing all of their attention on the narrow problem of celiac disease. A typical story I received emails like this every day: "Dr Ford, I have emailed you a number of times regarding our two children. I thought I should let you know that since going gluten free for the last three months, at last our son and daughter have put on some weight. If I had kept them on a normal gluten diet (which they recommended at the hospital) we would be still be having the headaches and sore tummies as well as the bad moods which our son would have. People just thought he was a naughty child, but now he is so different - we can talk to him without getting into any fights. I congratulate you for all your efforts on bringing gluten intolerance to the media and medical profession. More children and their families may find long awaited help. We have had to put up with this for seven years! At long last there is light at the end of the tunnel. Kind regards, Sue and Garry." Can gluten damage your brain? I believe that gluten was actually causing these two children to be sick. That is the explanation for their "naughty" behavior, their moods and their headaches. I postulate that gluten can damage your brain. I have come to this conclusion by the abundant circumstantial evidence from my observations of my patients who are gluten-sensitive. I have pondered the next questions: "Why do they have such an array of symptoms from gluten?" "Why do they recover so quickly when gluten is removed?" And "Why do they deteriorate so rapidly when only tiny amounts of gluten are eaten?" The concept of a brain/nerve disease can explain everything. The brain/nerve hypothesis "The symptoms from gluten occur through its action on the nervous system". I propose that gluten-sensitivity is a brain condition. Each and every organ in your body has some form of brain/nerve control. I propose that gluten can injure the delicate nervous networks that control your guts functions. A malfunction will subsequently lead to all of the gut symptoms that have so well been described. In addition, gluten can also directly affect brain function, which leads to the primary neurological symptoms that are so commonly seen with gluten-sensitivity. What is new? There are a number of new ideas that I put forward. These are based on circumstantial evidence. They produce a unifying theory of the symptoms that are attributed to gluten toxicity. A brain disease I consider that gluten-sensitivity is mostly a neurological problem. A major contribution to this debate is the realization that the brain has a central role in the expression of the symptoms that have, until now, been attributed to the local toxicity of gluten in the gut. A nerve disease I propose that gluten-sensitivity is a nerve disease. There is a gigantic network of nerves that controls every function that your gut is programmed to do. There are as many nerve cells in your gut as there are in your head! (about 25 billion nerve cells). I call it your tummy brain (or gut brain). Your tummy brain can be directly damaged by gluten reactions. This is the cause of so many sore tummies and bowel troubles. A wide spectrum of neurological manifestations For decades, there have been reports of unexplained brain and nerve symptoms which are associated with celiac disease. Although these associations have been described, there has been no universal mechanism proposed. However, if gluten is seen as a neurotoxin, then the explanation has been found. A very common disease Reactions to gluten have recently been documented to be extremely common. About one-in-ten people (as ascertained by blood donor studies) have high levels of gluten antibodies in their blood. My clinical studies have arrived at this same high number of gluten-sensitive people. Others have data to show that it is even more prevalent. Am I full if it? You might ask, "Is he full of it?" Yes, I am full of excitement and hope for the future. So many people can now be helped, if only this information can be widely distributed. I am full of ideas and full of enthusiasm. I hope that you are full of hope for your healthy and vibrant future. Tariq's story: "Dear Rodney, Thank you for your care and support of my family in regard to our allergies, gluten sensitivity and celiac disease that exists within that framework. My son Tariq, who is nearly 12 years old, has been a patient of yours over a number of years for his multiple food allergies. Tariq also suffers from dyslexia. Over the last several years Tariq has been becoming increasingly tired, lacking in energy and motivation, struggling with school work and constantly scratching due to his eczema and rashes covering all of his body. During this time, even though he has attended soccer training up to four times a week he somehow gained a lot of weight. Tariq was constantly grumpy and had low mood levels. Two months ago you diagnosed Tariq with gluten-sensitivity (his tTG 4; IgG-gliadin 86; IgA-gliadin 9). Tariq was extremely reluctant to go on a gluten free diet. But as the rest of the family had gone gluten-free—so he was forced also to become gluten-free. The changes that a gluten-free diet has evoked in Tariq have been astounding. His energy levels have increased, his skin has vastly improved, he has lost a lot of his excess weight (even though his appetite has increased) and he has shown improvement in his dyslexia. Tariq is not as grumpy as he was and his mood levels have improved. Tariq is now vigilant about gluten and can see the differences it has made to his life and the quality of it. Also, the other soccer parents have noticed a vast improvement in Tariq's energy levels and speed. His teacher has also noticed a big difference. Thanks again. Regards, Rosemary" Are you affected? The shocking truth is that gluten can damage your brain and that so many people are being encouraged to eat gluten-foods that might be steadily eroding their health and energy. If you have any lingering doubt about your own health, then I suggest that you check out the possibility of gluten-sensitivity.
-
Celiac.com 05/31/2021 - For people without celiac disease, does eating gluten have an impact on brain health, specifically on cognitive function? A recent study of nearly 14,000 non-celiac women at midlife revealed no statistical evidence of any association of long- or short-term gluten intake with cognitive function. More and more people are eating gluten-free for perceived health benefits that may not be real. It's true that cognitive impairment, sometimes called "brain fog," is a common symptom reported by many people before they are diagnosed with celiac disease. In those cases a gluten-free diet generally results in improvement of the symptoms. However, data are lacking in individuals without celiac disease. A recent study set out to "examine whether gluten intake is associated with cognitive function in women without celiac disease." Their study included US women who participated in the longitudinal, population-based Nurses’ Health Study II and had not previously or subsequently been diagnosed with celiac disease. Subjects answered a questionnaire that was used to cumulatively average gluten intake cycles prior to cognitive assessment. They then took a battery of tests on psychomotor speed and attention score, learning and working memory score, and global cognition score. They research team found no connection between long-term gluten intake and cognitive scores in middle-aged women without celiac disease. Their results, "do not support recommendations to restrict dietary gluten to maintain cognitive function in the absence of celiac disease or established gluten sensitivity." But how useful was the study? What did they actually measure? What did they actually show us? The study actually reveals very little, if anything. Celiac.com does not recommend a gluten-free diet for people who do not have celiac disease or gluten sensitivity, but we also do not oppose it. A properly structured gluten-free diet can be every bit as nutritious and health-promoting as a diet that contains gluten. However, we also do not agree with studies with conclusions that seem to be designed to scare people off of a gluten-free diet, or to soft-pedal a diet that contains wheat. The study does not say that there is no cognitive benefit to giving up gluten for people who do not have celiac disease or gluten intolerance, or that those without celiac disease might also benefit from a gluten-free diet. The benefits or harm of a gluten-free diet in people who are not gluten-free remains poorly studied. Even in people with celiac disease, the implications of a long-term gluten-free diet have not been well-studied, and plenty of studies make unproven nutritional assumptions about those implications based on scant data. We believe that each person must choose their diet for themselves, and that many folks without celiac disease may choose to eat gluten-free for reasons that make sense to them. Some may do so because they perceive themselves to think more clearly when they do not eat wheat. The problem, from our perspective is that the study basically says: We looked at a bunch of women who eat wheat and gluten in various quantities. Their brains seem fine. Nothing to see here. People concerned about a potential connection between brain function and wheat consumption deserve more than a study that says, in effect, "hey, plenty of women eat gluten, and whether they eat a lot or a little, their brain test results seem fine." Telling us that eating wheat does not seem to cause brain impairment in non-celiacs is helpful. It is. But it's only part of the picture. As far as we can see, none of these subjects had brain function tests when eating gluten compared with tests when they were gluten-free. Nor did the test compare women who ate wheat to similar women on a gluten-free diet (but really, what was needed here was the former, a comparison of the same group of people, perhaps tested when eating different gluten levels, then re-tested after a prolonged gluten-free diet). For all of the seemingly grand implications of the study, it really doesn't tell us much about brain function in people who eat gluten. It doesn't tell us if there are any benefits brain wise to giving up gluten. Look, it could be that giving up gluten has a negative impact on non-celiacs, but that remains unproven. We really need a more comprehensive and focused study to help tell us what, if any, impact gluten has on the cognitive function of non-celiacs, along with what benefits, if any, they might have when giving up gluten. Read more in JAMA Netw Open. 2021;4(5):e2113020 The research team included Yiqing Wang, PhD; Benjamin Lebwohl, MD, MS; Raaj Mehta, MD; et al Yin Cao, ScD, MPH; Peter H. R. Green, MD; Francine Grodstein, ScD; Manol Jovani, MD; Paul Lochhead, MBChB, PhD; Olivia I. Okereke, MD, MS; Laura Sampson, MS, RD; Walter C. Willett, MD, DrPH; Qi Sun, MD, ScD, MMS; Andrew T. Chan, MD, MPH. They are variously affiliated with the Clinical and Translational Epidemiology Unit, Massachusetts General Hospital, Harvard Medical School, Boston; the Division of Gastroenterology, Massachusetts General Hospital, Harvard Medical School, Boston; the Celiac Disease Center, Department of Medicine, Columbia University College of Physicians and Surgeons, New York, New York; the Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, New York; the Division of Public Health Sciences, Department of Surgery, Washington University in St Louis, St Louis, Missouri; the Division of Gastroenterology, Department of Medicine, Washington University in St Louis, St Louis, Missouri; the Rush Alzheimer’s Disease Center, Rush University Medical Center, Chicago, Illinois; the Department of Internal Medicine, Rush Medical College, Chicago, Illinois; the Division of Gastroenterology and Hepatology, Johns Hopkins Hospital, Baltimore, Maryland; the Channing Division of Network Medicine, Department of Medicine, Brigham and Women’s Hospital and Harvard Medical School, Boston, Massachusetts; the Department of Psychiatry, Massachusetts General Hospital and Harvard Medical School, Boston; the Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, Massachusetts; and the Department of Nutrition, Harvard T. H. Chan School of Public Health, Boston, Massachusetts.
- 4 comments
-
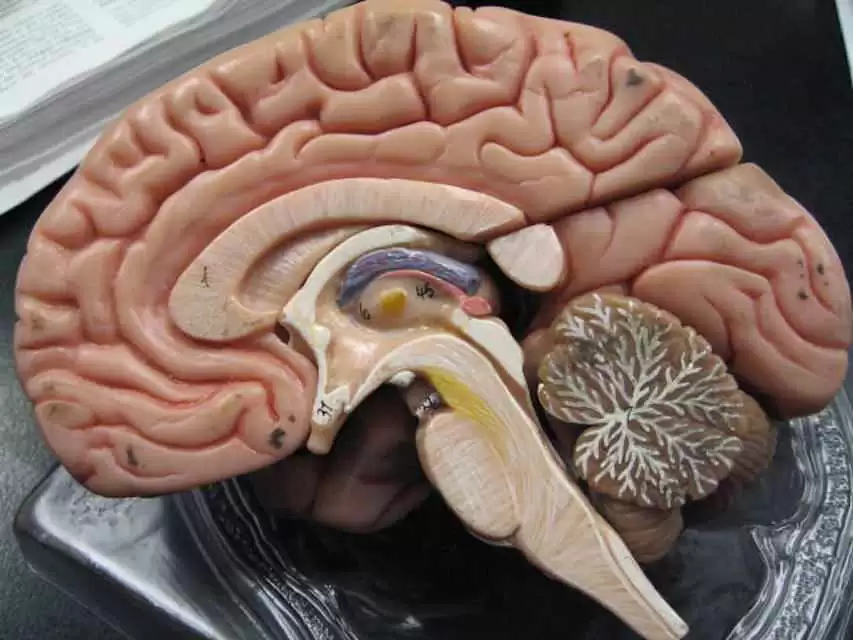
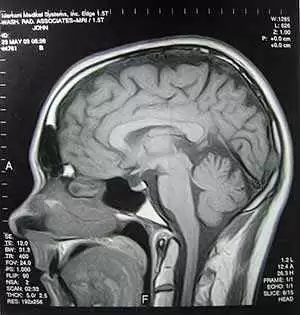
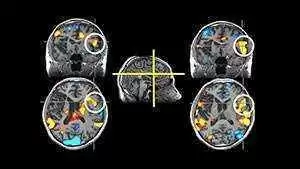
Celiac.com 02/01/2021 - Non-Celiac Gluten Sensitivity (NCGS) is poorly understood, particularly in terms of its neurological effects. A team of researchers looking into the matter first conducted a prospective postal survey to investigate its neurological presentation and symptom course. Based on the results of the survey, they conducted a brain MRI study to follow-up, and to note potential diagnostic biomarkers for future research. The research team included Iain D. Croall, Nigel Hoggard, Imran Aziz, Marios Hadjivassiliou, and David S. Sanders. They are variously affiliated with the Department of Infection, Immunity & Cardiovascular Disease, University of Sheffield/INSIGENO, Sheffield, United Kingdom; the Academic Unit of Gastroenterology, Royal Hallamshire Hospital, Sheffield Teaching Hospital NHS Foundation Trust, Sheffield, United Kingdom; and the Academic Departments of Neurosciences and Neuroradiology, Sheffield Teaching Hospitals NHS Trust, Sheffield, United Kingdom. The team recruited 125 patients with NCGS from a clinical center. Each patient completed a prospective postal questionnaire summarizing the symptoms, their severity and their course. The team used Chi-squared analysis to compare onset time to data from 224 celiac disease patients from the same centre. Five gluten-free respondents who self-reported brain fog then received MR brain imaging and questionnaires, both before and after a gluten challenge. The team recorded this “baseline” data, and looked for abnormalities. They then compared symptom severity and cerebral blood flow (CBF) both before and after the gluten challenge. Neurological symptoms included headaches in more than half of patients, brain fog in just under half, balance issues in about one-third of patients, and tingling in about 20%. Symptoms typically began with 90 minutes, and resolved within 48 hours. The pattern of symptom onset was similar to that seen in celiac patients. Extra-intestinal symptoms worsened by nearly 40% during a typical reaction. The combined survey and brain imaging analysis showed that non-trivial neurological symptoms are common, and may be studied within 2 hours following gluten ingestion. The team suggests that further brain imaging studies may help reveal physiological damage, and the physiological response to gluten. The researchers stress the need for diagnostic biomarkers for NCGS, and notes that there is limited research showing AGA is raised in NCGS patients compared to the general population This first-of-a-kind neuro-imaging study revealed numerous clinical variables, which may be helpful for further studying the pathophysiology of NCGS. The positivity rate in patients for this study was about 18%, compared to just under 13% for healthy volunteers, which is an insignificant difference. This generally supports previous literature showing that AGA is not a good way to diagnose typical NCGS. A better understanding of how gliadin positivity interacts with neurological outcomes may be helpful, as research indicates that these antibodies may harm the brain. Read more at PLOS.org
-
Celiac.com 01/25/2021 - What's the connection between celiac disease, and cognitive impairment? Does the connection change over time? Does following a gluten-free diet help reduce cognitive impairment? There really hasn't been much good study data on this so far. One of the main problems, according to researchers, previous reports of cognitive deficit in celiac disease often study widely variable groups of patients at multiple stages of the disease, and/or lack control data. To better understand the connection between cognitive impairment and celiac disease duration and gluten-free diet adherence, a team of researchers recently set out to examine groups of newly diagnosed and long-standing celiac disease patients. The research team included Iain D Croall, Claire Tooth, Annalena Venneri, Charlotte Poyser, David S Sanders, Nigel Hoggard and Marios Hadjivassiliou. They are variously affiliated with the Department of Neuroscience, the Department of Infection, Immunity & Cardiovascular Disease, and the Institute for Silico Medicine, at the University of Sheffield in Sheffield, UK; the Department of Psychological Services, Royal Hallamshire Hospital, STH, Sheffield, UK; the South West Yorkshire Partnership NHS Foundation Trust in Wakefield, UK; the Academic Unit of Gastroenterology, Royal Hallamshire Hospital, Sheffield Teaching Hospitals National Health Service Foundation Trust, Sheffield, UK; and the Department of Neurology, Royal Hallamshire Hospital, Sheffield Teaching Hospitals National Health Service Foundation Trust in Sheffield, UK. The team recruited 21 healthy control subjects, along with 19 newly diagnosed celiac patients (NCD) and 35 established celiac patients (ECD). Each participant took cognitive tests that established seven baseline domain scores. Patients also responded to SF-36 quality of life (QoL) questionnaires. The team then controlled for age, and compared data in between-group ANCOVAs with Tukey’s post-hoc test. The team then compared significant outcomes in the ECD group between fully gluten-free patients patients who not fully gluten-free diet, as defined by Biagi scores and blood tests. In visual, verbal, and memory tasks, the NCD and ECD groups underperformed relative to controls, by comparable measures. The ECD group only underperformed in visual-constructive tasks. In terms of QoL measures, the NCD patients reported lower vitality, while the ECD patients reported more bodily pain. Comparisons based on dietary adherence were non-significant. The team's findings confirm cognitive deficit in celiac patients, which seems to exist at the time of diagnosis, after which it seems to level off. While it seems that a gluten-free diet may be that cause of the leveling off, more research is needed to establish the degree to which this is true, and to what extent any further decline might result from ongoing gluten exposure. Read the team's paper entitled, Brain fog and non-coeliac gluten sensitivity: Proof of concept brain MRI pilot study, in Nutrients 2020, 12(7), 2028
-
Celiac.com 09/10/2020 - Brain fog is a state of mind that many celiacs experience, frequently in response to eating gluten, whether intentionally or otherwise. Sometimes we experience brain fog even when we are quite certain that we have not had any exposure to gluten. I am intimately familiar with this mental state, both when I have accidentally ingested gluten, and at times when I am sure I have not. At such times, my thinking becomes cloudy. I feel slightly detached from the world and my own emotions. I make mistakes that I would not normally make. I feel less alert, do not remember as well, become absent minded, require more sleep, sleep more soundly, and feel less rested when I awaken. I’m also a tad clumsier. I’m more easily confused. I find it more difficult to focus my attention and I sometimes feel mildly depressed. As I have mentioned in a previous article, brain fog is likely due to the convergence of a variety of contributing factors. My focus on that occasion was on exorphins—the morphine-like substances that come from partly digested gluten and dairy products and are sometimes called opioids. I also mentioned in that earlier article that the increased intestinal permeability found in active celiac disease, and now associated with the recently discovered zonulin, was a likely contributor. In susceptible individuals, gluten ingestion causes increased zonulin production. Zonulin widens the spaces between epithelial cells. Gluten’s contribution to brain fog is especially likely because zonulin not only causes a leaky gut—it also causes the same increase in permeability of epithelial junctions that form the blood brain barrier and which normally protects the brain from impurities in the bloodstream. Zonulin-induced permeability in the gut and the brain open a path for opioids to enter the circulation and then the brain. One feature of opioid activity is to alter blood flow patterns in the brain (1). Both the action of zonulin and opioid-induced impacts on brain perfusion combine to suggest that opioids derived from gluten and dairy products are likely to contribute to brain fog in celiac patients when they ingest gluten. Thus, gluten indirectly opens the gates to allow passage of gluten and dairy proteins through our protective barriers. However, food derived opioids are only one of many likely contributors to the brain fog that comes to us through a leaky gut. A leaky gut allows a mixture of foreign proteins and peptides to enter the bloodstream and the brain. Many of these foreign substances may well impact on brain function in various and unpredictable ways. The possibilities for negative impact on brain function are almost infinite. The Feingold Association has long held that a variety of synthetic food additives and colorings have a powerful impact on symptoms of attention deficit hyperactivity disorder (ADHD) in some individuals (https://www.feingold.org). Perhaps these individuals have undiagnosed celiac disease or gluten sensitivity and are over-producing zonulin, thus allowing these chemicals access to the bloodstream and the brain. The leaky gut is only one feature of celiac disease that may be at work in the symphony of interacting variables that result in our brain fog. Malabsorption may also play an important role here. Fat malabsorption, a long recognized feature of celiac disease, is often signaled by pale, floating stools and may be another contributor to brain fog. Our failure to absorb fats will include reduced absorption of essential fats. They are called “essential” because these fats are necessary to maintaining good health. Our bodies use essential fats to make cell membranes for neurones in the brain, to make a range of hormones that are involved in immune function, platelet aggregation, inflammation, and other important functions. Shortages of essential fatty acids have been reported in connection with neuro–degenerative diseases such as Alzheimer’s and depression (2). Mineral malabsorption is another important, well recognized feature of celiac disease. In fact, one common finding that often leads to the diagnosis of celiac disease is long term, treatment resistant, unexplained iron deficiency. Many untreated celiacs experience iron deficiency anemia. Some of us, despite the gluten-free diet, continue to experience challenges in achieving and maintaining iron repletion. Because most medical focus is on measuring hemoglobin, (which is the iron component of blood that distributes oxygen throughout the body) to identify iron deficiency, many more celiacs are likely to experience low iron stores and never be identified as long as their iron deficiency falls short of inducing anemia. A number of reports have identified reduced intellectual function in association with deficiencies in iron stores. These individuals are not anemic but they are likely to experience many of the symptoms of impaired intellectual function that are associated with iron deficiency. Since iron ions are critical to the hippocampal function of encoding memories, it is not surprising that other researchers report improved memory and cognition among iron deficient subjects following iron supplementation. Iron is also involved in some facets of immune function, mood, and impulse control. It is easy to see how subclinical iron deficiency may be a large factor in brain fog. To learn more about how iron deficiency can cause or contribute to poorer memory, lower intelligence, confusion, and despair, pick up a copy of my new book, “Get the Iron Edge”. More importantly, this book will guide you through a process that will help you to optimize your iron status, memory, and cognitive capacities. Of course, iron is not the only mineral that may play a role in brain fog. Magnesium and zinc are also important to healthy brain function, and magnesium supplementation alone has been shown to mitigate ADHD symptoms in some subjects (3). Malabsorption of any or all three of these minerals is likely to contribute to brain fog. By the time we finally get a diagnosis of celiac disease many of us try to improve our bone density by taking calcium supplements. Unfortunately, other minerals compete for the same transport mechanism that moves them across the intestinal barrier. Excessive calcium supplementation may swamp our transport capacity and result in induced deficiencies of other minerals that are important to brain function. Given all these data, brain fog is likely due to an unpredictable, unique, individualized mixture of contributing factors. Thus, each of us will experience brain fog a little differently. Gluten avoidance is the first step. For some, dairy avoidance is another important step. Balanced intake of minerals and other nutrients is also very important. The elevation to a state of alertness, optimum brain function, and a healthy brain will help us rise above our present difficulties, one step at a time. Sources: Gerra G, Calbiani B, Zaimovic A, Sartori R, Ugolotti G, Ippolito L, Delsignore R, Rustichelli P, Fontanesi B. Regional cerebral blood flow and comorbid diagnosis in abstinent opioid addicts. Psychiatry Res. 1998 Aug 26;83(2):117-26. Caramia G., The essential fatty acids omega-6 and omega-3: from their discovery to their use in therapapy. Minerva Pediatr. 2008 Apr;60(2):219-233. Starobrat-Hermelin B, Kozielec T. The effects of magnesium physiological supplementation on hyperactivity in children with attention deficit hyperactivity disorder (ADHD). Positive response to magnesium oral loading test. Magnes Res. 1997 Jun;10(2):149-56.
- 11 comments
-
Celiac.com 03/18/2020 - Researchers are still debating the extent to which celiac disease might cause brain damage. Some research has indicated that celiac disease can trigger changes to brain white matter, among other potential issues. A team of researchers recently set out to validate previous reports, we investigated the prevalence of neuropsychological dysfunction in persons with celiac disease included in the National UK Biobank, which contains experimental medical data from 500,000 adults in the United Kingdom. The research team included I.D. Croall, D.S. Sanders, M. Hadjivassiliou, and N. Hoggard. They are variously affiliated with the University of Sheffield, Academic Unit of Radiology; the Academic Unit of Gastroenterology; and the Department of Neurology at Royal Hallamshire Hospital, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom. The team matched 104 otherwise healthy celiac disease patients with 198 healthy individuals controls, closely matched for age, sex, level of education, body mass index, and diagnosis of hypertension. The researchers then compared scores from five cognitive tests, and multiple-choice responses to six questions about mental health, between groups using t test and χ2 analyses. Group analyses of magnetic resonance imaging brain data included a study of diffusion tensor imaging metrics (mean diffusivity, fractional anisotropy, radial diffusivity, axial diffusivity), voxel-based morphometry, and Mann-Whitney U comparisons of Fazekas grades. Compared to the control subjects, celiac disease patients showed substantially slower reaction times, and markedly higher rates of anxiety, depression, thoughts of self-harm, and health-related unhappiness. Tract-based spatial statistical analysis showed sharply higher axial diffusivity in widespread locations, which shows that white matter changes in brains of people with celiac disease. Voxel-based morphometry and Fazekas grade analyses were similar between the groups. Brain imaging shows that celiac disease patients suffer from cognitive deficit, changes to brain white matter, and reduced mental health, which support the notion that celiac disease is associated with both neurological and psychological features. Read more in Gastroenterology
- 2 comments
-
- brain
- brain damage
-
(and 5 more)
Tagged with:
-
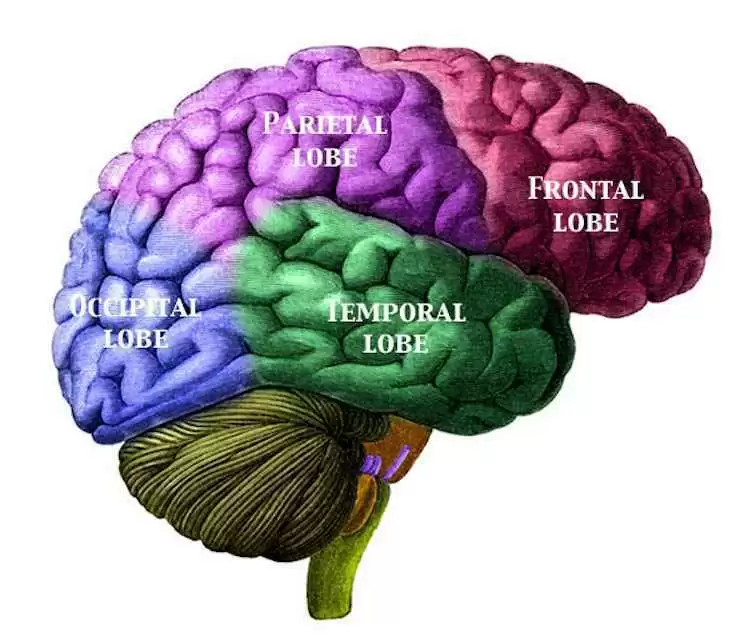
Celiac.com 03/12/2020 - A number of studies have shown a connection between migraine headaches and certain gastrointestinal (GI) disorders, like Helicobacter pylori infection, irritable bowel syndrome (IBS), and celiac disease. Is there a connection between migraine and the gut-brain axis? When researchers speak of the “gut-brain axis," they are describing a two-way relationship between the gastrointestinal system and the central nervous system. So far researchers don't currently have very good information about the ways in which the gut and the brain might interact in patients with migraine. A team of researchers recently set out to review and discuss the direct and indirect evidence for a connection between migraine headaches and the gut-brain axis. The research team included Mahsa Arzani, Soodeh Razeghi Jahromi, Zeinab Ghorbani, Fahimeh Vahabizad, Paolo Martelletti, Amir Ghaemi, Simona Sacco, Mansoureh Togha and on behalf of the School of Advanced Studies of the European Headache Federation (EHF-SAS). Prior research points to a number of potential factors, including inflammatory mediators (IL-1β, IL-6, IL-8, and TNF-α), gut microbiota profile, neuropeptides and serotonin pathway, stress hormones and nutritional substances. The current consensus is that neuropeptides, including CGRP, SP, VIP, NPY exert an antimicrobial impact on numerous strains of gut bacteria which are likely involved in the bidirectional relationship between the gut and the brain. Current research indicates that eliminating Helicobacter pylori bacteria, for example, can help reduce migraine headaches in people with Helicobacter pylori, and people with a long history of migraines and high headache frequency are much more likely to have IBS. Further, both IBS and migraine can change the makeup of gut bacteria, and so might influence gut-brain axis and inflammatory response. Migraine headaches have also been associated with celiac disease, and doctors should keep this in mind, especially in migraine patients whose brain imaging shows occipital and parieto-occipital calcification. Studies show that a gluten-free diet can help reduce migraine frequency in such patients. Many researchers believe that migraine headaches can be improved by diets that support healthy gut microbiota and gut-brain axis, including a low glycemic diet, higher fiber intake, supplemental vitamin D, omega-3 and probiotics, as well as weight loss and dietary plans for overweight and obese patients. Read more in the Journal of Headache and Pain volume 21, Article number: 15 (2020) The researchers in this study are variously affiliated with the Headache Department, Iranian Center of Neurological Research, Neuroscience Institute, Tehran University of Medical Sciences, Tehran, Iran; the Headache Department, Neurology Ward, Sina University Hospital, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran; the Cardiovascular Diseases Research Center, Department of Cardiology, Heshmat Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran; the Department of Clinical Nutrition and Dietetics, Faculty of Nutrition and Food Technology, Shahid Beheshti University of Medical Sciences, Tehran, Iran; the Neuroscience section of the Department of Applied Clinical Sciences and Biotechnology, University of L’Aquila, L’Aquila, Italy; the Department of Virology, Pasteur Institute of Iran, Tehran, Iran; and the Department of Clinical and Molecular Medicine, Sapienza University of Rome, Rome, Italy.
-
I have been gluten free since Feb 2012. Many of my symptoms have subsided, but there are some alarming ones that have maintained and persisted. To the extent I had gone back to the dr. b/c I believed them to be something separate from the celiac disease. Now I'm not sure. The dr.s have no clue and I believe they are ready to send me for a psych consult. The neurologist alluded to a conversion disorder...psychosomatic etc.....I know that is not it. My celiac dr had put me on the Fasano diet, b/c I am so sensitive to gluten, and the 3 accidental exposures I have had have laid me out for 5 weeks at a time. I have been doing better since the Fasano diet, but these things have stood out glaringly. I have persisting dizziness and lightheadedness. Fatigue is severe. I wake up fine, and do as much as I can before I am a waste case for the rest of the day. That is between 6-9 am... and then I am exhausted for the rest of the day. If I rest, I can get a little energy back and it is gone quickly I feel like a cell phone that can't hold a charge. I have episodes when I am walking, I start to slow down, balance is off...weakness takes over, I can barely walk, or hold a conversation. My face goes grey, my eyes are sunken. I need assistance getting into a chair. It takes a few hours before this passes. I feel like I am trapped in my body. Sometimes this comes with a sensation of a shivering or fluttering sensation in my brain. It is very concerning. However, the neurologist has never heard of this before. (thankfuly my celiac doc told me yesterday that he has had patients with the same fluttering....No other dr!) When these episodes pass, they leave me exhausted for hours to days. Please can someone advise if they have had some of the same symptoms? My ANA is high, 640 My ttg is around 29. I live in 100% gluten free house. Including all of my beauty products.
-
Celiac.com 09/04/2017 - Researchers think they may have discovered an important connection between diet and dementia. For the first time, they have tied a specific dietary pattern to blood markers for inflammation. In addition, they showed that elderly adults who followed a certain dietary pattern had reduced brain gray matter volume, and worse visuospatial cognitive function. The team found that “people who consume less omega 3, less calcium, vitamin E, vitamin D, and vitamin B5 and B2 have more inflammatory biomarkers," study investigator Yian Gu, PhD, Columbia University and the Taub Institute for Research on Alzheimer's Disease and the Aging Brain, New York City, told reporters. Some studies have linked chronic inflammation to an increased risk for AD. But, until now, no research addressed whether diet affects brain and cognitive health by modulating inflammation. "No study has formally tested whether the relationship of diet with cognition, or with the brain, is actually because of inflammation," said Dr Gu. Dr. Gu’s research team conducted a new cross-sectional study on 330 elderly adults from the Washington Heights–Inwood Community Aging Project imaging study. Researchers conducted structural MRI scans on these patients, and measured levels of the inflammatory biomarkers CRP and IL6. Each participant responded to a 61-item questionnaire about food and nutrient intake over the past year. The researchers used the results to craft a statistical model of the inflammation-related nutrient pattern (INP). These new findings suggest that dietary and/or medical treatments that reduce inflammatory markers may be helpful. Results of their study were presented at the Alzheimer's Association International Conference (AAIC) 2017. Source: Alzheimer's Association International Conference (AAIC) 2017
-
- aging
- alzheimer's
-
(and 5 more)
Tagged with:
-
PEDIATRICS Vol. 108 No. 2 August 2001, p. e21 Kieslich M, Errazuriz G, Posselt HG, Moeller-Hartmann W, Zanella F, Boehles H. Departments of Pediatrics, Johann Wolfgang Goethe University, Frankfurt/Main, Germany. Celiac.com 08/24/2001 - It is well known that celiac disease causes destruction of the villi in the small intestine that results in malabsorption of nutrients in affected individuals. There is solid evidence that additional neurological complications can result, such as epilepsy, possibly associated with occipital calcifications or folate deficiency and cerebellar ataxia. An increase in brain white-matter lesions has been reported in patients with Crohn disease and ulcerative colitis, but until now, not in patients with celiac disease. A recent study published in the August 2, 2001 issue of Pediatrics has now demonstrated a similar increase of these lesions in patients with celiac disease. The study was carried out by Dr. Kieslich and colleagues of the Departments of Pediatrics, Johann Wolfgang Goethe University, Frankfurt/Main, Germany, on 75 biopsy-proven celiac disease patients who were on a gluten-free diet. Most of the patients in the study were between 2.8 and 24.2 years old, and the mean age was 11.6 years. All of the patients underwent prospectively clinical neurological examinations, laboratory investigations, electroencephalography, computed tomography, and magnetic resonance imaging. According to the study the mean period of gluten exposure was 2.4 years, although it was likely longer as recent studies have shown that many celiacs are asymptomatic for many years before damage occurs that is severe enough to cause obvious symptoms. The researchers found that ten of the patients had neurological manifestations such as febrile seizures, single generalized seizures, mild ataxia, and muscular hypotonia with retarded motor development, although no folate deficiencies were found. Further, the hippocampal regions appeared normal, and no cerebral calcifications were found, however, the MRI results showed unilateral and bilateral T2-hyperintensive white-matter lesions in 15 patients (20%). According to the research, there does not appear to be a relationship between these lesions and dietary compliance or neurological or electroencephalographic abnormalities. The researchers conclude that focal white-matter lesions in the brain may represent an extra-intestinal manifestation of celiac disease. They theorize that the lesions may be the result of a decreased blood supply caused by the constriction or obstruction of blood vessels due to inflammation, or caused by the destruction of the nerve fiber due to inflammation. Further, children with white-matter lesions, even if they do not have intestinal symptoms, should be tested for celiac disease. Last, more research needs to be done on people celiac disease of all ages to develop a proper predictive value, and to discover the exact cause of the lesions.
- 6 comments
-
Celiac.com 06/12/2017 - Previously, Transcranial Magnetic Stimulation in de novo celiac disease patients has signaled an imbalance in the excitability of cortical facilitatory and inhibitory circuits. Researchers have reported that, after about of 16 months on a gluten-free diet, patients experience a global increase of cortical excitability, which suggests some kind of compensation for disease progression, likely mediated by glutamate. To better assess these finding, a team of researchers recently conducted cross-sectional evaluation of the changes in cortical excitability to TMS after a much longer gluten-free diet. The research team included M. Pennisi, G. Lanza, M. Cantone, R. Ricceri, R. Ferri, C.C. D’Agate, G. Pennisi, V. Di Lazzaro, and R. Bella. They are variously affiliated with the Spinal Unit, Emergency Hospital "Cannizzaro", Catania, Italy, the Department of Neurology IC, I.R.C.C.S. "Oasi Maria SS.", Troina, Enna, Italy, the Department of Medical and Surgical Sciences and Advanced Technologies, Section of Neurosciences, University of Catania, Catania, Italy, the Gastroenterology and Endoscopy Unit, University of Catania, Catania, Italy, the Department "Specialità Medico-Chirurgiche,” University of Catania, Catania, Italy, and the Institute of Neurology, Campus Bio-Medico University, Rome, Italy. For their study, the team enrolled twenty patients who had followed an adequate gluten-free diet for about 8.35 years, on average. They then compared the results with twenty de novo patients, and twenty more healthy controls. The team measured Transcranial Magnetic Stimulation, recorded from the first dorsal interosseous muscle of the dominant hand, as follows: resting motor threshold, cortical silent period, motor evoked potentials, central motor conduction time, mean short-latency intracortical inhibition and intracortical facilitation. De novo patients showed a shorter cortical silent period, while responses for gluten-free diet participants were similar to controls. Regardless of diet, all celiac patients showed a significantly smaller amplitude of motor response than did control subjects, Again, without regard to diet, all celiac patients showed a statistically significant decrease of mean short-latency intracortical inhibition and enhancement of intracortical facilitation with respect to controls. The team also observed that gluten-free celiac patients showed more intracortical facilitation compared to non-gluten-free patients. Neurological examination and celiac disease-related antibodies were both negative. This study showed that a gluten-free diet helps to mitigate the electrocortical changes associated with celiac disease. Even so, in many patients, an intracortical synaptic dysfunction, mostly involving excitatory and inhibitory interneurons within the motor cortex, may persist. The calls for further investigation into the clinical significance of subtle neurophysiological changes in celiac disease. Source: PLoS One. 2017 May 10;12(5):e0177560. doi: 10.1371/journal.pone.0177560. eCollection 2017.
- 1 comment
-
- activity
- associated
- (and 12 more)
-
Celiac.com 12/01/2016 - Alcohol-related cerebellar degeneration is one of the most common forms of acquired cerebellar ataxia. Researchers still do not understand the exactly how alcohol damages the cerebellum. Very little study has been done on auto-reactive immune mediated mechanisms as a possible contributor. Recently, a team of researchers set out to investigate the potential role of alcohol-induced immune mediated cerebellar degeneration. The research team included Priya D. Shanmugarajah, Nigel Hoggard, Stuart Currie, Daniel P. Aeschlimann, Pascale C. Aeschlimann, Dermot C. Gleeson, Mohammed Karajeh, Nicola Woodroofe, Richard A. Grünewald and Marios Hadjivassiliou. They are variously associated with the National Blood Service Sheffield, UK; Department of Immunology, Northern General Hospital, Sheffield, UK and Academic Unit of Radiology, University of Sheffield, UK. For their study, the team recruited patients with ataxia and a history of heavy alcohol use from the Ataxia and Hepatology tertiary clinics at Sheffield Teaching Hospitals NHS Trust. The team determined the pattern of cerebellar involvement both on clinical (SARA score) and imaging (MRI volumetry and MR spectroscopy) parameters. They also evaluated HLA genotyping, serological markers for gluten-related disorders and serological reactivity on rat cerebellar tissue using indirect immunohistochemistry. In all, the team studied thirty-eight patients with ataxia, which negatively impacted the gait in 97% of patients, and stance and heel-shin slide in 89% of patients. The team used MRI volumetric and spectroscopy techniques to show significant structural, volumetric and functional deficiencies of the cerebellum with particular involvement of the cerebellar vermis. They found circulating anti-gliadin antibodies in 34% of patients, compared with 12% of healthy controls. They found antibodies to transglutaminase 6 (TG6) in 39% of patients, but only in 4% of healthy control subjects. Using immunohistochemistry, they found Purkinje cell and/or granular layer reactivity in 71% of patient sera. Alcohol induced tissue injury to the CNS leading to cerebellar degeneration may also involve immune mediated mechanisms, including sensitization to gluten. The team is calling for role of gluten in ataxia to be studied further, to determine the exact mechanism, and the extent of gluten's impact on ataxia patients. Source: Cerebellum & Ataxias 2016, 3:17. DOI: 10.1186/s40673-016-0055-1
-
- alcohol-related
- brain
-
(and 2 more)
Tagged with:
-
Celiac.com 09/17/2012 - Many aspects of celiac disease simply have not been well studied, so they remain poorly understood. For example, researchers have not done enough study on people with celiac disease to understand if they show any readily available serological markers of neurological disease. To better understand this issue, a research team recently assessed the amount of brain abnormality in patients with celiac disease, along with looking into MR imaging sequences as biomarkers for neurological dysfunction. The study team included S. Currie, M. Hadjivassiliou, M.J. Clark, D.S. Sanders, I.D. Wilkinson, P.D. Griffiths, and N. Hoggard, of the Academic Unit of Radiology at University of Sheffield, Royal Hallamshire Hospital, in Sheffield, UK. For their study, they conducted a retrospective examination of a consecutive group of 33 patients with biopsy proven celiac disease, who had been referred for neurological opinion. The group ranged in age from 19 to 64 years old, with an average of 44±13 years. Researchers divided the group into subgroups based on their main neurological complaints of balance disturbance, headache and sensory loss. They used 3T MR to evaluate variations in brain grey matter density, cerebellar volume, cerebellar neurochemistry and white matter abnormalities (WMAs) between celiac patients and control subjects. The results showed that the celiac patients had a significantly lower cerebellar volume than did control subjects. Celiac patients had 6.9±0.7% of total intracranial volume, compared with 7.4±0.9% for control subjects (p<0.05). Celiac patients also showed significantly less grey matter density in multiple brain regions, both above and below the tentorium cerebelli, compared with the control subjects (p<0.05). The data showed that 12 (36%) patients demonstrated WMAs unexpected for the patient's age, with the highest incidence occurring in the headache subgroup. This group of patients averaged nearly double the number of WMAs per MR imaging session than the subgroup with balance disturbance, and six times more than the subgroup with sensory loss. The MR images of celiac patients who have neurological symptoms show significant brain abnormality on MR imaging, which means that MR imaging may serve as valuable biomarkers of disease in celiac patients. Source: J Neurol Neurosurg Psychiatry. 2012 Aug 20.
- 6 comments
-
- abnormalities
- brain
-
(and 6 more)
Tagged with:
-
Celiac.com 03/20/2014 - No one wants a brain disease, and some recent books on the effects of gluten-free diets are suggesting that a gluten-free diet might actually protect you from brain diseases. One such book is Grain Brain: The Surprising Truth About Wheat, Carbs, and Sugar — Your Brain's Silent Killers, by David Perlmutter, M.D., a practicing neurologist. Symptoms of celiac disease are known to include intestinal difficulties associated with an adverse immunological response triggered by gluten. This response, which leads to inflammation in the gut, can happen elsewhere in the body too. According to Perlmutter, inflammation is at the root of many diseases and complications, including, brain decay. According to Perlmutter, gluten can lead to inflammation in the brain, which he believes leads to conditions like dementia and Alzheimer's. Perlmutter says that gluten, by triggering the immune system, causes inflammation in the brain, which promotes the brain's glycation by circulating blood sugar. Gram for gram, wheat raises blood sugar levels more than sugar itself. Perlmutter encourages strong dietary changes that have drawn some criticism. Specifically, he has recommended an intake of 60 or fewer grams of carbohydrate per day. Some point out potential negative health consequences of a high-fat, low-carb diet, both in healthy people and for those with specific conditions, like adrenal or thyroid issues. However, Perlmutter's take on brain glycation, in which gluten triggers an immune response in certain people, contributing to inflammation, and to inflammatory disease, such as diabetes and Alzheimer's, may have some foundation. Perlmutter is a reputable neurologist, so his opinion and insight go beyond anecdotal evidence and speculation. It will be interesting to see how much of his perspective is borne out by science. Meantime, Perlmutter certainly makes for interesting, thought-provoking reading. What's your experience? Has going gluten-free made an impact on your brain function and awareness? Read more at: Celiac.com and at Medical Express.com.
-
Celiac.com 10/02/2014 - Most people have heard about kidney stones, or gall stones, due to calcium build up. Others may know that calcium deposits can affect the heart, and even the brain. However, until now, it was not known that, in certain cases, celiac disease can trigger calcification in the brain. Doctors examining a 24-year-old Brazilian man with a history of recurrent headaches revealed a rare condition known as the CEC syndrome, a combination of celiac disease, epilepsy, and cerebral calcification, commonly referred to as ‘brain stones.’ The man had been treated for migraine headaches over a period of 10 years, with little response. Standard blood tests showed a mildly decreased folate level (2.2 ng per milliliter [5.0 nmol per liter]; compared to a reference range of 3.1 to 17.5 ng per milliliter [7.0 to 39.0 nmol per liter]). A computed tomographic scan of his brain showed bilateral occipital calcification, or ‘brain stones.’ Laboratory testing showed normal cerebrospinal fluid and elevated levels of serum IgA antitransglutaminase antibodies (45 U per milliliter). The man received an endoscopy, and his jejunal-biopsy specimen showed crypt hyperplasia, villous atrophy of the jejunal mucosa, and an increased number of intraepithelial lymphocytes; all classic indications of celiac disease. Doctors started treatment with a gluten-free diet, folic acid supplementation, and carbamazepine, and the patient's symptoms disappeared and his condition improved. In this case, there was no indication that the man suffered from epilepsy. The likely culprit is folate malabsorption, because cerebral calcification has been seen in other conditions related to folate deficiency, such as treatment with methotrexate, congenital folate malabsorption, and the Sturge–Weber syndrome. So, physicians treating celiac patients with low folate levels may want to keep an eye out for any indications of cerebral calcification, and to make sure that patients receive appropriate supplemental folate. Source: New England Journal of Medicine
-
Can going gluten-free boost your brain power? Dr. David Perlmutter, neurologist, and author of Grain Brain, published by Little Brown and Company, thinks there's a good reason why we may want to go gluten-free a try. Dr. Perlmutter gives three basic reasons for people to avoid gluten in their diets: 1. Avoiding Gluten Reduces Brain Degredation While the majority of individuals suffering from gluten sensitivity experience intestinal discomfort, Perlmutter says an increasing number are experiencing neurological challenges including difficulty staying on task, poor memory function, brain fog and severe headaches that result from inflammation; a common reaction to gluten in those with a sensitivity to the protein. "The brain responds really badly to inflammation," says Perlmutter. Another reason for the loss of cognitive function is that some of our brain proteins look similar to gliadin, a protein found in gluten-containing foods, says Perlmutter. Anti-gliadin antibodies produced by individuals with gluten sensitivity can't tell the difference between these two proteins and eat up the brain proteins that are required for normal cognitive function. Going gluten-free likely won't make you any smarter, but Perlmutter says it may help protect your cognitive function from weakening. 2. Avoiding Gluten Strengthens the Immune system Perlmutter says gluten stimulates the cells of the intestine to secrete a protein called zonulin, which regulates the absorbency of the intestine. The increased production of zonulin erodes the walls of the intestine, allowing various proteins to leave the gut and enter our blood stream. This poses many challenges to the immune system, weakening our ability to fight off diseases. According to Perlmutter, avoiding gluten, strengthens the immune system. A healthy immune system is essential for optimal brain function. 3. Avoiding Gluten Improves Brain Fueling According to Perlmutter, a healthy brain needs generous amounts of healthy fats. Because our brains are 70 percent fat, food loaded with carbs and sugar rob them of the fuel they need to function well. In place of gluten and carb-laden breakfast food such as a bagel and orange juice, Perlmutter recommends a high-fat breakfast rich in omega 3 fatty acids that protect the brain, including eggs, nuts, seeds or avocado. The verdict is out as to whether or not people without gluten sensitivity experience the same cognitive decline as those with gluten sensitivity, However, Perlmutter urges anyone experiencing poor cognitive function, chronic headaches or inflammatory illnesses, including joint or abdominal pain, to avoid gluten for few months and see if there is any positive change. What do you think? Has going gluten-free helped improve your brain function, along with your other celiac symptoms? Share your comments below. Source: Entrepreneur
-
Celiac.com 09/13/2008 - In the last two decades, research has begun to focus on gluten’s effects on the brain, including associations with Autism Spectrum Disorder (ASD) and Attention Deficit Hyperactivity Disorder (ADHD). Celiac disease itself occurs no more frequently in children with ASD than in neurologically normal children, but it appears there are other reasons to consider excluding gluten from the diet. “Mal-digestion of dietary proteins, particularly casein (from cow’s milk) and gluten-containing foods, produces small peptides (amino acid sequences) that may function as opioids”. This is what is known as “The Peptide Theory”, also called “The Opioid Excess Theory”. What this means is that incomplete digestion of specific foods allows the remaining small protein fragments, called peptides, to pass through the gut wall into the bloodstream. Peptides are tiny, but children affected by dietary peptides often have what is termed a “leaky gut”, or a gut that is in some way damaged and unable to fully perform its protective function. In children (and adults) with ASD, gluten breaks down into a peptide called gliado-morphin, and casein breaks down into a peptide called caso-morphin. Eventually these peptides are thought to bind to opioid receptors in the brain, where they are perceived by the body as morphine-like substances. It is this morphine-like or narcotic-like effect that causes many of the typical behaviors associated with ASD. These behaviors can include sensory problems, lack of eye contact, self-stimulation, and altered pain threshold, among others. Repeated exposure to gluten and casein causes a condition similar to opiate addiction - children with this condition often crave the very thing that is causing their problems; consequently, sudden, complete elimination of gluten and casein from the diet can cause withdrawal symptoms. The discovery of caso-morphin and gliado-morphin in the urine of autism patients may be strong supporting evidence for the peptide theory. Many parents and practitioners believe in also excluding “excitotoxins” such as dyes, food-additives, MSG, and sweeteners containing aspartame from a child’s diet (Excito-toxins are also suspected to play a role in Attention Deficit Disorder (ADD) and ADHD). Complete allergy testing, as well as testing for Candida (systemic fungal overload) is also recommended. A good time to do this is after your child has improved somewhat and is stabilized on a gluten-and-casein-free diet. You will know when your child is ready to move on to the next level. Careful treatment by a clinician skilled in working with special-needs children is essential, and certain types of body work such as IMT (Integrated Manual Therapy) can be important in tackling these challenges. Patience is important – it may take only a few days for milk-derived peptides to leave the body, but gluten-derived peptides can persist for several more months. Discuss keeping a food diary, and appropriate timelines for an individual child’s response to a special diet, with your practitioner. For those skeptical of altering a child’s diet to effect positive behavioral and neurological changes, there are some small clinical studies (and more needed) and thousands of anecdotal reports from grateful parents whose children have demonstrated spectacular and lasting changes from a gluten and-casein-free diet. That is not to say that the diet is completely “curative”, or that an unrestricted diet that includes gluten and casein “causes” Autism (which may be due to a variety of factors). Here is a thoughtful passage from Marilyn LeBreton’s book, “Diet Intervention and Autism” : “I knew I had to give the diet a go…..It seemed the most sensible route of treatment to try with him (her young son “Jack”). It did not involve giving him drugs, nor did it involve very intensive behavioral treatments…” In another passage she writes, “I knew about the (Gluten-free/Casein-free) diet for six months before I implemented it with my own son…I now bitterly regret these wasted months.” A CDC report issued in 2006 estimates 300,000 school-age U.S. children have Autism, a staggering statistic with wide educational and social implications.16 In the book, “Autism Spectrum Disorders”, Chantal Sicile-Kira relates that “with a diagnosis rate as high as 1 in 166, and in some places 1 in 150, everyone knows someone whose life is touched by autism.” For families directly affected by Autism Spectrum Disorder, attending a support group is a very good idea. Gluten ataxia is a rarely diagnosed and frequently overlooked condition* responsible for a set of symptoms usually labeled “sporadic idiopathic ataxia” - meaning that symptoms arise spontaneously and sporadically, and cannot be traced to any definitive cause. This condition usually occurs in adults and seniors and manifests in a variety of neurological symptoms: severe headaches, lack of muscle coordination, drooping eyelids, gait and balance disturbances, drooling, numbness, tingling, and weakness in the extremities, and problems with speech and word-finding. Usually the client is worked up for M.S., Parkinson’s, ALS, and other neurological disorders but is negative. Repeated MRI scans cannot pinpoint the exact cause of these symptoms, which can be severe and debilitating. Once the diagnosis “sporadic idiopathic ataxia” is given, they are offered supportive but not curative treatment. Fortunately, some patients are able to find a neurologist who specializes in difficult diagnoses. Often the diagnosis of gluten ataxia is only made when the patient reveals a past positive test for gluten intolerance, family history of celiac disease, or a history of gastrointestinal problems like irritable bowel syndrome or colitis. In the case of gluten ataxia, gluten cannot be properly digested in the body, and certain protein deposits develop in the brain, causing changes that affect the neurological system. Complete avoidance of gluten in addition to supportive physical and cognitive therapies can sometimes reverse many of the patient’s symptoms, but complete recovery is not always possible. A very poignant and thought-provoking article on gluten ataxia was published in “Living Without”, Spring, 2007, and it is well worth reading if you or someone in your family is experiencing problems with movement, strength, or balance. Peripheral neuropathy, common among diabetics, can also be related to gluten intolerance. Neuropathy results in painful or numb extremities, including the feet, so it impairs mobility and increases the risk of falls. It is similar to the “pins and needles” feeling one gets from siftting on the knees too long, only much more intense and constant. The pain can be so severe that it is necessary to take pain medications. In a book unrelated to gluten intolerance, John A. Seneff explains that the amino acid Acetyl-L-Carnitine may have protective and restorative effects on the nerves involved in this disorder. Interestingly, patients with celiac disease and gluten intolerance often show low levels of L-Carnitine and benefit from supplementation . In addition to the above conditions, many gluten-sensitive individuals report mental sluggishness, “foggy thinking”, and forgetfulness. I’m sure we all would like to find a reason for our occasional memory lapses, but in some people, gluten-sensitivity may induce cognitive symptoms that impair job performance, relationships, driving ability, and general safety - these cases require evaluation by a physician. Gluten sensitivity as a factor in the development of schizophrenia has been substantiated by a number of epidemiological and clinical studies. It has also been noted that this psychiatric disorder rarely occurs in countries where wheat and other gluten grains are not often consumed. I believe that we will find that more and more neurological conditions are related to impaired digestion of gluten from grains, and casein from dairy products. If you or a loved one have any neurological symptoms, especially symptoms not attributable to any other cause, it would be worthwhile to investigate gluten and or casein sensitivity with an experienced medical practitioner. In my experience, a naturopath or MD/ND is the best place to start. Of course, it is always important to see your medical practitioner to track developmental milestones and growth patterns in infants and young children. * Sporadic Idiopathic Ataxia accounts for nearly 74% of all patients who have ataxia, and of that 74%, nearly 41% have positive antibodies indicating gluten sensitivity (Lieberman, The Gluten Connection, 2007.)
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8-M):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8-M):