-
Welcome to Celiac.com!
You have found your celiac tribe! Join us and ask questions in our forum, share your story, and connect with others.
-
Celiac.com Sponsor (A1):
Celiac.com Sponsor (A1-M):
-
Get Celiac.com Updates:Support Celiac.com!
Search the Community
Showing results for tags 'causes'.
-
Celiac.com 04/17/2024 - Maintaining optimal health involves ensuring that our bodies receive essential nutrients, including magnesium, a vital mineral crucial for various bodily functions. Magnesium deficiency can arise from various factors, including medical conditions like celiac disease, poor absorption, increased need, or excessive elimination. Understanding the signs, causes, and remedies for magnesium deficiency is essential for overall well-being. Identifying Magnesium Deficiency Symptoms Magnesium deficiency symptoms may initially manifest subtly, including muscle spasms, fatigue, decreased appetite, and nausea. However, if left unaddressed, more severe effects such as abnormal heart rhythm, seizures, anxiety, and personality changes may occur. As these symptoms overlap with those of other health conditions, a blood test from a medical provider is crucial to confirm magnesium deficiency accurately. Causes of Magnesium Deficiency Malabsorption due to gastrointestinal conditions like celiac disease or inflammatory bowel disease can hinder magnesium absorption. Additionally, certain medications and increased magnesium needs, such as during pregnancy or in athletes, can contribute to deficiency. Factors that affect magnesium elimination, like alcohol consumption or medical conditions such as kidney disease, also play a role. The Role of Magnesium in the Body Magnesium plays a vital role in numerous bodily processes, including muscle and nerve function, heart rhythm maintenance, blood sugar control, bone health, and blood pressure regulation. Furthermore, magnesium influences hormone balance related to sleep, circadian rhythm, and mood regulation, and can alleviate conditions like migraine headaches. Sources of Magnesium To address magnesium deficiency, both oral supplements and magnesium-rich foods can be beneficial. Supplements, such as magnesium glycinate or magnesium citrate, offer an easily accessible solution, although they may cause mild gastrointestinal side effects. Alternatively, incorporating magnesium-rich foods like pumpkin seeds, almonds, spinach, soy, and black beans into one's diet can help meet daily magnesium requirements. Frequently Asked Questions About Magnesium What is the best magnesium supplement? Magnesium glycinate and magnesium citrate are generally well-tolerated forms of magnesium supplements. Are there supplements best avoided when taking magnesium? Calcium supplements should be taken separately from magnesium to prevent competition for absorption. What medications interfere with magnesium: Certain medications, including proton pump inhibitors, antibiotics, diuretics, and chemotherapy drugs, can hinder magnesium absorption and should be managed accordingly. In conclusion, recognizing the signs of magnesium deficiency, understanding its causes, and knowing how to address it through supplementation or dietary adjustments are essential for maintaining optimal health. Consulting healthcare providers for accurate diagnosis and personalized treatment plans is vital in managing magnesium deficiency effectively. This article is not intended to offer medical advice, and is for informational purposes only. Please consult a medical professional for personal advice on celiac disease, magnesium deficiency, and/or any other medical concern.
-
- absorption
- causes
- (and 8 more)
-

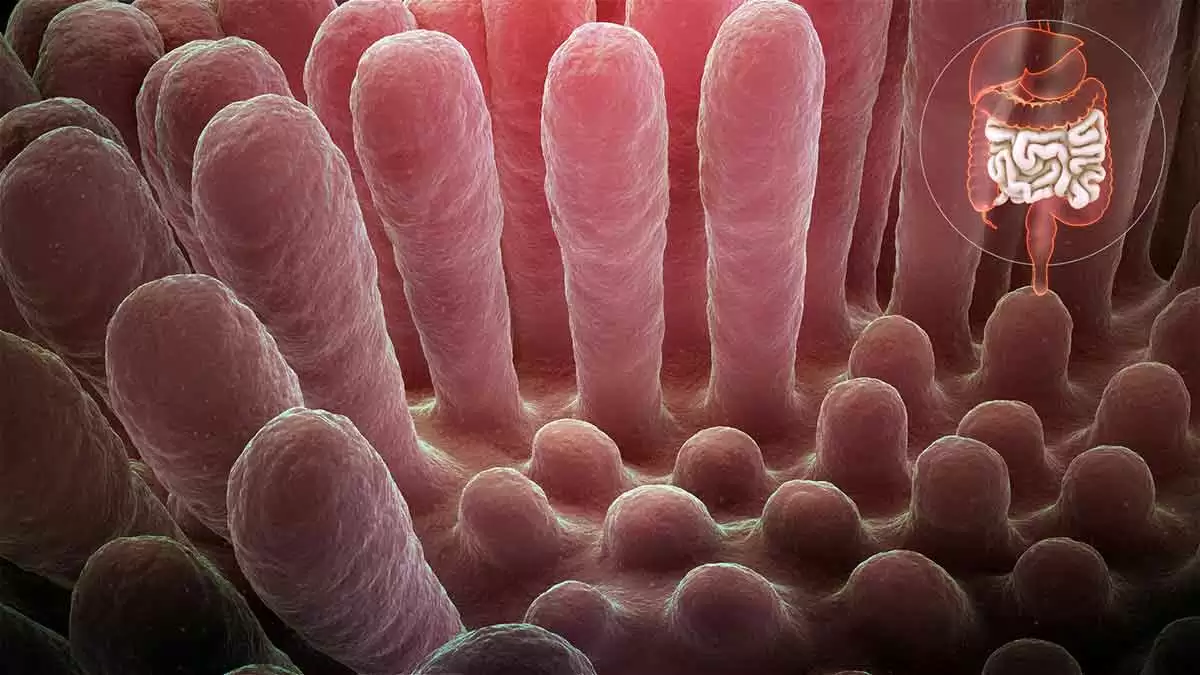
Exploring Other Causes of Villous Atrophy Beyond Celiac Disease
Scott Adams posted an article in Spring 2024 Issue
Celiac.com 02/10/2024 - Villous atrophy, a condition marked by the blunting or flattening of the microscopic structures called villi in the small intestine, is most commonly associated with celiac disease. However, emerging research and clinical observations have unveiled a spectrum of diverse conditions beyond celiac disease that can lead to villous atrophy. This article explores the lesser-known contributors to villous atrophy, shedding light on various health conditions that may present with similar histological changes in the small intestine. While celiac disease remains a prominent cause, understanding these alternative pathways to villous atrophy is crucial for accurate diagnosis, appropriate management, and a comprehensive approach to gastrointestinal health. From autoimmune disorders to infections and drug-induced reactions, exploring the multifaceted nature of villous atrophy enhances our grasp of gastrointestinal pathology and guides clinicians toward more nuanced and personalized patient care. Other Conditions Associated with Villous Atrophy In the following sections, we delve into a comprehensive exploration of diverse health conditions intricately linked to villous atrophy, shedding light on their unique associations and implications for gastrointestinal health. Eosinophilic Enteritis Eosinophilic enteritis is an inflammatory disorder characterized by an increased presence of eosinophils in the gastrointestinal tract. Eosinophils are a type of white blood cell involved in the immune response. In eosinophilic enteritis, these cells infiltrate the walls of the intestines, causing inflammation and damage. This inflammatory process can lead to various symptoms, including abdominal pain, diarrhea, and malabsorption. In some cases, the inflammation may result in villous atrophy, affecting the absorptive capacity of the small intestine. Diagnosis often involves endoscopic procedures with tissue biopsy to evaluate the extent of inflammation and associated damage. Crohn's Disease Crohn's disease is a chronic inflammatory bowel disease that can affect any part of the gastrointestinal tract, from the mouth to the anus. In the small intestine, Crohn's disease can cause inflammation and damage to the intestinal lining, leading to complications such as strictures and fistulas. In some cases, individuals with Crohn's disease may experience villous atrophy, particularly in areas of the small intestine affected by inflammation. The severity of villous atrophy can vary among patients with Crohn's disease, and its presence may contribute to malabsorption issues and nutritional deficiencies. Management often involves anti-inflammatory medications, immunosuppressants, and, in severe cases, surgical intervention to address complications. Giardiasis Giardiasis is an intestinal infection caused by the parasite Giardia lamblia. This parasitic infection can lead to symptoms such as diarrhea, abdominal cramps, and bloating. In addition to the acute phase of the infection, chronic giardiasis has been associated with villous atrophy in some cases. The mechanisms by which Giardia lamblia causes villous atrophy are not fully understood, but it is believed to involve both direct damage to the intestinal lining and an immune response triggered by the presence of the parasite. Diagnosis typically involves stool tests to detect the parasite, and treatment includes antiparasitic medications. Common Variable Immunodeficiency (CVID) Common Variable Immunodeficiency (CVID) is a primary immunodeficiency disorder characterized by impaired antibody production, leading to increased susceptibility to infections. Some individuals with CVID may experience gastrointestinal symptoms, including chronic diarrhea and malabsorption. In severe cases, villous atrophy can occur, impacting the absorption of nutrients in the small intestine. The association between CVID and villous atrophy underscores the complex interplay between the immune system and the intestinal mucosa. Management involves immunoglobulin replacement therapy to address the immune deficiency and supportive measures for gastrointestinal symptoms. Autoimmune Enteropathy Autoimmune enteropathy is a rare autoimmune disorder that primarily affects the small intestine. In this condition, the immune system mistakenly attacks the cells of the intestinal lining, leading to severe inflammation and damage. Villous atrophy is a characteristic feature of autoimmune enteropathy, affecting the absorptive surface area of the small intestine. Individuals with autoimmune enteropathy often present with persistent diarrhea, malabsorption, and failure to thrive. Diagnosis requires extensive evaluation, including endoscopic procedures and tissue biopsy. Treatment involves immunosuppressive medications to modulate the autoimmune response and manage symptoms. Human Immunodeficiency Virus (HIV) Advanced Human Immunodeficiency Virus (HIV) infection can result in various gastrointestinal complications, affecting both the upper and lower parts of the digestive tract. HIV-associated enteropathy may involve villous atrophy, contributing to malabsorption and nutritional deficiencies. The mechanisms leading to villous atrophy in HIV infection are multifactorial, involving both direct viral effects and immune-mediated processes. Additionally, opportunistic infections and other HIV-related complications can further impact the gastrointestinal mucosa. Management includes antiretroviral therapy to control HIV replication and supportive measures to address nutritional deficiencies and associated symptoms. Regular monitoring and a multidisciplinary approach are crucial in the care of individuals with HIV-associated gastrointestinal conditions. Dermatitis Herpetiformis (DH) Dermatitis herpetiformis is a chronic skin condition characterized by intensely itchy, blistering skin lesions. While DH primarily manifests as a skin disorder, its connection to celiac disease is well-established. Both conditions share a common trigger: gluten ingestion. DH is considered the skin manifestation of celiac disease, and individuals with DH often have underlying gluten sensitivity. The immune response triggered by gluten in susceptible individuals leads to the formation of IgA antibodies, which deposit in the skin, causing the characteristic skin lesions. While DH predominantly affects the skin, it is crucial to recognize its association with celiac disease, as individuals with DH may also experience villous atrophy in the small intestine. Therefore, a gluten-free diet is not only essential for managing skin symptoms but also for addressing the underlying celiac disease and preventing intestinal damage. Diagnosis involves skin biopsy for characteristic IgA deposits and, in some cases, intestinal biopsy to assess the extent of villous atrophy. Treatment primarily revolves around strict adherence to a gluten-free diet, often complemented by medications to control skin symptoms. Managing DH effectively requires a multidisciplinary approach, involving dermatologists, gastroenterologists, and dietitians to address both the skin manifestations and the underlying celiac disease. Idiopathic Sprue Idiopathic sprue is a term used for cases of sprue (malabsorption syndrome) where the cause is unknown. It may include cases that do not fit the criteria for celiac disease or other known causes of malabsorption. It shares some features with celiac disease, such as malabsorption and damage to the small intestine, but it lacks specific diagnostic markers for celiac disease. Diagnosis may involve excluding other causes of malabsorption, and it may be considered when typical celiac disease markers are absent. Tropical Sprue Tropical sprue is a malabsorption syndrome that occurs in tropical regions, and its exact cause is not fully understood. It is thought to be associated with infections or environmental factors. It presents with symptoms of malabsorption, such as diarrhea, weight loss, and nutritional deficiencies. It is more commonly observed in tropical regions but can occur in non-tropical areas as well. Collagenous Sprue Collagenous sprue is a rare disorder characterized by collagen deposition in the small intestine. The cause is not well-established. It leads to malabsorption and features similar to celiac disease but is distinguished by the characteristic collagen band in the intestinal lining. Diagnosis involves histological examination of small intestinal biopsies. The management of collagenous sprue may involve a combination of treatments, including a gluten-free diet and immunosuppressive medications. Corticosteroids or other immunosuppressants may be prescribed. Peptic Duodenitis Peptic duodenitis, a condition characterized by inflammation of the duodenal lining due to exposure to stomach acid, shares a commonality with celiac disease in its potential to induce villous atrophy. In peptic duodenitis, the inflammatory response triggered by gastric acid can extend into the duodenum, disrupting the delicate balance of the intestinal mucosa. This sustained inflammation may lead to changes in the architecture of the small intestine, including the villi, finger-like projections crucial for nutrient absorption. The damage incurred can result in villous atrophy, akin to the characteristic intestinal changes observed in celiac disease. Helicobacter Pylori Helicobacter pylori, a bacterium known for its association with gastric ulcers and gastritis, has been implicated in gastrointestinal conditions that extend beyond the stomach, including potential involvement in villous atrophy akin to celiac disease. The presence of H. pylori in the duodenum and small intestine has been linked to chronic inflammation and alterations in mucosal architecture. The bacterium's ability to induce immune responses may contribute to the damage of the intestinal villi, compromising their structure and functionality. This shared consequence of villous atrophy highlights the interconnectedness of various gastrointestinal disorders and underscores the need for comprehensive investigations to discern the specific triggers and mechanisms at play. While celiac disease and H. pylori-related duodenal changes differ in their etiology, understanding the potential overlap in their impact on intestinal health is crucial for accurate diagnosis and tailored therapeutic interventions. Small Intestinal Bacterial Overgrowth (SIBO) Small intestinal bacterial overgrowth (SIBO) is recognized for its capacity to disrupt the normal balance of microorganisms in the small intestine, leading to various gastrointestinal manifestations. In some cases, SIBO has been associated with mucosal damage, mirroring the villous atrophy observed in conditions like celiac disease. The overgrowth of bacteria in the small intestine can interfere with nutrient absorption and trigger an inflammatory response, potentially contributing to the erosion of the intestinal villi. While the mechanisms differ from those in celiac disease, the shared outcome of villous atrophy underscores the intricate relationship between dysbiosis and intestinal health. Lymphoma Lymphoma, a form of cancer that originates in the lymphatic system, can exhibit parallels with celiac disease in terms of inducing villous atrophy. In some cases, individuals with longstanding untreated celiac disease may face an elevated risk of developing enteropathy-associated T-cell lymphoma (EATL), a rare but serious complication. EATL is characterized by the infiltration of malignant T lymphocytes into the intestinal mucosa, leading to structural changes reminiscent of villous atrophy. While lymphoma and celiac disease differ fundamentally, the shared manifestation of villous atrophy underscores the intricate interplay between chronic inflammation and the potential oncogenic transformations within the gastrointestinal milieu. Thiamine (Vitamin B1) Deficiency There is some old research that indicates that prolonged low thiamine (vitamin B1) may cause thinning of the microvillus membrane. While these conditions may share some clinical features with celiac disease, the differences in their etiology, histopathology, and diagnostic criteria make them distinct entities. Accurate diagnosis and differentiation often require a thorough clinical evaluation, including serological tests, histopathological examination, and consideration of geographic or idiopathic factors. Consulting with a gastroenterologist or healthcare professional is essential for proper diagnosis and management. Drug-Associated Enteropathy: Medications Associated with Villous Atrophy Understanding the intricate interplay between medications and intestinal well-being is paramount for individuals managing chronic health conditions. While medications play a pivotal role in alleviating symptoms and improving overall health, certain drugs may harbor the potential to influence the delicate environment of the small intestine. This section delves into the impact of various medications on the intestinal villi, focusing on conditions that may lead to villous atrophy. From common pain relievers to immunosuppressive drugs, the discussion aims to shed light on the nuanced relationship between medications and gastrointestinal health. It underscores the importance of informed healthcare decisions, proactive monitoring, and open communication between patients and healthcare providers to mitigate potential complications and ensure optimal intestinal function during the course of medical treatments. Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) are commonly used to alleviate pain and inflammation, but prolonged and excessive use has been associated with adverse effects on the gastrointestinal (GI) tract. NSAIDs can cause irritation and inflammation in the small intestine, potentially leading to villous atrophy. The mechanism involves the inhibition of cyclooxygenase enzymes, which play a role in maintaining the integrity of the GI mucosa. Individuals relying on NSAIDs for chronic pain management should be cautious and work closely with healthcare providers to monitor and mitigate potential GI complications. Immunosuppressive Drugs Immunosuppressive drugs, such as methotrexate and mycophenolate mofetil, are crucial in managing autoimmune conditions and preventing organ rejection after transplantation. While these medications target the immune system to curb excessive responses, they may also impact the gastrointestinal lining. Long-term use could lead to intestinal complications, including villous atrophy. Healthcare providers prescribing immunosuppressive drugs carefully assess the risk-benefit profile for each patient and monitor closely for potential adverse effects on the GI tract. Chemotherapy Drugs Chemotherapy, a cornerstone in cancer treatment, aims to eradicate rapidly dividing cells, including cancerous ones. However, the impact isn't limited to tumors, and normal, healthy cells may also be affected. The rapidly renewing cells in the small intestine are particularly susceptible, potentially resulting in damage to the villi and compromising the absorptive capacity of the intestines. Individuals undergoing chemotherapy should discuss potential gastrointestinal side effects with their oncologist to address and manage any complications that may arise. Some Antibiotics Certain antibiotics, such as tetracycline and ampicillin, may disrupt the balance of the gut microbiota, leading to gastrointestinal disturbances. While these antibiotics target harmful bacteria, they can also affect beneficial microbes, influencing the overall health of the intestinal lining. The intricate relationship between antibiotics and the gut underscores the importance of judicious antibiotic use and, when necessary, the simultaneous administration of probiotics to support a healthy gut environment. Proton Pump Inhibitors (PPIs) Proton Pump Inhibitors (PPIs), commonly prescribed for acid reflux and gastroesophageal reflux disease (GERD), reduce stomach acid production. Prolonged use of PPIs has been linked to changes in the small intestine, potentially impacting the structure and function of the villi. Individuals relying on PPIs for an extended period should collaborate with healthcare providers to assess the necessity of continued use and explore alternative approaches to manage acid-related conditions. Opioid Pain Medications Opioid pain medications, including morphine and oxycodone, are known for their analgesic properties but are also associated with side effects such as constipation. Chronic use of opioids may lead to intestinal issues, affecting the normal functioning of the small intestine. It is crucial for healthcare providers to carefully manage opioid prescriptions, considering the potential impact on the gastrointestinal tract, and to explore alternative pain management strategies whenever possible. Patients should communicate openly with their healthcare team about any digestive issues experienced during opioid therapy to ensure timely intervention and support. Conclusion In conclusion, the journey through conditions associated with villous atrophy extends far beyond the realms of celiac disease. This exploration has highlighted the intricate interplay of various factors that can impact the health of the small intestine, leading to structural changes in the form of villous atrophy. Recognizing these diverse contributors is pivotal for healthcare professionals navigating the complexities of gastrointestinal disorders. As we deepen our understanding of the nuanced manifestations of villous atrophy, we pave the way for improved diagnostic accuracy and tailored treatment strategies. The heterogeneity of conditions linked to villous atrophy underscores the need for a holistic and individualized approach to patient care, ensuring that the intricacies of each case are addressed with precision and empathy. Through continued research and clinical vigilance, we strive to unravel the mysteries of these conditions and enhance the well-being of individuals facing the challenges of villous atrophy. Further reading on the topic of other causes of villous atrophy: Not All That Flattens Villi Is Celiac Disease: A Review of Enteropathies -
Celiac.com 02/20/2023 - Celiac disease is a condition that is caused by the immune system's response to gluten, a protein found in wheat, rye and barely. In celiac patients, an immune response triggers a pro-inflammatory environment in the small intestine, causing damage to the tissue. A major role in the pathogenesis of celiac disease is played by the HLA-restricted gliadin-specific intestinal T-cell response generated in a pro-inflammatory environment. A recent review article highlights the growing body of research that supports the central role of inflammation in the development of celiac disease, and how it is influenced by factors such as sensitivity to gluten and other pro-inflammatory agents. The review is authored by researchers Maria Vittoria Barone, Renata Auricchio, Merlin Nanayakkara, Luigi Greco, Riccardo Troncone, and Salvatore Auricchio. The are variously affiliated with the Department of Translational Medical Science, University Federico II in Naples, Italy; and the European Laboratory for the Investigation of Food Induced Disease (ELFID), University Federico II in Naples, Italy. Live studies on a population at risk have explored the mechanisms behind this inflammation. These studies show cellular and metabolic alterations in the absence of a T cell-mediated response, before the onset of the disease and before the introduction of gluten in the diet. Gluten exacerbates these constitutive alterations, both live and in the lab. The role of inflammation in celiac disease has led researchers to consider it as a chronic inflammatory disease, similar to other autoimmune disorders. The review also explores the crucial role played by the intestine in controlling inflammation both locally and systemically, and the impact of nutrients and gut bacteria on inflammation. Reduction of Early Inflammation Could Delay Onset of Celiac Disease Celiac disease is characterized by inflammation, which plays a critical role in the onset of the disease. It begins with a pre-clinical phase where the body is set up for inflammation, making it susceptible to various pro-inflammatory agents, including gluten. Historically, research has focused on the T-cell response in celiac disease, but there is growing recognition of the importance of the pre-inflammatory state. Modulating this state with a Mediterranean-type diet or preventing intestinal viral infections could have a significant impact on the onset of celiac disease, and could be easier to manage than the more complex autoimmune response. The implications of this research extend to additional chronic inflammatory diseases including inflammatory bowel diseases and diabetes, where early intervention with the state of inflammation in at-risk subjects could have a lasting impact on their health. Read more in mdpi.com
- 1 comment
-
- causes
- celiac disease
- (and 8 more)
-
Celiac.com 12/11/2006 - Yes, that's what I think. Gluten-sensitivity is a disease of your brain and nerves. The gluten puzzle I have come to this conclusion after studying the effects of gluten on my patients for over a decade. I am a pediatric gastroenterologist and allergist. I run a busy clinic for children and their parents. I have been increasingly concerned by the large numbers of my patients who are affected by gluten. I was perplexed by their wide-ranging symptoms. The puzzle was to explain how gluten could cause so much ill health to so many people in so many different ways, including celiac disease. Faulty brain control Eureka! The solution came when deep in discussion with my friend and colleague, Ron Harper, Professor of Neurobiology, UCLA. We were both struggling with the concept of multiple symptoms that needed to be explained. The answer appeared absurdly simple: disturbed "brain control". It suddenly seemed obvious—gluten could disturb the neural pathways of the body. Gluten was gradually damaging the brain and the nerves of susceptible people. It was the brain that was the common pathway for the manifestations of all of the gluten symptoms. So I set out to research what the world medical literature had to say. Is gluten a neurotoxin? I felt excited. I reviewed my patients in this new light—I began looking for a brain-grain connection. I began to see gluten as a neurotoxin—this could provide a universal model of gluten-sensitivity. This toxicity might act through inflammatory mechanisms or cross-reactivity with neurons. I began accumulating the evidence for my proposal that gluten-sensitivity is a brain and nerve disease. "Full Of It!" The concept of "Full of it" developed from the stories from my patients. I wrote my hypothesis down in a book now called Full of it! It refers to our diets being full of gluten; to the world being full of gluten-sensitive people; to the medical practitioners who are so skeptical of adverse reactions to gluten; to the enthusiasm of people who are feeling vibrant again on a gluten-free diet; and to those who are brimming with hope that the problem of gluten has now been recognized. Food allergy skeptics As a junior doctor I decided to formally research the food allergy phenomenon. I was awarded a research post and carried out the first comprehensive food allergy studies in New Zealand. I triumphantly demonstrated that food allergy was both a real entity and that it was common. But, to my disappointment, my colleagues were reluctant to believe me or my data. They professed a "disbelief" in food allergy. This surprised me as I had the research data. My next step was to conduct four more years of investigation of food allergy in Australia (at the Royal Childrens Hospital, Melbourne). This was a bigger and more elaborate study. My Doctoral Thesis (1982) based on this work is called: Food hypersensitivity in children: diagnostic approaches to milk and egg hypersensitivity. Since then I have continued my investigations into food allergy—but still today (25 years later) medical skepticism abounds. This "disbelief" is held despite the vast body of research describing food allergy. There seems to be an underlying unwillingness for doctors to consider food allergy as a possibility. Unfortunately, this also applies to gluten reactions. The shocking truth The shocking truth about gluten is that gluten foods are causing tremendous damage—but currently this is going mostly unrecognized. Unfortunately, gluten grains have become our staple diet. The quantity of gluten in our food supply has been steadily increasing. Yet worse, official Health Policies endorse gluten grains as the foundation of our food pyramid. Medics turn a blind eye Gluten is sapping the energy and wellbeing of countless millions. To date, the medical profession has turned a blind eye to glutens wider problems whilst focusing all of their attention on the narrow problem of celiac disease. A typical story I received emails like this every day: "Dr Ford, I have emailed you a number of times regarding our two children. I thought I should let you know that since going gluten free for the last three months, at last our son and daughter have put on some weight. If I had kept them on a normal gluten diet (which they recommended at the hospital) we would be still be having the headaches and sore tummies as well as the bad moods which our son would have. People just thought he was a naughty child, but now he is so different - we can talk to him without getting into any fights. I congratulate you for all your efforts on bringing gluten intolerance to the media and medical profession. More children and their families may find long awaited help. We have had to put up with this for seven years! At long last there is light at the end of the tunnel. Kind regards, Sue and Garry." Can gluten damage your brain? I believe that gluten was actually causing these two children to be sick. That is the explanation for their "naughty" behavior, their moods and their headaches. I postulate that gluten can damage your brain. I have come to this conclusion by the abundant circumstantial evidence from my observations of my patients who are gluten-sensitive. I have pondered the next questions: "Why do they have such an array of symptoms from gluten?" "Why do they recover so quickly when gluten is removed?" And "Why do they deteriorate so rapidly when only tiny amounts of gluten are eaten?" The concept of a brain/nerve disease can explain everything. The brain/nerve hypothesis "The symptoms from gluten occur through its action on the nervous system". I propose that gluten-sensitivity is a brain condition. Each and every organ in your body has some form of brain/nerve control. I propose that gluten can injure the delicate nervous networks that control your guts functions. A malfunction will subsequently lead to all of the gut symptoms that have so well been described. In addition, gluten can also directly affect brain function, which leads to the primary neurological symptoms that are so commonly seen with gluten-sensitivity. What is new? There are a number of new ideas that I put forward. These are based on circumstantial evidence. They produce a unifying theory of the symptoms that are attributed to gluten toxicity. A brain disease I consider that gluten-sensitivity is mostly a neurological problem. A major contribution to this debate is the realization that the brain has a central role in the expression of the symptoms that have, until now, been attributed to the local toxicity of gluten in the gut. A nerve disease I propose that gluten-sensitivity is a nerve disease. There is a gigantic network of nerves that controls every function that your gut is programmed to do. There are as many nerve cells in your gut as there are in your head! (about 25 billion nerve cells). I call it your tummy brain (or gut brain). Your tummy brain can be directly damaged by gluten reactions. This is the cause of so many sore tummies and bowel troubles. A wide spectrum of neurological manifestations For decades, there have been reports of unexplained brain and nerve symptoms which are associated with celiac disease. Although these associations have been described, there has been no universal mechanism proposed. However, if gluten is seen as a neurotoxin, then the explanation has been found. A very common disease Reactions to gluten have recently been documented to be extremely common. About one-in-ten people (as ascertained by blood donor studies) have high levels of gluten antibodies in their blood. My clinical studies have arrived at this same high number of gluten-sensitive people. Others have data to show that it is even more prevalent. Am I full if it? You might ask, "Is he full of it?" Yes, I am full of excitement and hope for the future. So many people can now be helped, if only this information can be widely distributed. I am full of ideas and full of enthusiasm. I hope that you are full of hope for your healthy and vibrant future. Tariq's story: "Dear Rodney, Thank you for your care and support of my family in regard to our allergies, gluten sensitivity and celiac disease that exists within that framework. My son Tariq, who is nearly 12 years old, has been a patient of yours over a number of years for his multiple food allergies. Tariq also suffers from dyslexia. Over the last several years Tariq has been becoming increasingly tired, lacking in energy and motivation, struggling with school work and constantly scratching due to his eczema and rashes covering all of his body. During this time, even though he has attended soccer training up to four times a week he somehow gained a lot of weight. Tariq was constantly grumpy and had low mood levels. Two months ago you diagnosed Tariq with gluten-sensitivity (his tTG 4; IgG-gliadin 86; IgA-gliadin 9). Tariq was extremely reluctant to go on a gluten free diet. But as the rest of the family had gone gluten-free—so he was forced also to become gluten-free. The changes that a gluten-free diet has evoked in Tariq have been astounding. His energy levels have increased, his skin has vastly improved, he has lost a lot of his excess weight (even though his appetite has increased) and he has shown improvement in his dyslexia. Tariq is not as grumpy as he was and his mood levels have improved. Tariq is now vigilant about gluten and can see the differences it has made to his life and the quality of it. Also, the other soccer parents have noticed a vast improvement in Tariq's energy levels and speed. His teacher has also noticed a big difference. Thanks again. Regards, Rosemary" Are you affected? The shocking truth is that gluten can damage your brain and that so many people are being encouraged to eat gluten-foods that might be steadily eroding their health and energy. If you have any lingering doubt about your own health, then I suggest that you check out the possibility of gluten-sensitivity.
-

What Causes Villous Atrophy Besides Celiac Disease?
Scott Adams posted an article in Additional Concerns
Celiac.com 06/01/2021 - Villous atrophy not caused by celiac disease is called "non-celiac enteropathy." In many cases, the symptoms mirror the classic symptoms of celiac disease: diarrhea, weight loss, abdominal pain, and fatigue. Spotting the difference between celiac disease and non-celiac enteropathy can be challenging. That's why physicians recommend celiac disease blood tests, which are used to find adverse immune reactions to the gluten protein in the foods you eat. Just as it's possible to have damaged villi without celiac disease, it's possible to have celiac disease, and villi damage, even with negative blood antibody tests. People with celiac disease usually improve on a gluten-free diet. While some may not, many folks with non-celiac enteropathy do not respond to a gluten-free diet. People who do not see symptom improvement on a gluten-free diet may need to consider alternative causes for their symptoms and villous atrophy. Non-Celiac Causes of Villous Atrophy Non-celiac causes of villous atrophy include: Benicar (olmesartan) In some patients, taking this blood pressure medication leads to villous atrophy combined with diarrhea and weight loss. The U.S. Food and Drug Administration issued a warning about this in 2013. Common Variable Immune Deficiency, or CVID CVID is a condition that leaves people vulnerable to recurrent infections. Crohn's disease Villous atrophy is unusual in Crohn's disease, but can happen. Lymphoma One study found two different types of lymphoma could cause villous atrophy: small intestinal T-cell lymphoma, and enteropathy-associated T-cell lymphoma. Enteropathy-associated T-cell lymphoma is closely linked to celiac disease. Casein/Cow's Milk Intolerance Research has shown that flattened villi can also be caused by casein intolerance. For more info see "Mucosal reactivity to cow's milk protein in C(o)eliac disease," which states "A mucosal inflammatory response similar to that elicited by gluten was produced by CM (Cows Milk) protein in about 50% of the patients with coeliac disease. Casein, in particular, seems to be involved in this reaction." Certain Drugs Drugs that suppress your immune system (such as Imuran and CellCept), the antibiotic neomycin, and the anti-inflammatory medication Colcrys, also have been linked to reports of medication-induced villous atrophy. Small intestine Bacterial Overgrowth, or SIBO Symptoms of SIBO can mimic those of celiac disease. Other possible causes of villous atrophy, including infection with parasites or with the ulcer-causing bacteria Helicobacter pylori, also have been reported. Thiamine Deficiency and/or Beri Beri Both can cause thinning of the villi, leading to both casein/lactose intolerance and in time possibly a celiac disease or non-celiac gluten sensitivity (NCGS) diagnosis. Not all Villous Atrophy is From Celiac Disease Most, but not all, cases of villous atrophy are caused by celiac disease. Patients with negative blood test, who do not see symptoms improve on a gluten-free diet, should consult with a doctor about other possible causes of villous atrophy.- 10 comments
-
Celiac.com 04/23/2021 - The above phrase may seem to be an obvious statement. However, I believe if many of us with gluten sensitivities look closely at our lives, we will find that we are apt to ascribe most of our physical abnormalities to gluten. Not consuming gluten makes such a huge difference in one’s physical well being that many of us come to believe that gluten must be responsible for just about everything when we feel “bad.” Seeking information on life without gluten, I regularly read a number of celiac disease support forums on the Internet. It is not uncommon to see posts about all kinds of symptoms such as tingling, headaches, anxiety, stomach cramps, limb weakness, and skin problems (which may or may not be dermatitis herpetiformis). The authors of these posts are almost always seeking others with celiac disease who have experienced similar problems. These questions are posed out of a personal sense that eating gluten is associated with the bothersome, even worrisome, physical symptom in question. Indeed, the connections may be very real! But once an individual hears of another person who has similar problems, they rest easy—assured that symptoms have been only a “gluten” effect. Recent events in my own health have caused me to clearly see that one can, indeed, experience symptoms connected to gluten ingestion that are certainly real, but the symptoms can also be harbingers of an underlying disease that has nothing at all to do with celiac. In other words, a disease separate from celiac may be present, and exposure to gluten may worsen the symptoms of that disease. Conversely, not eating gluten may lessen the symptoms, but will not cure the disease. Eat no gluten, the symptoms go away … but the disease remains, almost insidiously in silence. If you have a persistent medical problem—even if it improves with eating gluten free—my advice is to GO TO YOUR DOCTOR and MAKE SURE to have full diagnostic tests. Do not leave your diagnosis to just asking others on a celiac support forum if they’ve experienced anything similar. For some years, I had a cascade of neurological symptoms. They seemed to be small seizures, problems with my eyes, weakness in my hands, and electrical-shock type of pains down my back. When I stopped eating gluten, these symptoms either went away completely or diminished to rare appearances. I actually did go see a neurologist, but—at the time I saw him—I’d been eating gluten free for about 2 years, and most of my neurological symptoms had abated. I also told him that if I did accidentally ingest gluten, some of the symptoms would return. In an effort to not break our household bank by sending me for an MRI, the doctor agreed that whatever it was seemed to be associated with the gluten. He was not worried, so neither was I. We agreed I’d continue to avoid gluten, and...no MRI was done. Until three years later, when I ended up unconscious on the bathroom floor from a grand mal seizure, and temporarily paralyzed on my left side. I was rushed to the hospital with everyone thinking I’d had a stroke. However, they immediately performed a CT scan and there it was. I had a large, flat pancake-shaped meningioma tumor in the region of my frontal lobe. Within a week, I was in surgery for a craniotomy and it has now been removed, along with the brain tissue that was attached. This is a situation where eating gluten free actually ended up masking a significant medical problem that I had. I cannot say why eating GF might have made things better. I do know that a large part of my reaction to gluten is inflammation in my joints—so why not inflammation around the tumor as well, increasing the possibility of neurological problems? Such conjecture really matters little at this point. I should have had an MRI years ago, to make sure there was nothing amiss—even though so many of my symptoms had improved after eating gluten free. In fact, I was doing such a great job of being my own doctor about this, that my neurologist even believed my “diagnosis” of gluten-related problems to be the probable issue. Believe me, brain surgery is no picnic. I did well, and had an excellent neurosurgeon, but even now—months post surgery—I am still recovering in many ways. I cannot help but wonder if, three years ago when my doctor and I elected not to do that MRI, the discovery of the tumor then would have resulted in an easier process. A smaller tumor might have led to less invasion of my brain tissue. I hope my story helps others to stop and think. Gluten can be such a powerful toxin that it may actually work to worsen symptoms of other diseases—or, by the same token, lessen those symptoms if you do not consume gluten. However, eating or avoiding gluten does not necessarily make all other diseases disappear. One may end up (as I did) blaming problems on gluten, and failing to seek out the cause of the underlying problem. We should all be very cautious about self-diagnosis. Gluten truly is at the root of many problems for so many people. It is natural and easy to begin to blame almost every physical discomfort on exposure to gluten. Perhaps, with some of us, it is a convenient form of denial to decide “all I have to do is not eat gluten, and my health will be perfect.” I learned that this kind of thinking can be a trap as well. I’d like to leave the reader with one last thought. There appears to be significant connections between gluten and the brain. By Googling “celiac and brain disease,” one gets more than half a million hits. Even the NIH page on celiac disease notes that one symptom may be seizures. Who knows? Someday scientists may find that gluten sensitivity is a root cause of meningioma tumors, just as it is for other diseases, such as osteoporosis. Whether gluten played a role or not, the disease was there—possibly festering for decades—and I was closing my eyes to the reality of what it might truly be, under the blanket of “everything bad is about gluten”—until it could not be ignored any longer.
- 2 comments
-
- causes
- celiac disease
-
(and 3 more)
Tagged with:
-
Celiac.com 09/25/2020 - New research into the origin of our medical woes has revealed something startling: As it turns out, we are our own worst enemy. Yes, the Pogo quote of yesteryear found in the title of this article is quite accurate when applied to our medical lives. We love to discuss those things that we call “causes” of diseases even though we often have little knowledge of how these things really cause illness. Even medical professionals can have difficulty grasping the true cause-and-effect. But that becomes understandable once some insight is gained into the true nature of medical training. One would think that we are exposed to the gamut of current medical knowledge in medical school. But in fact, we gain limited knowledge as to the true workings of pathogens, parasites, and chemical insults. Sure, we are often taught which virus or bacteria causes a certain disease state and are then shown the established/accepted mode of therapy. But most of us never gain an appreciation for the circumstances that led to that illness or why one individual has the condition while the next person remains healthy. We are also not told why many of these “pathogens” are ubiquitous in the environment and yet only cause clinical syndromes in a relatively small percentage of individuals. We refer to “immunity” but don’t delve into the fine points of why one pet or person lives to a ripe old age while the next one develops cancer or some other catastrophic illness at a much earlier age. We usually point to the old standby of “genetics” for the explanation. As many of you know, I love to discuss “genetics”. Now, I do not claim to be an authority on the subject, but I do love kicking it around. I like to ponder the logic behind scientists’ referring to certain diseases as “genetic” without offering a good explanation for why these “genes” wait so long to manifest. Do genes wait? Do the genes that code for our brain, liver and kidneys to form properly wait for 6 months or 6-60 years to do what they do? I get a kick out of reading how genes “mutate”, as well. Certainly, we do get true genetic mutations at times (e.g. one arm, one kidney, two heads) but thankfully these are relatively rare when compared to the number of “genetic mutations” that have been reported to cause disease. Here’s a door-opening key: Researchers now estimate that up to 45% of the genetic information in our DNA is viral information, some active and some extinct. Have you grasped the importance of this yet in relationship to the preamble above? Think about it for a moment before proceeding. Got it? Can you now see that our DNA not only contains the information that makes you who you are phenotypically (outward, observable appearance) but also has information encoded in it that can govern the outcome of your medical life. Yes, your double-stranded DNA is a little virus hotel and the guests can get a bit rowdy. I love to tell people that if I could do a Star Trek type of scan on then and give them a print out of all of the viruses in their body, both “genetic” and acquired, then they just might take better care of themselves. But here is the good news...the really cool news...the new “medical gospel”. We have much better control over our medical lives than most think or have been told. In fact, it is phenomenal how much control we have over whether we live a long, healthy life or a brief, afflicted one. How can that be, especially if these “culprits” are in our very DNA? Ahhhh! There is the amazing thing to see. They are not culprits. Viruses are residing in our body for a purpose and a good purpose at that. Viruses are responsible for two critically important functions in nature: Variation and adaptation. Yes, it is the virus that is behind much of what is termed “evolution”. Many viruses can change in response to alterations in their environment, sort of like a chameleon or a flounder. (How do they do that, anyway???) How did we end up with soooo many variations of butterflies? As many of you know, I am a creationist and wholeheartedly believe in God. But I also see how He could have used viruses to facilitate the wide array of appearances among the different species of insects, animals and plants. There are numerous species of butterflies. However, they are all butterflies. In order to prove his theory of evolution, Darwin himself said that finding numerous inter-species would be required. Have we found them? Would he now believe in his original theory? But the focus of this medical discussion should be on the adaptability of the virus. Yes, they are quite adept at this maneuver. And that is to our benefit more than it is to our detriment. Viruses exist throughout nature and our individual bodies in order to facilitate our adaptation to this ever-changing environment. If we could snap our fingers and take all of the viruses out of nature, the entire ecosystem would collapse, including this amazing thing we call a body. They are busily working away to help us cope with daily challenges such as air pollution, malnutrition, hormonal variations, and other microorganisms. They sense the change in their surroundings and react- and appropriately, I might add. “But what about the ‘diseases’ they cause?” you might be asking. Well let’s use my favorite example called cancer—nearly everyone’s biggest fear. We have demonized the virus in those forms of cancer that have been publicized as being “caused” by the virus. (I believe that most of you will hear in your lifetime that all cancer is viral.) In reality, the virus would not have caused the cancer without being goaded into it by what we call carcinogens. And, the cancer would not have developed had the immune system not failed in its duty. So, we suddenly see that cancer, like so many other conditions, is a “syndrome”, with multiple factors coming together to produce the result. Now, let’s dissect that premise for a moment. Viruses are in situ, doing what they do, adapting to changes and insults that are thrown our way. Along comes a “carcinogen” and the virus forms a tumor. Now whose fault was that? I mean, can we blame the virus for making a cocoon for itself and the cell it was charged to protect? (Do you see how I tried to just quickly slip that past you?) But seriously, I now look at tumors as the ultimate adaptation of the virus that we know “causes” the cancer. Once the insults are bad enough, the viruses goes into survival mode, telling the cell to replicate itself in order to survive the caustic insult we call a carcinogen. Is that too far-fetched? Again, this process does not occur until one more thing of vital importance takes place, which is the failure of the immune system to do its job. Yes, as some love to point out at cocktail parties, we are all fighting cancer as we speak...hopefully. As long as we possess a competent immune system, we are successful in our battle to keep cells that are being challenged with carcinogens (that we face every single day) from turning into cancer. However, once our immunity wanes, we are subject to these ongoing processes. Thankfully, there is an intermediate stage called “immune-mediated disease” where the immune system does housecleaning to rid our bodies of these revolutionaries that are gaining an upper hand in the face of our deteriorating governor. A number of wise doctors have said that cancer is the end game of immune mediated diseases, meaning that cancer often follows long bouts with “autoimmune*” conditions (*a term I no longer use). And they are right IF we survive the immune mediated attack. But how do we treat “autoimmune diseases”? Yes, we use immune suppressing drugs. Oh,oh! The term “pretzel logic” comes to mind. This is in the same vein as using carcinogens to treat cancer. Kinda sorta doesn’t make good sense. So whose fault is it when we fail with our current mode of therapy in the treatment of autoimmune diseases and cancer? “Darn those viruses and carcinogens.” So why is there so much variation in the age of onset and severity of cancer? I think we should all be gaining some insight into this conundrum by now. Cancer, like so many diseases, is a spectrum disorder, meaning that we have individuals ranging from the “best of the best” to the “worst of the worst”. The best live to be over 100 years old and experience a relatively disease-free life. The worst don’t survive the time in the womb. We see brain tumors and leukemia in the very young and in the aged. We also see age spikes in the cancer rates that are quite logical, accompanying concurrent stresses such as adolescence and “the wall” at age 40, while observing a meteoric rise after age 65. I used to call cancer viruses “opportunists”, applying to them the connotation of being malicious or even “evil”. But now I see that categorization was inaccurate and downright unfair. They are not waiting around to cause cancer or other diseases; they are FORCED into it by us. We are the ones supplying the carcinogens. We are the ones eating diets that are filled with potentially damaging proteins (gluten, casein , soy, and corn), chemicals, trans fats, and food additives. We are the ones who are trouncing our immune systems through poor diets, lack of exercise, improper sleep, and crazy lifestyles. We are our own worst enemy! We are quite accomplished at the blame game when it comes to shirking our own responsibilities in this process. But, in all fairness, it is not completely the patient’s fault. Look at the current medical and pharmacological approach to the symptoms we experience. “Got a fever? Not anymore. We have a pill for that. (Forget that fever is essential in the proper immune response.)” “Got heartburn, IBS, headaches, fibromyalgia, insomnia, or depression? Not anymore. We have lots of pills for those. (And you no longer have to worry about what causes them because “these medications can be taken for life”.) So, whose fault is it when those symptoms go away and the next and more severe set arise? I tell people, “If you don’t like these warning signs, you’re really not going to like the next set. And if you don’t like those, you’re really not going to like what they are warning you of.” What’s the bottom line? We need to wake up! We need to realize that our bodies are an amazing entity with the ability to withstand serious insult- repeated, ongoing insults. But, there is a limit to what it can take. Thankfully, that limit is quite gracious. But there will come a time when our bodies and those incredible little viruses in them say enough is enough. The phenomenal thing to see is that we have the vast majority of the say in when that occurs. We simply have to stop doing the harm that we are doing to these downright miraculous vessels that we have been given. It is that simple. It is not necessarily easy, but it is that simple. Are we our own worst enemy? We don’t have to be. Now that’s great news!
-
Celiac.com 05/29/2014 - Many people with celiac disease report symptoms of depression, which usually subside upon treatment with a gluten-free diet. But a new study out of Australia suggests that gluten can cause depression in people with non-celiac gluten-sensitivity. Current evidence shows that many patients with self-reported non-celiac gluten sensitivity (NCGS) continue to have gastrointestinal symptoms on a gluten-free diet, but say that avoiding gluten makes them feel ‘better'. So, why do people with non-celiac gluten sensitivity seem to feel better on a gluten-free diet, even if they still have gastrointestinal symptoms? A team of researchers wanted to know if this might be due to gluten’s effects on the mental state of those with NCGS, and not necessarily because of gastrointestinal symptoms. The research team included S. L. Peters, J. R. Biesiekierski, G. W. Yelland, J. G. Muir, and P. R. Gibson. They are affiliated with the Department of Gastroenterology, Central Clinical School of Monash University at The Alfred Hospital in Melbourne, the Department of Gastroenterology at the Eastern Health Clinical School of Monash University in Box Hill, and the School of Health Sciences at RMIT University in Bundoora, Victoria, Australia. For their double-blind cross-over study, they looked at 17 women and five men, aged 24–62 years. All participants suffered from irritable bowel syndrome, but not from celiac disease, and their symptoms were controlled on a gluten-free diet. The team gave the participants one of three random dietary challenges over 3 days, followed by a minimum 3-day washout before moving to the next diet. All participants got all three diets over the course of the study. For each phase, the team supplemented the challenge gluten-free food with gluten, (16 g/day), whey (16 g/day) or nothing at all (placebo). The team assessed mental state as determined by the Spielberger State Trait Personality Inventory (STPI), cortisol secretion and gastrointestinal symptoms. They found that gluten ingestion was associated with higher overall STPI state depression scores compared to placebo [M = 2.03, 95% CI (0.55–3.51), P = 0.010], but not whey [M = 1.48, 95% CI (−0.14 to 3.10), P = 0.07]. They found no differences for other STPI state indices or for any STPI trait measures, and they saw no difference in cortisol secretion between challenges. Gastrointestinal symptoms were similar for each dietary challenge. Short-term exposure to gluten specifically induced current feelings of depression with no effect on other indices or on emotional disposition. Moreover, the team saw no gluten-specific trigger of gastrointestinal symptoms. Such findings might explain why patients with non-coeliac gluten sensitivity feel better on a gluten-free diet despite the continuation of gastrointestinal symptoms. Source: Aliment Pharmacol Ther. 2014;39(10):1104-1112.
-
- causes
- depression
-
(and 5 more)
Tagged with:
-
Celiac.com 02/19/2018 - It's very important that people with celiac disease maintain a gluten-free diet. Still, there has been some data to suggest that some people with celiac disease may be "hyper vigilant" in their approach to a gluten-free diet, and that such extreme vigilance can cause them stress and reduce their overall quality of life. Can a more relaxed approach improve quality of life for some people with the disease? A team of researchers recently set out to determine whether "extreme vigilance" to a strict gluten-free diet may increase symptoms such as anxiety and fatigue, and therefore, lower quality of life (QOL). The research team included Randi L. Wolf, Benjamin Lebwohl, Anne R. Lee, Patricia Zybert, Norelle R. Reilly, Jennifer Cadenhead, Chelsea Amengual, and Peter H. R. Green. They are variously affiliated with the Department of Health and Behavior Studies, Program in Nutrition, Teachers College Columbia University New York USA, the Department of Medicine, Celiac Disease Center Columbia University Medical Center, Harkness Pavilion New York, USA. The team assessed the influence of QOL with energy levels and adherence to, and knowledge about, a gluten-free diet. For their cross-sectional prospective study, the team looked at 80 teenagers and adults, all with biopsy-confirmed celiac disease, living in a major metropolitan area. They assessed QOL using celiac disease-specific metrics. The team based dietary vigilance on 24-hour recalls and an interview. They based knowledge on a food label quiz. They used open-ended questions to describe facilitators and barriers to following a gluten-free diet. Overall, extremely vigilant adults had greater knowledge, but significantly lower QOL scores than their more relaxed counterparts. Both teens and adults who reported lower energy levels had much lower overall QOL scores than those with higher energy levels. To maintain a strict gluten-free diet, hyper-vigilant celiacs were more likely to avoid eating out, to cook at home, and to use internet sites and apps. For hyper vigilant eaters, eating out was especially challenging. Being hyper-vigilant about maintaining a strict gluten-free diet can cause stress and adverse effects in both teens and adults with celiac disease. Doctors may want to look toward balancing advocacy of a gluten-free diet with promoting social and emotional well-being for celiac patients. In some cases, allowing a more relaxed approach may increase well-being and, thus, make dietary adherence easier. Obviously, people would need to tailor any relaxation in their gluten-free vigilance to make sure they weren't suffering preventable symptoms or doing themselves any harm. Source: Dig Dis Sci (2018)
- 29 comments
-
Celiac.com 09/09/2013 - Many people with celiac disease show slightly elevated liver enzymes, though these enzyme levels usually return to normal after gluten-free diet. A team of researchers recently set out to investigate the cause and prevalence of altered liver function tests in celiac patients, basally and after 1 year of gluten-free diet. The research team included Giovanni Casella, Elisabetta Antonelli, Camillo Di Bella, Vincenzo Villanacci, Lucia Fanini, Vittorio Baldini, and Gabrio Bassotti. They are affiliated with the Medical Department, and the Clinical Pathology Department of Desio Hospital in Monza and Brianza, Italy, the Department of Clinical and Experimental Medicine, Gastroenterology and Hepatology Section at the University of Perugia in Perugia, Italy, and with the Department of Laboratory Diagnostics, Pathology Section, Brescia, Italy. The team gathered data from 245 untreated celiac disease patients, 196 women and 49 men, ranging in age from 15 to 80 years. They then analyzed the data, and assessed the results of liver function tests performed before and after diet, as well as associated liver pathologies. They found that 43 (17.5%) of the 245 patients, showed elevated levels of one or both aminotransferases; In 41 patients (95%) the elevation was mild, meaning that it was less than five times the upper reference limit. The remaining two patients (5%) showed marked elevation, meaning levels more than ten times the upper reference limit. After patients eliminated gluten for one year, aminotransferase levels normalized in all but four patients, who had HCV infection or primary biliary cirrhosis. Celiac patients who show hypertransaminaseaemia at diagnosis, and who do not show normalization of liver enzymes after 12 months of gluten-free diet, likely suffer from coexisting liver disease. In such cases, the research team recommends further assessment to assess the possible coexisting liver disease. Spotting and treating coexisting liver disease in celiac patients is important for improving liver function and preventing possible complications. Source: Liver International. 2013;33(7):1128-1131.
-

Scientists Finally Know What Causes Celiac Disease!
Jefferson Adams posted an article in Latest Research
Celiac.com 08/19/2015 - For the first time since it was described and named by 1st century Greek physician Aretaeus of Cappadocia, first linked to wheat in the 1940's, and specifically linked to gluten in 1952, scientists have discovered the cause of celiac disease. Professor Ludvig Sollid, and his team at the Centre for Immune Regulation at University of Oslo, have discovered that people with celiac disease suffer from one of two defective human leukocyte antigens (HLAs), which cause the immune system to see gluten molecules as dangerous, triggering the immune response that causes classic celiac-associated inflammation and other symptoms. To be true, the team was not working in the dark. They were armed with a complete map of the genes, an understanding that two types of HLA (HLA-DQ2 and HLA-DQ8) predispose a person for celiac disease, and the very crucial recent discovery by a team of German colleagues that celiac patients have antibodies for a very precise enzyme: transglutaminase 2. "We also found that the bits of gluten that were presented to the T-cells have some changes caused by an enzyme in the body – transglutaminase 2", says Sollid. HLAs are proteins which act as markers, binding to fragments of other proteins, and telling T-cells how to treat them. So it wasn't much of a stretch for Professor Sollid's team to determine that the defective HLAs bind to fragments of gluten, causing the T-cells to treat them as bacteria or viruses. Basically, two HLA types present gluten remnants to the T-cells, causing the T-cells to regard the gluten as dangerous, and to trigger immune reactions that cause inflammation in the intestines, and this is what causes celiac disease. "We think that this is huge," Sollid said. "We understand the immune cells that are activated and why they are activated." At present, Professor Sollid and his group are investigating how antibodies against transglutaminase are formed. This is a simple, but huge moment in the annals of medicine and in the annals of celiac disease. It's a discovery that will help researchers develop new approaches to treatment, and/or a cure for celiac disease in the future. Source: Med.uio.no- 20 comments
-

German Researchers Chase Causes of Wheat Sensitivities
Jefferson Adams posted an article in Latest Research
Celiac.com 07/01/2016 - Between five to ten percent of Germans may suffer from wheat intolerance. These people suffer immune reactions when they eat wheat and other cereals such as spelt, rye, and barley. They suffer symptoms including diarrhea, fatigue, psychological disorders, and worsening of chronic inflammatory diseases. They may have celiac disease, wheat allergy, and non-celiac-non allergy wheat sensitivity (NCWS). Now doctors and biomedical and agricultural researchers at Johannes Gutenberg University Mainz (JGU) and the University of Hohenheim have joined forces to study these disorders, especially NCWS. They are gearing their research towards the breeding of new types of wheat that lack these disease causing properties, while maintaining favorable characteristics, such as good baking properties and palatability. The researchers have three main aims. Firstly, they want to find out how the content of wheat proteins called alpha-amylase-trypsin inhibitors (ATI's) has naturally evolved in the various wheat varieties. For this purpose, they are looking at whether there are differences in ATI content in older and newer varieties, the extent to which this is genetically determined in each variety, and whether environmental influences play a role. They also hope to establish exactly how many proteins belong to the family of ATIs in the wheat varieties examined and which of these proteins mainly cause the immune response. The harvested samples are thus being analyzed for ATI content by genetic and proteome methods, while human cell lines are being used to evaluate their immune system-activating effects in the laboratory. Lastly, the scientists hope to be able to establish how far ATI content affects baking properties and palatability, evaluating the wheat variants on the basis of standard quality criteria. Finally, and outside of the current proposal, "we plan several proof-of-concept clinical studies with patients that suffer from defined chronic diseases to assess how far a significant reduction of ATIs in the diet, for example by approximately 90 percent, may improve their condition," said Schuppan. The goal over the medium term is to use the findings to breed new varieties of wheat that sensitive population groups will better tolerate. "We thus need to get the balance correct and create wheat varieties with a low ATI content that still have good baking properties and palatability," concluded Longin. Source: eurekalert.org.- 3 comments
-
DQ8 Causes More Than Just Celiac Disease
Hallie Davis posted an article in Anemia and Celiac Disease
Celiac.com 08/18/2009 - Many of you know that DQ8 is one of the two major genes which may lead to celiac disease. You may also know that celiac disease is often associated with various other autoimmune diseases. What you may not know is that DQ8 may be the direct cause of these other autoimmune diseases, for these autoimmune diseases are found in increased incidence not just in celiac disease, but also with DQ8 itself. What follows is a list I have compiled showing the various diseases that are found in increased frequency among people who have the DQ8 gene (DQB1*0302). I will show the reference number next to each, and the corresponding references will appear below: Celiac disease (1) Scleroderma (2) Rheumatoid arthritis (1) Autoimmune thyroiditis (3) Pemphigus (4) Lupus (6) Pemphigoid (5) Focal myositis (7) Multiple sclerosis (8) Myasthenia gravis (1) Insulin dependant latent autoimmune diabetes of adults and adult Type 1 diabetes (9) Type 1 juvenile diabetes (1) Sjogren’s syndrome (10) Addisons’s disease (11) Complex regional pain syndrome with dystonia (12) Latex allergy (13) This list is not intended to be exhaustive. It is a starter list. Hopefully more research will be done on these, including carefully controlled research as to whether gluten plays any role in triggering these other autoimmune diseases even in the absence of gluten blood antibodies or positive duodenal biopsies. I, for one have DQ8 and numerous of these autoimmune diseases, even though my gluten blood antibodies and duodenal biopsies are negative. We who have this gene need to know for certain #1 whether a gluten free diet will help prevent the triggering of these other various autoimmune diseases, and #2 whether a gluten-free diet will help mitigate autoimmune symptoms that have already developed. I feel no better on the gluten-free diet than before I started it a year and a half ago. However, if I had not been on the diet, perhaps I would be feeling even worse now. Only controlled research will give us the answer.References: http://en.wikipedia.org/wiki/HLA-DQ8 Autoantibodies to fibrillarin in systemic sclerosis (scleroderma). An immunogenetic, serologic, and clinical analysis. Frank C. Arnett, MD, John D. Reveille, MDet al. See abstract at http://www3.interscience.wiley.com/journal/112212324/abstract. A strong association between thyrotropin receptor-blocking antibody- positive atrophic autoimmune thyroiditis and HLA-DR8 and HLA-DQB1*0302 in Koreans. Cho, JH Chung, YK Shong, YB Chang, H Han, JB Lee, HK Lee and CS Koh. See abstract at http://jcem.endojournals.org/cgi/content/abstract/77/3/611. Association between HLA-DRB1, DQB1 genes and pemphigus vulgaris in Chinese HansBy Zhou SH, Lin L, Jin PY, Ye SZ. See abstract at: http://www.ncbi.nlm.nih.gov/pubmed/12579512. Polymorphisms of HLA-DR and -DQ Genes in Japanese Patients with Bullous Pemphigoid. By Okazaki A, Miyagawa S, et al. See abstract at: http://sciencelinks.jp/j-east/article/200017/000020001700A0339663.php. HLA-DRB1*03 and DQB1*0302 associations in a subset of patients severely affected with systemic lupus erythematosus from western India. By U Shankarkumar, K Ghosh, S S Badakere, D Mohanty. See abstract at: http://ard.bmj.com/cgi/content/extract/62/1/92. HLA typing in focal myositis. By Kenji Sekiguchi, Fumio Kanda, Kenichi Oishi, Hirotoshi Hamaguchi, Kenichiro Nakazawa, Nobuya Maeda, Hiroyuki Ishihara and Kazuo Chihara. See abstract at: http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6T06-4DB5B4F-1&_user=10&_rdoc=1&_fmt=&_orig=search&_sort=d&_docanchor=&view=c&_searchStrId=975695599&_rerunOrigin=google&_acct=C000050221&_version=1&_urlVersion=0&_userid=10&md5=36883393fca9b990607eeb0d38116c5a. HLA-DRB1*1501, -DQB1*0301, -DQB1*0302, -DQB1*0602, and -DQB1*0603 alleles are associated with more severe disease outcome on MRI in patients with multiple sclerosis. By Zivadinov Robert; Uxa Laura et al. See abstract at: http://www.biomedexperts.com/Abstract.bme/17531857/HLA-DRB1_1501_-DQB1_0301_-DQB1_0302_-DQB1_0602_and_-DQB1_0603_alleles_are_associated_with_more_severe_disease_outcome. Similar Genetic Features and Different Islet Cell Autoantibody Pattern of Latent Autoimmune Diabetes in Adults (LADA) Compared With Adult-Onset Type 1 Diabetes With Rapid ProgressionBy Nóra Hosszúfalusi, MD, PHD, Ágnes Vatay, MD1, et al. See abstract at http://care.diabetesjournals.org/content/26/2/452.full. Specific amino acid residues in the second hypervariable region of HLA- DQA1 and DQB1 chain genes promote the Ro (SS-A)/La (SS- autoantibody responses. ByJD Reveille, MJ Macleod, K Whittington and FC Arnett. See abstract at http://www.jimmunol.org/cgi/content/abstract/146/11/3871. Analysis of extended human leukocyte antigen haplotype association with Addison’s disease in three populations. ByGombos, Hermann, et al. See study at: http://www.eje-online.org/cgi/reprint/157/6/757.pdf. HLA-B62 and HLA-DQ8 are associated with Complex Regional Pain Syndrome with fixed dystonia. By Rooij, Gosso, et al. See study at: http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6T0K-4WH0JWP-2&_user=10&_rdoc=1&_fmt=&_orig=search&_sort=d&_docanchor=&view=c&_rerunOrigin=google&_acct=C000050221&_version=1&_urlVersion=0&_userid=10&md5=c869b6d3a38081820fad17c162b510ba. HLA-DQ8 and the HLA-DQ8-DR4 haplotype are positively associated with the hevein-specific IgE immune response in health care workers with latex allergy. By Rihs Hans-Peter; Chen Zhiping; Ruëff Franziska; et al. See abstract at: http://www.biomedexperts.com/Abstract.bme/12209103/HLA-DQ8_and_the_HLA-DQ8-DR4_haplotype_are_positively_associated_with_the_hevein-specific_IgE_immune_response_in_health_c -
Celiac.com 03/18/2009 - A recent study used lactulose hydrogen-breath assays to show that small intestine bacterial overgrowth (SIBO) is likely a routine cause of non-responsive celiac disease. A team of researchers from the Mayo Clinic College of Medicine recently set out to assess the rates and significance of SIBO in celiac disease based on the results of quantitative culture of intestinal aspirate. The team was made up of Alberto Rubio-Tapia, M.D., Susan H. Barton, M.D., Joseph A. Murray, M.D., of the Mayo’s Division of Gastroenterology and Hepatology, and Jon E. Rosenblatt, M.D., of the Mayo’s department of Laboratory Medicine and Pathology. Their efforts were supported by the American College of Gastroenterology (ACG) International Training Grant 2006 (ART) and the NIH grants DK-57892 and DK-070031 (JAM). Currently, the rate of SIBO in celiac disease diagnosed by quantitative culture of intestinal aspirate is not known. The team set out to assess the rate and determine the significance of SIBO in celiac disease based on the results of quantitative culture of intestinal aspirate. The team set out to examine the causes of non-responsive celiac disease by looking at people with celiac disease in whom culture of intestinal aspirate was assessed for the presence of both aerobic and anaerobic bacteria. They defined bacterial overgrowth as culture >105 colony forming units/mL. In all, they evaluated 149 people with biopsy-confirmed celiac disease. They took intestinal aspirate samples from 79 (53%) patients with non-responsive celiac disease, 47 (32%) as initial work-up for mal-absorption, and in 23 (15%) with asymptomatic treated celiac disease. The team diagnosed 14 cases of SIBO (9.3%), nine cases of non-responsive celiac disease (11%), five cases at initial work-up for mal-absorption (11%), and 0 cases in asymptomatic treated celiac disease. Patients with a positive culture showed signs of worse mal-absorption. 67% of patients with both non-responsive celiac disease and bacterial overgrowth showed a coexistent disorder. The results showed that nearly 1 in 10 celiac patients had SIBO as diagnosed by quantitative culture of intestinal aspirate (9.3%). This figure included both patients with symptomatic treated or untreated celiac disease. This shows that SIBO may exist along with other maladies associated with non-responsive celiac disease. Journal of Clinical Gastroenterology: Volume 43(2)February 2009pp 157-161
- 4 comments
-
Am J Gastroenterol. 2002 Aug;97(8):2016-21 Celiac.com 01/29/2004 - According to researchers at the Mayo Clinic in Rochester Minnesota, the main causes of non-responsive celiac disease are: "1) gluten contamination is the leading reason for non-responsive celiac disease; 2) of non-responsive celiac disease cases, 18% are due to Refractory Sprue; and 3) alternative diseases or those coexistent with celiac disease and gluten contamination should be ruled out before a diagnosis of Refractory Sprue is made." The researchers define Refractory Sprue as "failure of a strict gluten-free diet to restore normal intestinal architecture and function in patients who have celiac-like enteropathy," and conducted a study to determine possible causes, including how many people actually have Refractory Sprue compared with how many are diagnosed with it. The researchers examined the medical records of 55 patients who were, between 1997 and 2001, presumed to have non-responsive celiac disease, six of which were later found not to have celiac disease. Of the 49 remaining patients 25 were identified as having gluten contamination in their diet. The researchers add: "Additional diagnoses accounting for persistent symptoms included: pancreatic insufficiency, irritable bowel syndrome, bacterial overgrowth, lymphocytic colitis, collagenous colitis, ulcerative jejunitis, T-cell lymphoma, pancreatic cancer, fructose intolerance, protein losing enteropathy, cavitating lymphadenopathy syndrome, and tropical sprue." I think that it is clear that if you have celiac disease and continue to have symptoms your first step should be to look closely at your diet for any possible gluten contamination. Your next step should be eliminating other common food intolerance items such as cows milk, soy, eggs or corn. -Scott Adams
-

Swedish Study on the Causes of Death in Celiac Disease Patients
Scott Adams posted an article in Latest Research
Arch Intern Med. 2003;163:1566-1572. Ulrike Peters, PhD, MPH; Johan Askling, MD; Gloria Gridley, MS; Anders Ekbom, MD, PhD; Martha Linet, MD Celiac.com 07/30/2003 - The following abstract paints a fairly bleak picture for those of us with celiac disease; however, after taking a closer look at it I believe that it has some serious limitations that should not be overlooked, and have likely produced skewed or irrelevant results. For example, the study does not indicate whether or not the patients in it followed a strict gluten-free diet. Other studies have shown that the mortality risk for celiacs decreases to that of the normal population when a gluten-free diet is followed for at least five years, and that it is also affected by how soon the diagnosis is made and how soon treatment begins. It is well known that not following a gluten-free diet will increase a celiacs risk of death by many causes to many times that of the normal population, which is precisely why it is so important to include such information in studies of this type. In my opinion doing a study like this and not including such data is like doing a study on diabetes where perhaps half or more people in the study do not take insulin but ought to, and then publishing the ultra-high mortality rate that would be its outcome: "Conclusion: Diabetics have a 20-fold mortality rate over the normal population." The conclusion would clearly not be true for those who took their insulin. Additionally the time period that is covered by this study, 1964-1993, could be considered the dark ages of celiac disease, even in Europe (we actually may be just entering the Renaissance age for celiac disease here in the USA, but this could be argued!). Many doctors during this time did not stress enough to their patients the importance of following a strict gluten-free diet, just as many still do not even do this day. My doctor didnt. He just diagnosed me and said I shouldnt eat gluten (as opposed to telling me that it could kill me if I kept eating it), and he didnt even explain to me HOW to avoid it! Is it possible that some of the folks in this study, diagnosed as far back as 1964, might have had similar experiences with their doctors? I would be willing to bet that at least 50% of the people in this study (if not more) were not following a strict gluten-free diet, or were not following the diet at all. If this is true, it is kind of like studying a group of diabetics whose only treatment was to be told by their doctors that they should avoid sugar, which seems absurd if you think about it. Last, the study has considerable bias in that it recruited only hospitalized celiacs, presumably because they were already significantly ill, and those who never made it into a hospital were excluded. It reports findings of auto-immune diseases and small bowel/lymphomaexcesses--these are already well known--but what other researchers may disagree with is the scale of the excess--SMR is always a very crude method ofexpressing this in such studies. - Scott Adams (special thanks to Dr. Geoff Helliwell for his comments on this study) Abstract: "Background: Patients with celiac disease have an increased risk of death from gastrointestinal malignancies and lymphomas, but little is known about mortality from other causes and few studies have assessed long-term outcomes." "Methods: Nationwide data on 10,032 Swedish patients hospitalized from January 1, 1964, through December 31, 1993, with celiac disease and surviving at least 12 months were linked with the national mortality register. Mortality risks were computed as standardized mortality ratios (SMRs), comparing mortality rates of patients with celiac disease with rates in the general Swedish population." "Results: A total of 828 patients with celiac disease died during the follow-up period (1965-1994). For all causes of death combined, mortality risks were significantly elevated: 2.0-fold (95% confidence interval [CI], 1.8-2.1) among all patients with celiac disease and 1.4-fold (95% CI, 1.2-1.6) among patients with celiac disease with no other discharge diagnoses at initial hospitalization. The overall SMR did not differ by sex or calendar year of initial hospitalization, whereas mortality risk in patients hospitalized with celiac disease before the age of 2 years was significantly lower by 60% (95% CI, 0.2-0.8) compared with the same age group of the general population. Mortality risks were elevated for a wide array of diseases, including non-Hodgkin lymphoma (SMR, 11.4), cancer of the small intestine (SMR, 17.3), autoimmune diseases (including rheumatoid arthritis [sMR, 7.3] and diffuse diseases of connective tissue [sMR, 17.0]), allergic disorders (such as asthma [sMR, 2.8]), inflammatory bowel diseases (including ulcerative colitis and Crohns disease [sMR, 70.9]), diabetes mellitus (SMR, 3.0), disorders of immune deficiency (SMR, 20.9), tuberculosis (SMR, 5.9), pneumonia (SMR, 2.9), and nephritis (SMR, 5.4)." "Conclusion: The elevated mortality risk for all causes of death combined reflected, for the most part, disorders characterized by immune dysfunction." -
The following is a list of causes of flattened villi which was published in a book titled Coeliac Disease by W. T. Cooke and G. K. Holmes, published by Churchill Livingstone, Medical Division of Longman Group Limited (1984). Celiacs on a gluten-free diet (for a prolonged period) who continue to have flatten villi may be want to look for other causes to their problem. Keep in mind that some of the items listed rarely cause flatened villi, and are usually found in conjunction with Celiac Disease or immuno-deficiencies. Coeliac Disease Cows Milk Protein Intolerance Soy Protein Intolerance Refractory Sprue Collagenous Sprue Immunodefiency Synodromes Mediterranean Lymphoma Intestinal Ulceration Gastroenteritis Intractable Diarrhoea of Infancy Protein Calorie Malnutrition Kwashiorkor Tropical Sprue Parasitic Disease: Giardiasis Strongyloidiasis Coccidiosis Intestinal Capillariasis Hookworm Disease Eosinophilic Gastroenteritis Contaminated Bowel Syndrome Drug and Radiation Damage
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8-M):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8-M):