-
Welcome to Celiac.com!
You have found your celiac tribe! Join us and ask questions in our forum, share your story, and connect with others.
-
Celiac.com Sponsor (A1):
Celiac.com Sponsor (A1-M):
-
Get Celiac.com Updates:Support Celiac.com!
Search the Community
Showing results for tags 'inflammation'.
-
Hello everyone, I was diagnosed with celiac disease at the end of September 2023 and immediately started the gluten-free diet. Ever since I was a little girl, I've often been ill, and throughout my childhood I was underweight and severely deficient in iron and vitamin D in particular. In my pre-adolescence, I began to have difficulty standing, running etc., and after more than a year of tests and X-rays, no diagnosis could be made. Fortunately, in adolescence it went away on its own. The doctors never really understood why I was so often ill as a child. I changed doctors and treatments several times, but nothing helped. Around the age of 14, I started to lose a lot of my hair, and by the age of 18 I had severe alopecia. Several years later I had an event in my life that deeply affected me and I suffered a great deal of stress for a long time, since when I've also started to lose my eyebrows. After a major eyebrow loss this summer, I decided to do something about all this and understand what is going on with me. After a lot of research, I realized that I might have celiac disease. I was diagnosed with the disease in September and my gastroenterologist has put me on a strict diet which I follow to the letter (I eat almost no processed foods and those I do eat rarely I check for contamination). However, I don't feel that my symptoms are improving. True, I no longer have a constant gut ache or dizziness, but apart from that, my acne is still present and has even worsened, my hair and eyebrows don't seem to be improving (I still loss lots of them) and I'm constantly tired. I have a diet where I eat very little dairy, lots of protein and fruits, vegetables, oilseeds, etc.. I'm 6 months into a gluten-free diet, how long did it take you to see your skin, hair and fatigue improve for those who also had these symptoms in particular? Thank you very much
- 12 replies
-
- acne
- alopecia areata
- (and 8 more)
-
Celiac.com 08/15/2023 - Researchers from the University of Otago in New Zealand recently studied the effects of dietary wheat gluten on the hypothalamus of male mice. The researchers include Mohammed Z. Rizwan, Romy Kerbus, Kaj Kamstra, Pramuk Keerthisinghe, and Alexander Tups. Their findings are intriguing. The researchers are variously affiliated with the Centre for Neuroendocrinology and Department of Physiology at the University of Otago School of Biomedical Sciences in Dunedin, New Zealand; the Centre for Neuroendocrinology and Department of Anatomy at the University of Otago School of Biomedical Sciences in Dunedin, New Zealand, and the Maurice Wilkins Centre for Molecular Biodiscovery in Auckland, New Zealand. Gluten is commonly found in wheat, rye, and barley, and is a major dietary component in many western countries. Gluten has been linked to weight gain and peripheral inflammation in mice. This research aimed to understand its impact on central inflammation, particularly in relation to diet-induced obesity. Low-fat Diet vs. High-fat Diet with Gluten The study observed that adding gluten to a low-fat diet had no discernible effect, but male mice fed a high-fat diet enriched with gluten exhibited increased body mass and adiposity compared to those on an high-fat diet without gluten. Additionally, when gluten was introduced to the low-fat diet, it led to higher levels of circulating C-reactive protein. Interestingly, it made no difference whether gluten was added to a low-fat or a high-fat diet. Either way, it triggered a significant increase in the number of microglia and astrocytes in the arcuate nucleus of the hypothalamus. These changes were identified using specific markers through immunohistochemistry. Even on an low-fat diet, gluten appeared to replicate the immunogenic effects seen with an high-fat diet, and its inclusion in the latter led to a further rise in the number of reactive immune cells. Gluten Triggers an Obesity and Injury to the Hypothalamus Overall, the findings suggested that gluten had a moderate obeso-genic effect, when given to mice exposed to an high-fat diet. Moreover, the study reported that gluten triggered the presence of astrocytes and microglia in the hypothalamus, indicating a potential injury to the hypothalamus in rodents. Mice are used in studies to model human disease risk due to genetic similarities, allowing researchers to investigate potential factors and develop treatments in controlled, ethically manageable settings. This research contributes to our understanding the complex relationship between dietary components, like gluten, and obesity-related inflammation in the brain. It also offers up some exciting areas of further research inquiry into the brain's response to gluten in both mice and humans. Read more in the Journal of Neuroendocrinology
- 2 comments
-
Celiac.com 06/01/2023 - The rising popularity of gluten-free diets has captured public attention in recent years. With claims of weight loss, improved digestion, and increased energy, many individuals have jumped on the gluten-free bandwagon. However, it's important to base dietary decisions on scientific evidence, rather than mere trends. To shed some scientific light on the subject, a team of researchers conducted a controlled study to investigate the effects of gluten intake on body weight, body composition, resting energy expenditure, and the changes in nutrient intake caused by gluten-free diets. Study on Effects of Gluten Intake The research team included Hirla Karen Fialho Henriques, Luana Moreira Fonseca, Karine Silva de Andrade, Nitin Shivappa, James R. Hébert, Adaliene Versiani Matos Ferreira & Jacqueline Isaura Alvarez Leite. They are variously affiliated with the Department of Biochemistry and Immunology - ICB, Federal University of Minas Gerais, Belo Horizonte, Brazil; the Department of Nutrition, School of Nursing, Federal University of Minas Gerais, Belo Horizonte, Brazil; the Department of Biochemistry and Immunology - ICB, Federal University of Minas Gerais, Belo Horizonte, Brazil; and the Cancer Prevention and Control Program, University of South Carolina, Columbia, South Carolina, USA. Their study enrolled twenty-three women, who adhered to a gluten-free diet for a duration of six weeks. During this period, the participants were provided with muffins containing either 20 grams of gluten isolate (known as the gluten period) or gluten-free muffins (the gluten-free period) in a crossover, single-blind, non-randomized trial. The researchers assessed the subjects' habitual diet, including gastrointestinal symptoms, food frequency questionnaires, body composition, resting energy expenditure, and recorded daily food intake for the entire six-week duration. The Findings - Increase in Fat and Sodium Intake Surprisingly, the data showed that body weight, body composition, gastrointestinal symptoms, and resting energy expenditure remained similar during both the gluten and gluten-free periods. These results indicate that consuming up to 20 grams of gluten per day does not affect body weight or composition in healthy women without caloric restriction, at least over a relatively short period of three weeks. However, the team saw some concerning changes when the nutrient composition of the gluten-free period was compared to the participants' habitual diet. The gluten-free diet led to an increase in fat and sodium intake, while reducing the intake of fiber, as well as vitamins B1, B6, B12, and folate. This imbalance in nutrient intake resulted in an elevated dietary inflammatory index, indicating a higher inflammatory potential associated with gluten-free diets. These findings highlight the importance of considering the overall nutritional quality of a diet, rather than focusing solely on the absence of gluten. While a gluten-free diet may be necessary for individuals with specific medical conditions, such as celiac disease, the results suggest that adopting a gluten-free diet without medical necessity may have adverse effects on nutrient intake and potentially contribute to inflammation. The study offers some potentially valuable insights into the impact of gluten intake and gluten-free diets on health, especially with regards to nutrient intake, but it's important to note that it has certain limitations. The small sample size and the short duration of the trial invite further research with larger populations and longer intervention periods, to validate and expand upon these findings. Additionally, the study focused solely on healthy women, so the results may not be generalizable to other populations, or those with specific health conditions. It's also important to note that following a gluten-free diet can lead to imbalances in nutrient intake, particularly a reduction in fiber and essential vitamins, and an increase in dietary inflammation potential, even in non-celiacs. As with any dietary decision, it's best to consult with a healthcare professional or registered dietitian to ensure a well-rounded and nutritionally adequate diet that suits individual needs. Read more in the J Am Nutr Assoc. 2022 Nov-Dec;41(8):771-779.
- 5 comments
-
Celiac.com 02/20/2023 - Celiac disease is a condition that is caused by the immune system's response to gluten, a protein found in wheat, rye and barely. In celiac patients, an immune response triggers a pro-inflammatory environment in the small intestine, causing damage to the tissue. A major role in the pathogenesis of celiac disease is played by the HLA-restricted gliadin-specific intestinal T-cell response generated in a pro-inflammatory environment. A recent review article highlights the growing body of research that supports the central role of inflammation in the development of celiac disease, and how it is influenced by factors such as sensitivity to gluten and other pro-inflammatory agents. The review is authored by researchers Maria Vittoria Barone, Renata Auricchio, Merlin Nanayakkara, Luigi Greco, Riccardo Troncone, and Salvatore Auricchio. The are variously affiliated with the Department of Translational Medical Science, University Federico II in Naples, Italy; and the European Laboratory for the Investigation of Food Induced Disease (ELFID), University Federico II in Naples, Italy. Live studies on a population at risk have explored the mechanisms behind this inflammation. These studies show cellular and metabolic alterations in the absence of a T cell-mediated response, before the onset of the disease and before the introduction of gluten in the diet. Gluten exacerbates these constitutive alterations, both live and in the lab. The role of inflammation in celiac disease has led researchers to consider it as a chronic inflammatory disease, similar to other autoimmune disorders. The review also explores the crucial role played by the intestine in controlling inflammation both locally and systemically, and the impact of nutrients and gut bacteria on inflammation. Reduction of Early Inflammation Could Delay Onset of Celiac Disease Celiac disease is characterized by inflammation, which plays a critical role in the onset of the disease. It begins with a pre-clinical phase where the body is set up for inflammation, making it susceptible to various pro-inflammatory agents, including gluten. Historically, research has focused on the T-cell response in celiac disease, but there is growing recognition of the importance of the pre-inflammatory state. Modulating this state with a Mediterranean-type diet or preventing intestinal viral infections could have a significant impact on the onset of celiac disease, and could be easier to manage than the more complex autoimmune response. The implications of this research extend to additional chronic inflammatory diseases including inflammatory bowel diseases and diabetes, where early intervention with the state of inflammation in at-risk subjects could have a lasting impact on their health. Read more in mdpi.com
- 1 comment
-
- causes
- celiac disease
- (and 8 more)
-
Inflammation Model for Sickness Beginning with B-Vitamin Deficiency in Celiac's and other Inflammation triggered diseases…. AKA The LUPUS Inflammation Model or How the ignorance about nutrition is killing us today or how and why B Vitamins are being diagnosed as genetic GI diseases like Celiac disease today Note to blog reader :::::::) I get in the weeds sometimes...If you decide to read this anyway...don't say I didn't warn you.... from an earlier correspondence with Scott who said It would be ok? to post here in the blog area of Celiac.com I did this research originally for myself and how the pieces finally came together....and now posting here below my collected thoughts on this research I have done over the years...here goes nothing...with everything that is going on with COVID-19... It seemed the right time to post it....... Since the day I was diagnosed as a Celiac patient 12+ years ago I began to see if I could confirm my diagnosis or come to the same conclusion based on the current available research. It is said knowledge is power and ignorance kills or at least maims us in this case...the ignorance about nutrition in the medical field is striking because genetics and environment mix/intersect with B-Vitamins. I choose early on in my research the Capstone B-Vitamin --- Niacin because it has been linked to building stomach acid in the body....it was an easy choice I thought but as I begin to make this argument it was apparent .... this model had some holes in the barrel.... Meaning while some Celiac's can/do develop Celiac disease (in time) ...it did explain the majority of the cases. You can read the original article here... Now with two years more study the clinical picture has become more distinct. I choose capstone disease...not the Cornerstone disease. A good model is predictive (or should be)....Pellagra predicts the 25 to 30 pct of those that get DH....so I was only 1/4 to a 1/3 right? It didn't cover the 2/3 of Celiac's who the IJCD in 2015said might go one to develop Pellagra.... and what encourage me to begin talking about Pellagra as a differential diagnosis. First published 5 years ago in the IJCD http://pubs.sciepub.com/ijcd/3/1/6/index.html I made the same mistake the did....I believe they identified Pellagra Sine Pellagra aka a Riboflavin deficiency as Pellagra instead. Which is an honest mistake even for seasoned researchers because one mimics the other.... In fact, because it is a cascade reaction....one stone build’s upon the other...B-Vitamins don't happen in an uncomplicated matter. If you have developed Pellagra a Niacin deficiency you have already developed Pellagra Sine Pellagra (hereafter) PSP a Riboflavin deficiency. Pellagra is like……a 3 alarm fire.....if you have it....everybody else knows you are sick....because the raging nutritional fire in your body has broken out to the surface...and you have terrible skin rashes....IE DH etc.... The main difference between PSP and Pellagra is the level of skin involvement..... PSP only develops skin rashes at junctions of the skin like gentalia, corners of mouth, folds of the skin etc... You might also have hives or various not my hair/skin is on fire itching.....just whelps not itchy ones... Today this might be called a MCAS disease 15+ years ago Prousky proved this a Niacin deficiency orthomolecular.org/library/jom/2002/pdf/2002-v17n01-p017.pdf Then known as a Histadelia or known today as a Histamine Intolerance But this the Capstone nutrient and only a 1/3 of Celiac's will ever develop DH. By now you won't be able to develop any stomach acid.... https://www.ncbi.nlm.nih.gov/pubmed/3992169 Studied 30+ years ago.....NO stomach acid leads to DH.... But other things have happened before this happens.....Like the low Riboflavin that has triggered your PSP. We know it is PSP because organs other than your GI system is involved like your Thyroid for example.... Low Riboflavin levels leads to low thyroid production.... In fact, the bodies ability to synthesize it's own Thyroxine can be/is a sign your body is now low in Riboflavin... https://www.ncbi.nlm.nih.gov/pubmed/3809170 And why in part....Celiac develops/affect multiple organ systems because you have multiple vitamin deficiencies.... Like a web of life....deficiencies are connected in a cascade/feedback loop. ONCE this feedback loop is broken your immune system begins attacking itself triggered by gluten.... The 64K question is how do we stop this auto-immune reaction from happening in the first place or can we? If Celiac disease involves a trigger like gluten to set it off....I believe we can...it is Epigenetics.... and something that is not well understood today...even Genetics have a trigger... we see this in many ways like how stress in Spouses of Celiac's make them have a higher rate of diagnosis even without Celiac genes??? The environment is the trigger! The hormone matters site does a good job of summarizing this... https://www.hormonesmatter.com/mitochondria-energy-not-genetics-underlies-health-disease/ yet we tend to think disease is 70pct genes and only 30pct environment when it much closer to 50/50 for Celiac disease. The latest research confirms this hypothesis.... https://www.genengnews.com/news/dna-has-relatively-little-say-in-disease-risk-usually/ quoting.... "Notice that Wishart referred to most diseases. According to Wishart and colleagues, these include many cancers, diabetes, and Alzheimer’s. In fact, for such diseases, the genetic contribution to disease risk is just 5–10%. There are diseases, however, for which the genetic contribution is about 40–50%. These diseases include Crohn’s disease, celiac disease, and macular degeneration." Now let's see if can see why this is? We know from previous research on air pollution B-Vitamins help us fight the negative effects of our environment .... down regulating our Immune System... https://www.sciencedaily.com/releases/2017/04/170412111211.htm And why taking B-2 or B-3 can help those in the 2nd or 3rd phase of Celiac disease.... But yet we still have not reached the "Cornerstone" Nutrient... Remember this a complex biological system we are dealing with --- one deficiency effects the other deficiencies.... So, we need an analysis (model) that can determine the capstone from the cornerstone....like I confused them and the IJCD did? If this updated hypothesis (Model) is correct? WE know B1, B2, and B3 work together to control our immune system because their synergistic effect has been studied together. https://www.ncbi.nlm.nih.gov/pubmed/30903555 B1, B2, and B3 together protects us from our immune system. But this doesn't tell us what (which of the B-Vitamins) is the trigger? we just know which ones it is.... if our analysis is right and it is a combination of factors/nutrient deficiencies depending on the phase of the disease... But we do know they work in a synergistic way.... We now know and can reasonably conclude stress and the resultant inflammation is the trigger for our Celiac disease in a 50/50 manner.... Let' look at other associated diseases to see if they can help us? Often Celiac is said to have many wicked sister/associated diseases and in our simplicity we like of them as separate diseases.... but an elegant model says/sees a connection (explains) their association. This "Inflammation" model explains how Celiac disease can have many different "faces" or show up in other associated diseases like Lupus as an example....because we only have ONE inflammation model in the body....presenting (being diagnosed with diffuse symptom's in other diseases) all related to Celiac disease....because they are in different phases of the disease IE Celiac disease... or Pellagra or PSP or LUPUS because it is the same "Inflammation" model. This ordered step by connection has been worked out for Lupus recently and why Lupus shows up as an associated disease of Celiac disease because they are the same inflammation model. https://www.eurekalert.org/pub_releases/2019-09/uoaa-hia091319.php We know the same Interleukins involved in Lupus are also involved in Celiac disease which is instructive too us if they are are the same disease in different stage/phases with different faces... The reason Celiac disease has 200+ symptom's because our body uses the same Kyneurine Pathway to develop Niacin.... and by the time Pellagra show up we really are half dead...(Metabolically) speaking....this connection has been established in human diseases effecting nearly every organ system in the body.....because Inflammation shows up everywhere in time... after this pathway breaks down... https://www.ncbi.nlm.nih.gov/pubmed/22084578 But what start/triggers the break? If it is not Niacin as the Capstone nutrient? (I will skip over the discussion of B-2 for brevity purposes (which deserves it's own paper) and skip down to the Cornerstone nutrient.....Thiamine aka Vitamin B1 Think of your body like an engine for a moment....every ICE (Internal Combustion Engine) has a Top Dead Center (TDC) IE firing order etc....the way the engine runs smoothly and in tune...mess with the firing sequence... and the engine won't run at alll......and the same is so for the Krebs’s cycle... It is a robust but fragile cycle that let's make our own energy from our food....like chlorophyll for photosynthesis.... Magnesium and Thiamine are the TDC of the Krebs cycle... (Again to make this short as possible I will not elaborate on the role Magnesium plays in this analysis but only mention in passing (like a spark plug) for analogy purposes the engine won't run without gas....and magnesium acts like a spark plug/catalysis for us to use our Thiamine (gas) for energy in the cell).... Lonsdale says Magnesium and Thiamine are the keys to disease... https://www.ncbi.nlm.nih.gov/pubmed/25542071 This analysis is based on the key neurotransmitter Acetylcholine that regulates our biofeedback system in the body that triggers our immune system in the body. Note: to Celiac.com forum/blog readers much of the above was written free hand...as I collected my thoughts some of the remaining thoughts have been shared first with Ch88 or Knitty Kitty and EnnisTx (in a piece meal fashion) haven written these thoughts out before (but not shared publicly) I am collecting them here for others to research, test out and prove, contest and confirm with more research... but consider it as always (2 Timothy 2:7) and the Lord give you understand (and have your medical experts (doctor's)) review this idea as plausible.... This analysis stands and falls on Acetylcholine....and how we can't make it without Thiamine... when we get low in thiamine ...the acetylcholine (link) is what breaks...that put's our body in an alarm state... but we get low in thiamine FIRST... the low thiamine causes thin villi and leads to lactose intolerance etc... see this research entitled "Effect of dietary thiamin deficiency on intestinal functions in rats. " https://www.ncbi.nlm.nih.gov/pubmed/6465054 the role of acetylcholine was recently confirmed as the triggering mechanism to alert our body to go into alert mode or auto-immune mode by triggering inflammation in our tissues/organs etc.. https://www.medicalnewstoday.com/articles/321624.php and how the use of Baking Soda can help tame this auto-immune effect by turning off this alarm mode for the body... Baking Soda can mitigate this alarm mode by triggering the stomach to produce more stomach acid... And since acetylcholine is one of three triggering mechanism in the stomach in the production of stomach acid along with Histamine they (and gastrin ) I believe regulate when we produce stomach acid and why being low in thiamine lead to be low in stomach acid...but not completely disabling our stomach acid production....Niacin does that... But we are in limp home mode at this point... and auto-immune system is now triggered... Because Thiamine is used in the synthesis of Acetylcholine and it's role in the Parasympathetic Nervous System organs through out the whole body are affected... See this Wikipedia figure that expands how this simple neurotransmitter is used in multiple organs in the body not just the brain (at the name implies) https://en.wikipedia.org/wiki/Acetylcholine#/media/File:1503_Connections_of_the_Parasympathetic_Nervous_System.jpg since Acetylcholine is used by the intestines to regulate our smooth muscle tissues (think peristalsic action of GI tract) often times the GI tract is the first place people notice it...medical definition of peristalsis.... "the wormlike movement by which the alimentary canal IE (the GI tract) or other tubular organs with both longitudinal and circular muscle fibers propel their contents, consisting of a wave of contraction passing along the tube" see this great overview on how thiamine effects the body...on the health supplements guide website... https://healthsupplementsnutritionalguide.com/vitamin-b1/ quoting how Acetylcholine is used to regulate key organ systems including the Brain, Heart and GI tract.... "11. used by the nervous system to ensure normal muscle tone of the heart, stomach and intestines" causing intermittent constipation and diarrhea... People don’t' put 2+2 together because we think these complex systems are acting independently but the Parasympathetic Nervous system (as a neurotransmitter acetylcholine) connects them all... But this research shows how low thiamine status leads to an interruption of Acetylcholine production by the body... and not surprisingly it is 30 years old and a generation has forgot about it...entitled "Impairment of acetylcholine synthesis in thiamine deficient rats developed by prolonged tea consumption" https://www.sciencedirect.com/science/article/abs/pii/0024320584906258 For must humans we don't consume enough "sweet" tea to trigger this ...but more than 6 to 8 or more cups of coffee a day... could do it..as an example.... The reason most humans develop Beri Beri is a high CARB load....not just high wheat etc.... Anybody that (is lacking protein in a well balanced diet) could on a high (SAD) diet could develop Beri Beri (fatigue etc.) PSP (thyroid problems) Skin Issues (DH, Pellagra etc.)...as the diseases pile on ever more symptom's... Pharmacy Times has a nice article about Thiamine, Magnesium and Obesity on this topic.... https://www.pharmacytimes.com/contributor/adam-remick/2018/07/thiamine-and-magnesium-in-obesity-a-possible-factor-in-disease-prevention-and-co-treatment this article has a nice overview as well... https://www.eonutrition.co.uk/blog/thiamine-deficiency-a-major-cause-of-sibo In fact, up to a 1/3 of patients obese enough to have gastric bypass surgery due to an over reliance to CARBS in their diet triggering sub-clinical Beri Beri... https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4352173/ Now people (Celiac's) just need to get tested for it....to confirm this analysis??? But be aware tests can be tricky...because they often test for the wrong things...It is much quicker to take a high quality supplement like Benfotiamine than to confirm a Beri Beri diagnosis because the symptom's are so diffuse and common in other diseases today the doctor's don’t' recognize Beri Beri anymore as a separate disease unless you are drinking... Here are more resources from the hormones matters website that might be helpful to you... http://www.hormonesmatter.com/thiamine-deficiency-testing-understanding-labs/ https://www.hormonesmatter.com/navigating-thiamine-supplements/ As I told EnnisTx....doctor's are much more likely when your 1/3 to a 1/2 dead today like in emergency room today... https://www.sciencedirect.com/science/article/pii/S0872817813001197 When diagnosed in Celiac's ....they term it a "rare" condition (as usual) because they rarely recognize it today ... and even Celiac's have a claim too it .....it is called a Celiac Crisis.... I say it is a crisis today that B-Vitamins deficiencies like Thiamine, Riboflavin, and Niacin are not being diagnoses and worse tested for these deficiencies so the real rate of this high calorie malnutrition is being diagnosed and treated so people can get better from these (often) misdiagnosed disease in Celiac disease.... Beri Beri being the Cornerstone for the Cascade (house of cards) to come tumbling down. I know it was in my case....burning feet (pins and needles), Creatine in Kidneys, Angular Cheilitis, begins of a thyroid problems, chronic fatigue, low stomach acid, lingering constipation and diarrhea, Low T, chronic fatigue all got better with a B-complex and/or B-1, B-2 and B-3 supplementation.... And I now know after 12+ years of research that low Thiamine was the beginning of the cascade causing thin Villi, leading in time to Leaky Gut... I hope this is helpful....share with as many Celiac experts as you think would listen, this is about educating others...."For to Educate is to Free" Tests need to be done to confirm the years of research I've done so it can benefit other still suffering.... and all I ever wanted to do.... I just hope it is not another 20+ years before doctor's begin testing for these nutritional deficiencies in Celiac's... 2 Timothy 2: 7 “Consider what I say; and the Lord give thee understanding in all things” this included. Posterboy by the Grace of God, Note: For the intrepid reader still reading this blog post....I have tried to make this as exhaustive as possible (but you can stop reading now if you want) what follows is additional resources added later (after I composed this blog post/originally meant as two separate posts) but presented here today as a long, rambling post in the eclectic posterboy style.... I am known for...see references for more study for yourself below.. PART 2 References Micronutrient deficiencies in inflammatory bowel disease trivial or crucial like IBS and Chrons one third have a thiamine deficiency https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4863043/ 1/3 develop a thiamine deficiency …..the other 1/3 develop Chronic Fatigue etc…or Beri Beri.. Thiamine and fatigue in inflammatory bowel diseases an open label pilot study albumin synthesis, increased albumin breakdown, a redistribution of albumin in body fluids and greater losses of albumin can all contribute to lower serum levels with the stress response. Forum/Blog reader: I had all these things …..but it was being diagnosed as part of my Celiac disease…. Chronic Fatigue (Magnesium and Thiamine) , Burning Feet, Depression etc….Low Albumin levels (for an unknown reason) etc…. and they all got better after taking Thiamine (undiagnosed Beri Beri)….at one point from complications in my diabetes…. I had creatine in my kidney’s now it is under control… To demonstrate that fatigue and other disorders related to ulcerative colitis and Crohn's disease are the manifestation of an intracellular mild thiamine deficiency and not due to malabsorbtion, augmented https://www.ncbi.nlm.nih.gov/pubmed/23379830 Gastrointestinal beriberi a forme fruste of Wernickes encephalopathy in India BMJ Case report? https://www.ncbi.nlm.nih.gov/pubmed/29982183 The difference between a thiamine deficiency and Beri Beri….reference work by Lonsdale A Review of the Biochemistry Metabolism and Clinical Benefits of Thiamine and Its Derivatives Lonsdale knitty kitty Reference work on the difference between a thiamine deficiency and Beri Beri…. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1375232/ Useful resources::::::::::) Things added on the 2nd day Lays out Stress Response in the body and how Interleukins help manage this in the body…. about Albumin Deficiency and Cytokine production….see paragraph on stress response in the body https://healthfully.com/albumin-deficiency-8042757.html Stress Response Hypoalbuminemia is often caused by an acute or chronic inflammatory response to stress. Infections, surgery, trauma or burns can lead to an increase in cytokine release and reduced albumin production. Decreased albumin synthesis, increased albumin breakdown, ****I apologize for the length of this post.....this even too long for me...I (usually as noted above might break this into 2 or 3 blog posts) but with what is happening right now in our society and the world with Corona virus...WE never know how long the outbreak might last or who it might effect....so in case I don't make back it to the forum (or another posterboy blog post) for awhile.... I unloaded the kitchen sink... in hopes it might help the next person who has similar symptom's and/is being misdiagnosed/or going undiagnosed like I was for so.....soooo.... many years! If this helps anybody in anyway....praise God! ....I know must will never finish this blog post....but I truly believe it can/will help those who do completely read it and follow up with their doctor's on it.... 2 Corinthians 1:3, 4 3 Blessed be God, even the Father of our Lord Jesus Christ, the Father of mercies, and the God of all comfort; 4 Who comforteth us in all our tribulation, that we may be able to comfort them which are in any trouble, by the comfort wherewith we ourselves are comforted of God.
- 1 comment
-
- celiac
- inflammation
-
(and 4 more)
Tagged with:
-
Celiac.com 09/05/2022 - According to studies, most people with celiac disease are exposed to gluten on a regular basis, even those who are trying to be diligent about avoiding gluten. For these people, eating gluten can trigger gastrointestinal symptoms and intestinal damage. Anyone whose ever had that happen can testify to the unpleasant results, including the stomach pain, bloating, diarrhea, and other symptoms. Currently, there aren't too many options for celiacs who are exposed to small amounts of gluten, especially for those exposed on a regular basis. A team of researchers recently set out to assess changes in the ratio of villus height to crypt depth in celiac patients exposed to 2g of gluten per day for 6 weeks, as part of a study on IMGX003 (Latiglutinase). On behalf of theCeliacShield Study Group, the research team included Joseph A. Murray; Jack A. Syage; Tsung-Teh Wu; Chaitan Khosla; and Jennifer A. Sealey-Voyksner. They are variously affiliated with the Mayo Clinic, Gastroenterology and Hepatology in Rochester, MN; the Department of Laboratory Medicine and Pathology, Mayo Clinic, Rochester, MN; ImmunogenX, Inc., Newport Beach, CA; the Boston Biostatistics Research Foundation, Framingham, MA; Faculty of Medicine and Health Technology, Tampere University and Tampere University Hospital, Tampere, Finland; and Stanford University, Stanford, CA. The team administered the double-blind, placebo-controlled gluten-challenge as part of a Phase 2 trial to assess the safety and efficacy of a 1,200 mg dose of IMGX003 in celiac patients exposed to 2 g of gluten per day for 6 weeks. The team used ANCOVA to assess progress toward their main endpoint, which was a change in the ratio of villus height to crypt depth (Vh:celiac disease), along with secondary endpoints, which included densities of intraepithelial lymphocytes (IEL) and symptom severity. Tertiary endpoints included serology and gluten-immunogenic peptides (GIP) in urine. Forty-three out of fifty randomized patients completed the challenge. Twenty one patients received IMGX003, while twenty-two received a placebo. The results showed that IMGX003 reduced gluten-induced intestinal mucosal damage and symptom severity in celiac patients on a six week gluten challenge of 2 grams per day. Drugs like IMGX003 could potentially play a role in receding symptoms and gut damage in people with celiac disease who are exposed to low amounts of gluten, especially through accidental exposure. Still, we've seen promising drugs come and go, each falling by the wayside when they failed to deliver in clinical trials. Stay tuned for more on this and related stories. Read more at gastrojournal.org
-
- challenge
- clinical trial
-
(and 7 more)
Tagged with:
-
Hi all, I am new to this forum and decided to post my current situation with two hopes: that others may have some acquired wisdom they can share, and to also help anyone else out there who may be struggling. I have had chronic vertigo, inability to concentrate (foggy headedness), inflammation in the glands and inner ear, and sore throat for 17 months now. The symptoms ebb and flow, with some days being more tolerable and the flare-ups making me bedridden. The symptoms began during the flu season and began with a flu-like illness that developed into the syndrome. I saw two general practitioners who were puzzled and sent me to an ENT. The ENT diagnosed the vertigo as the type that occurs when the crystals in the inner ear get shaken up and said he 'didn't care' about the chronic sore throat or swollen glands. He sent me to a physical therapist who disagreed with his diagnosis and said the vertigo was likely due to neuritis, or inflammation of the nerve in the inner ear, which is thought to be caused by a viral infection. This is much more likely, but doesn't explain why I cant shake it, and there is no accepted cure for neuritis. I have been gluten free for several years. (Prior to that, I was a vegetarian and ate massive amounts of wheat gluten daily and so developed Candidiasis (thrush), another saga that involved skeptical or hostile doctors and the necessity to do research and self-diagnosis.) In the last two weeks I've also developed joint pain in the right hand and my vision is sometimes blurry or 'off'. The evidence seems to point towards some kind of autoimmune disorder, such as lupus, rheumatoid arthritis or thyroiditis. I'm now looking into lectins in food and their apparent connection to immune suppression/disorders in some people, but the research is scant. I'm going to eliminate high-lectin foods (grains, legumes, dairy and nightshades) for a week to see if this impacts the symptoms. Has anyone ever experienced anything similar, or has any substantive information about the lectin connection? Thanks so much and so nice to see this forum! megan
-
Hi all! Newly diagnosed here and a quick Q! Does anyone else have an issue, pre-or-post diagnosis, with fatigue, headaches, dizziness, and general malaise after rigorous exercise? I came across an article somewhere, where it said that due to the inflammation, when you exercise it causes even MORE inflammation which causes a myriad of "unwell" symptoms. I love running, but find I have SUCH a long recovery rate after rigorous exercise. Let me know your experiences and your thoughts!!
-
Celiac.com 01/31/2022 - As intestinal permeability and innate immune system activation emerge as possible pathophysiological mechanisms in non-celiac gluten sensitivity (NCGS), a number of researchers have become interested in markers for gut integrity and inflammation. The idea being that thesis markers might help to reveal pathological changes that occur with non-celiac gluten sensitivity. A team of researchers recently set out to assess relevant biomarkers in non-celiac gluten sensitivity by analyzing serum levels of gut integrity and permeability markers, pro-inflammatory cytokines and antigliadin IgG in patients with suspected non-celiac gluten sensitivity on a gluten-free diet, and compare them to serum levels in patients with irritable bowel syndrome (IBS) and healthy controls (HC). The research team included Hanna Fjeldheim Dale, Julianne CH Johannessen, Ingeborg Brønstad, and Gülen Arslan Lied. They are variously affiliated with the Centre for Nutrition, Department of Clinical Medicine, University of Bergen, Bergen, Norway; the Division of Gastroenterology, Department of Medicine, Haukeland University Hospital, Bergen, Norway; and the National Centre of Functional Gastrointestinal Disorders, Haukeland University Hospital, Bergen, Norway. Their team analyzed serum samples collected from twenty patients with suspected non-celiac gluten sensitivity patients on a gluten-free diet, twenty with IBS, and twenty healthy sex and age matched control subjects. The team used IBS severity scoring system (IBS-SSS) to assess gastrointestinal symptom severity. Compared to heathy control subjects, suspected non-celiac gluten sensitivity and IBS patients had higher IBS-SSS scores. Their analysis showed no significant differences in serum levels of any of the gut integrity and permeability markers, cytokines or antigliadin IgG antibodies between the three groups. However, they did see positive correlations between claudin-1 and i-FABP, and between claudin-1 and antigliadin IgG antibodies. The team's assessment showed no differences in serum levels of gut integrity and permeability markers, pro-inflammatory cytokines or antigliadin IgG antibodies among patients with suspected non-celiac gluten sensitivity patients on a gluten-free diet, IBS and healthy control subjects. The findings suggest that these biomarkers do not offer a way to spot possible pathophysiological mechanisms in non-celiac gluten sensitivity. Stay tuned for more on this and related stories. Read more at DovePress.com.
- 2 comments
-
- celiac disease
- gluten
- (and 7 more)
-
Celiac.com 05/28/2021 - In my search for medical answers, the study of lectins did explain so much. (e.g. The “Lectin Report. Once we see that these harmful glycoproteins, especially those from gluten, dairy, soy and corn, can cause tissue damage/inflammation all by themselves, without an immune response, things really start making sense. The immune response is secondary to that damage, which helps to explain why we see such variation in the measurable response by different individuals. Some will respond with an outpouring of antibodies yielding positive tests while others will not, thus helping to explain the negative tests in individuals who end up responding quite well to the elimination diet when employ it despite those negative tests. These dietary glycoproteins are also a big part of what we love to call “autoimmune disease”. Personally, I do not like nor do I use that term anymore, unless I put it in quotes. That term implies that the immune system is attacking its own body’s tissues for no good reason. I contend that this does not happen...ever. The immune system always responds appropriately. We do not always fully understand why it does what it does. The inflammation being incited by lectins is a prime example of this. Lectins are antibody-sized proteins/glycoproteins. That, of course, makes them very tiny. How would we know they are there when they are that small? We can’t see them in a routine tissue sample. It would take biochemical analysis or, again, antibody testing to determine whether they are involved. Therein lies the rub. Once again, not everyone responds with what we might consider an “appropriate” response- one that we can detect readily. We just have to know that these lectins can and do cause changes in the individual cells of the body (from neurons to nephrons to blood cells, etc.) of susceptible individuals. I contend that the “big 4” (gluten, dairy, soy and corn) are not healthy for anyone. They are simply better tolerated by some than others. This is the nature of “spectrum disorders” which range in severity from the “best of the best” to the “worst of the worst” when it comes to the afflicted individual. I tell people to think “peanut allergy” when thinking about the worst of the worst. Whoa, now that’s a sensitivity! So, does gluten affect neurons? Definitely. Can it kill neurons? Yes! Run an Internet search for “gluten, neurons” and you’ll find some interesting things. How it damages and kills neurons is fascinating, and the clue is in the link above about lectins. A concurrent study of viruses helps to complete the big picture and that is why I write so much about this on my site now. It is logical that the viruses inside that cell are the things that determine the response of that cell to the challenge by lectins, carcinogens, and other chemicals/pollutants/preservatives, etc. Reading “The Lectin Report,” one might ask what really determines how a cell decides which of the ten different responses it will manifest once challenged by the lectin (ranging from cell death to tumor formation). I believe the answer lies in the adaptive viruses found inside that cell. That’s what viruses do in nature. They facilitate adaptation (as well as cause variation in nature). The cool thing is that our very DNA contains these adaptive viruses. Researchers now estimate that up to 45% of the genetic codes in our double stranded DNA are actually viral information. This is what retroviruses, in particular, do. They infect the cell and incorporate their genetic information into our DNA. That is why these particular viruses are involved in cancer and why cancer can be “genetic” (inherited). This information can be transmitted vertically to offspring. The other cool thing to understand is that cancer itself is an adaptive process. The viruses that “cause” cancer are simply adapting to the challenges (e.g. carcinogens) that we keep throwing at them. When all else fails, they cause the cell they are designed to protect to start growing out of control in order to ensure the survival of that virus and the cell itself. Thus, I now look at a tumor as a “protective cocoon”. Is this a radical idea? Yes. Does it make sense when you understand the good and vital work that viruses do? It certainly does to me. So why don’t we all have cancer and develop it early in our lives? Once again, because there is another part of the “syndrome” that is necessary- a weakened immune system. That’s right. We are all killing cancer cells right now (hopefully). The immune system recognizes when a cell is trying to do something inappropriate or harmful and sends in the cavalry. This could be just what we (incorrectly) label as an “autoimmune response”. The body does know exactly what it is doing each and every time it does something. I believe that down to my socks. Again, we just don’t understand what it is doing sometimes and I believe that this is one of those times. How does this apply to epilepsy and other neurodegenerative diseases such as MS, Alzheimer’s, Parkinson’s, and ALS? As stated above, some viruses love the central nervous system. The two most common brain tumors in veterinary medicine are the astrocytoma and oligodendroglioma, both of which are viral and of those cells that control many of the supportive functions of the neuron, including the production of the myelin sheath and the control of neurotransmitter levels (glutamate). If there are viruses in there causing tumors, then through “reverse engineering”, we can see that there are going to be the processes (e.g. “autoimmune diseases”) taking place that precede the formation of these tumors because these are the means by which the immune system controls the tumor production…until it is overwhelmed by all the toxins we are throwing at it.
-
Hi everyone, Is there documented link between celiac disease and gym/sport-related injuries? I'm a recently diagnosed celiac and I'm wondering if the reason I have so many injuries (which won't go away even after months of rehab) is the celiac disease. Basically, I have ongoing pain in a number of areas in my body (left shoulder, right hamstring, left Achilles). The specialist and physio I've seen both think it is tendinitis, but I've been doing the recommended rehab and stretches for it for about 10 months and it's not going away. The injuries started around August 2016. Around March 2017 (so, well after the injuries), I started getting really sick and I was diagnosed with celiac disease. I've been gluten free since April (4 months) and the 'sickness' symptoms are gone but my injuries are still here. It kind of feels like every time I do exercise, something new goes off in my body. And I'm not training like an idiot or anything - before this I was training for 10 years without any injuries. At this point I am kindof hoping to god it's because of the celiac disease and that the injuries will sort themselves out once I finish healing (which I understand takes over 6 months?). Otherwise I have no idea what to do because I've been to the sports-doctor and physio a trillion times, I've spent a million hours doing rehab and there's basically no improvement. I just wanted to know whether anyone else has experienced the same thing and if you have any advice
- 17 replies
-
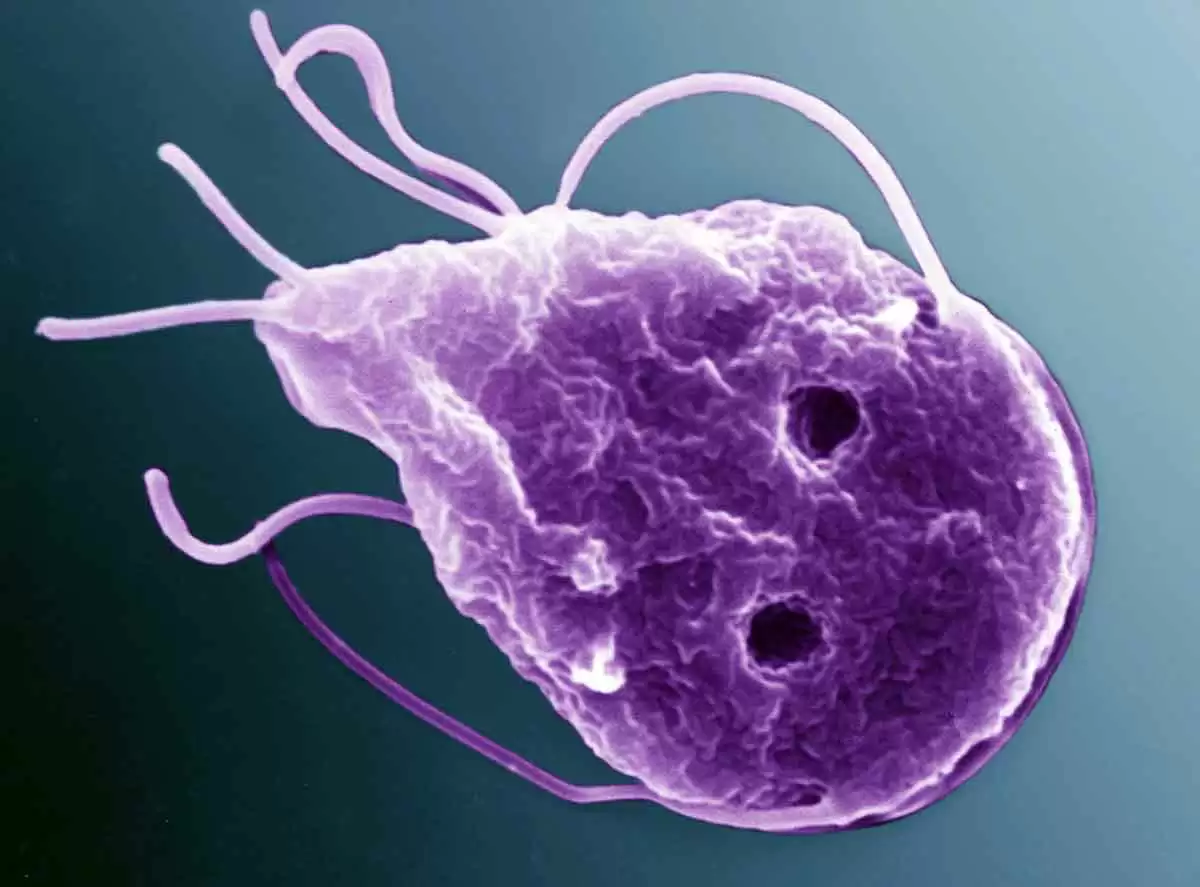
Celiac.com 05/12/2021 - Some types of intestinal inflammation or autoimmune disease can increase markers for celiac disease. A number of reports have suggested that intestinal infections may cause celiac disease to develop in certain people. A team of researchers recently set out to determine whether serum anti-tissue transglutaminase (tTG) and anti-endomysium antibodies (EMA) may be helpful in differentiating between giardiasis and celiac disease. The research team included Kurt Hanevik, Elisabeth Wik, Nina Langeland & Trygve Hausken. They are variously affiliated with the Centre for Cancer Biomarkers CCBIO, Department of Clinical Medicine, and the Department of Clinical Science at the University of Bergen, Bergen, Norway; and the Department of Pathology, the National Centre of Functional Gastrointestinal Disorders, Section of Gastroenterology, Department of Medicine, and the National Advisory Center for Tropical Infectious Diseases, Department of Medicine at Haukeland University in Bergen, Norway. The team looked at eight cases where patients showed elevated CeD serological markers and pathological duodenal histology during, or shortly after, Giardia infection. Their recent paper presents follow-up clinical and serological findings to determine which of these eight patients were diagnosed with celiac disease. Serum levels of tTG and EMA were poor indicators for spotting the difference between patients where celiac disease was excluded, and those who were later diagnosed with celiac disease. In their paper, the team discusses the value of these serological celiac markers in relation to celiac diagnosis in cases with chronic or recent giardiasis. Read their full report in the Scandinavian Journal of Gastroenterology [PAYWALL]
-
- celiac disease
- duodenal
-
(and 2 more)
Tagged with:
-
Celiac.com 04/30/2021 - According to Dangerous Grains by Dr. Ron Hoggan and James Braly, M.D., intolerances to foods other than gluten are the most common reason that people continue to have health problems after they've gone on a gluten-free diet. Yet, from the hundreds of emails I've gotten from people on the celiac email list, and from online forums, I've found that many people don't investigate other food intolerances, even though they suffer from health problems that likely could be cured by eliminating problem foods. I was sick for five months solid in the summer of 2004, after I'd adopted a gluten-free diet. I would get up in the morning feeling half well; I'd get my shopping done first thing in the morning. Then I'd go home and lapse into a semi-stuporous state. I would sit in a chair for the rest of the day, my mind slogging slowly through a swamp. I thought at the time it was hayfever from my 53 inhalant allergies, but I was taking six different allergy medicines, to no avail. I later found that I actually had intolerances to about 90% of the foods I'd been eating. What had really been happening, it seemed, was that I felt somewhat better after fasting overnight. Then I would eat something an allergen for breakfast. I'd get my shopping done then I'd start to feel sick from my breakfast. My inhalant allergies were actually only a small part of the problem. After going on an exotic foods diet, I became much healthier. In the summer of 2005, I went running every day and my mind was much clearer. My 53 inhaled allergies no longer bothered me as much. This is typical for people with multiple food intolerances. They can be hidden just like gluten intolerance. If you're like me, your body probably didn't like gluten long before you were aware of it. It's not like a peanut allergy. If you were allergic to peanuts, you'd probably know it. Your body isn't able to suppress that allergic reaction. But if you're gluten intolerant, you can eat gluten every day and never know what's making you so sick. Your body hides its reaction, so you don't notice feeling worse after eating gluten. Wheat might even have been one of your favorite foods. After you stop eating gluten, your body no longer has to work so hard to suppress food intolerance reactions. So if you have other food intolerances, after a few months or so you may start to feel obviously worse after eating those foods. This is an excellent reason for sticking strictly to a gluten-free diet - it will help you find any other food intolerances you may have, and thus speed your recovery. If you don't do a careful elimination diet, you may be in for a long, agonizing process of eliminating the foods you're intolerant to, one by one, feeling sick perhaps for years after starting a gluten-free diet. Food intolerance can cause many other problems. Joint pain and stiffness is a common symptom. Just before I found out about my gluten intolerance, both my elbows and knees were hurting, and the tendons in my forearm and hand hurt so much I couldn't lift a cast iron pan with one hand. After I eliminated the many foods I'm intolerant to, in addition to gluten, I was able to run without pain. I've also noticed that my old joint injuries often stiffen after food challenges. Joint inflammation and stiffening are thought to accelerate joint destruction in osteoarthritis, the wear-and-tear arthritis that many people suffer from as they get older. Many diseases are partly caused by chronic inflammation. Inflammation contributes to the onset and progression of tumors, and is involved in atherosclerosis. Hidden food intolerances can cause chronic inflammation and irritation in many areas of the body, so finding your food intolerances could help with any problem that involves irritation or inflammation. I think that when food intolerances are hidden, the body compensates somewhat for their pro-inflammatory effects, because my C-reactive protein and sedimentation rate, measures of inflammation, were high at a time when my food intolerances were in the process of being unmasked - but my C-reactive protein was actually lower than normal when I was still eating tiny amounts of some foods that I later found I had hidden intolerances to. However, the body doesn't seem to be able to compensate completely for the pro-inflammatory effects of food intolerances. A gluten-containing diet raises the risk of some GI tract cancers in celiacs. Perhaps other food intolerances also cause GI tract cancer - a scary possibility! I had a hard time with carbohydrates for more than twenty years. When I tried highly glycemic carbs, I would feel jittery, hungry, irritable, and tense. My carbohydrate reactions went away after I found my non-gluten food intolerances. I can eat almost any amount of tapioca starch mixed with maple syrup - an enjoyable, sticky goo with a very high glycemic index - and all that happens is that I get high and happy and I feel like going out and exercising. My jittery, anxious food reactions weren't simply reactions of intolerance. For example, I have intolerances to many low-carb foods, like peanuts. A tiny trace of peanut oil made me sick for days, but peanuts had never made me feel jittery or anxious when I ate them before I found my hidden food intolerances. Rather, it seems that having hidden food intolerances caused my body to release a lot of adrenaline after I ate carbohydrates, or else it made my body more sensitive to adrenaline. A study of people with suspected reactive hypoglycemia showed that they were hypersensitive to adrenaline. If you have emotional or psychiatric problems, it's also worth looking for hidden food intolerances, although according to Brostoff and Gamlin's book Food Allergies and Food Intolerance, people who have psychological problems from food intolerance usually have physical health problems as well. Some other problems that are possibly related to food intolerance are asthma, fatigue, rashes, irritable bowel syndrome, migraines, sinusitis, recurring urinary tract infections, and light and/or noise sensitivity. If you have food reactions that you might attribute to accidentally being exposed to gluten, but you can't verify that you actually had gluten, you might actually be reacting to other foods. The gold standard for finding food intolerances is to do an elimination diet for a week or two and then to try foods one by one, and see if they have some kind of bad effect. If you think you have a food reaction that's delayed for days, it would be a good idea to try the food again to see if the same reaction happens again. Here's another caution: once or twice, I've thought I'd reacted to a food challenge, when actually I had a bladder infection. If you do the elimination diet perfectly, you can probably find all of your food intolerances at once, which would save many people from many years of sickness. However, this is very difficult, because doing an elimination diet correctly means eliminating all common food allergens – that is, all foods that you normally eat fairly often, as well as all foods that might cross-react with those foods. Brostoff and Gamlin's book has a lot of information on food intolerance cross-reactions that very accurately reflects my experience. Ideally, you should also quit taking any medications or supplements that you normally take, or get your medications made by a compounding pharmacy without fillers, because most medications have many allergenic non-medical ingredients such as corn starch. Even your toothpaste could be causing a reaction. After I found my intolerance to birch, I kept on using toothpaste that was sweetened with birch xylitol, washing my mouth carefully with water after brushing my teeth. Once, though, I forgot to wash my mouth out, so a little toothpaste went down my throat, and I got sick for four days. You can brush your teeth with baking soda, which you won't have an intolerance to, since it's not made from anything organic. It's also very difficult to do an elimination diet because people are often addicted to foods they're intolerant to. On one elimination diet I did, I was unable to stop using fructose made from corn. Later, I painfully, slowly, quit using fructose over many months. When I finally eliminated all corn products from my diet, I found that my body had been masking about 30 or 50 other food intolerances, as a side effect of masking my corn intolerance. After I eliminated corn, I suddenly started getting sick after eating many of the foods I'd been eating all along. Elimination diets and food challenges can be done in an in-patient setting, which might be the only way to completely adhere to the diet. If you have an IgE mediated food allergy, food challenges should only be done with medical supervision. Brostoff and Gamlin's book has a number of elimination diets of varying degrees of strictness. Some people rely instead on IgG ELISA blood testing for food intolerances. The idea behind the test is that a higher than normal level of IgG antibodies to a food might mean that one has intolerance to it. The body normally makes IgG antibodies to foods. One research study showed that many people with irritable bowel syndrome were helped by eliminating foods based on IgG ELISA testing, but otherwise the tests haven't been validated by research. Researchers have also tried sending several blood samples obtained from the same person at the same time to different labs, or more than one blood sample to the same lab, and found the test results were very inconsistent. Finding your hidden food intolerances is often a long, painful process that is full of errors and guesses. It's also very important to do if you are not completely healthy on a gluten free diet.
-
- food intolerance
- food intolerances
- (and 5 more)
-
View full article
-
- food intolerance
- food intolerances
- (and 5 more)
-
Celiac.com 03/08/2021 - When people with celiac disease eat gluten, it triggers adaptive immune cells, which cause damage to the lining of the small intestine. Doctors gauge the severity of celiac disease through histological assessment of the intestinal damage via intestinal biopsy. To confirm diagnosis and to test drug efficacy in clinical trials, doctors rely on a gluten challenge. However, patients respond with different magnitudes to the same gluten challenge. This is a problem that a group of researchers looked at recently, in a study of 19 well‐treated celiac patients. The research team included Jorunn Stamnaes; Daniel Stray; Maria Stensland; Vikas K. Sarna; Tuula A. Nyman; Knut E. A. Lundin; and Ludvig M. Sollid. They are variously affiliated with the K.G. Jebsen Coeliac Disease Research Centre, University of Oslo, Oslo, Norway; the Department of Immunology, University of Oslo and Oslo University Hospital‐Rikshospitalet, Oslo, Norway; and the Department of Gastroenterology, Oslo University Hospital‐Ullevål, Oslo, Norway. In the study patients, proteome analysis of total tissue, or isolated epithelial cell compartment from formalin‐fixed paraffin embedded biopsies, collected before and after 14‐day gluten challenge, shows that patients with strong mucosal response to gluten challenge have signs of ongoing tissue inflammation prior to the gluten challenge. This low‐level tissue inflammation at baseline is mirrored by increased gluten specific CD4+ T‐cells in the gut, and a low‐level blood inflammatory profile. This study shows that even well‐treated celiac disease commonly features ongoing low‐grade inflammation and anti-gluten immunity in the gut mucosa, and that histology assessment alone is not a good measure of full recovery and gut mucosal healing in celiac patients. The findings raise a concern that even a vigilant gluten‐free diet might not be enough to curb gut inflammation in all celiac disease patients. Read more at Wiley Online Library
- 52 comments
-
- celiac disease
- chronic
-
(and 5 more)
Tagged with:
-

Gluten's Inflammatory Role in Celiac and Other Chronic Diseases
Scott Adams posted an article in Winter 2008 Issue
Celiac.com 02/05/2021 - Recently, a team of doctors in the Czech Republic conducted a study of the inflammatory action of wheat gluten, and its relation to chronic diseases. Even with all of the research that has been conducted, many of the causes and mechanisms behind inflammatory and autoimmune diseases remain shrouded in mystery. Doctors just don't know what causes most autoimmune diseases or how they actually work. It is assumed that some sort of a breakdown occurs in the innate and adaptive immune system that regulates the body's mucous. On one level this makes a great deal of sense. Epithelial cells make up our skin and the linings of our respiratory, digestive and uro-genital tracts. From the moment we're born, our epithelial cells are coming into contact with the substances from the outside world. Our skin is regularly bombarded by germs, bacteria, and other foreign substances. Just the simple act of breathing brings dirt, germs, bacteria and other foreign substances into contact with the epithelial cells that line our lungs. Eating and drinking brings dirt, germs and bacteria into contact with the epithelial cells that line the digestive and uro-genital tracts. It is the job of our mucous layers, and the mucous they generate, to protect our epithelial cells that line our respiratory, digestive and uro-genital tracts. When the mucous layer fails, the immune system can be stressed. When the immune system breaks down or over-reacts, autoimmune ailments can result. Unlike the multiple layers of epithelial cells that form the protective layers of our skin, just a single layer of epithelial cells protects our uro-genital, respiratory and digestive tracts. Many people are surprised to learn that the surface area of human skin averages just two square meters in size, while of the lining of the respiratory, digestive and uro-genital tracts average about 300 square meters. Again, these surfaces are mostly covered with just a single layer of epithelial cells, yet to fend off the millions of micro-organisms that regularly bombard them they must be able to tell the bad from the good microorganisms and to keep the bad ones from crossing the epithelial barrier. Unlike other food proteins, the group of proteins in wheat, known as gliadin, has the ability to cause immune cells to produce cytokines. Cytokines are proteins and peptides that function as signaling compounds. Simply put, they tell other cells what to do. Inflammatory Activity of Gluten in Chronic Disease In the case of celiac disease, the presence of wheat protein activates immune cells to produce cytokines that tell the cells lining the intestine to become inflamed as a means of protecting the body against what it sees as a foreign invader. In the skin, mucosa, and lymphoid tissues there is a highly specialized kind of white blood cell called a dendritic cell. The role of dendritic cells is to initiate a primary immune response by activating lymphocytes and secreting cytokines. Research has shown that when these dendritic cells are exposed to wheat gliadin, they cause the body to increase the production of cytokines, which in turn triggers inflammation of the mucosal layer. This pattern of activity seems to play an important part in celiac disease. As stated earlier, this thin epithelial layer is all that protects the body from invasion by harmful intruders. It is also a place where nutrient exchange occurs. In the respiratory tract, oxygen is exchanged. In the digestive tract, nutrients are absorbed. In fact, for nutrients to be absorbed, it is necessary for there to be a degree of permeability in these cell linings. If they kept everything out, we'd die of malnutrition, or maybe thirst. If they let everything in, we'd likely die of one disease or another. So, the body keeps up a delicate balancing act here. In fact, the body has developed a highly sophisticated system of mechanical and chemical mechanisms whose job it is to protect this single layer of epithelial cells by identifying, degrading and removing intruders, while identifying and permitting beneficial items like nutrients to pass freely into the body for processing. In healthy folks, this process works very smoothly. The bad stuff is broken down and cleaned out, while the good stuff is permitted to cross the barrier and to carry the proper nutrients to our bodies. Once we leave the sterile environment of the womb, billions of different bacteria begin to colonize most of our mucosal and skin surfaces. Whether a person is healthy or not, the number of foreign bacterial cells living on and in our bodies far outnumber the cells we have when we are born. Most of these bacteria are beneficial, with the most beneficial bacteria residing in the gut. In fact, there are so many different kinds, with such high levels of specificity, that scientists haven't yet been able to cultivate all of them. These beneficial bacteria in the gut play an important role in immunity, metabolism, and other activities. Gluten's Connection to Various Chronic Diseases A wide range of inflammatory and autoimmune diseases are associated with celiac disease and untreated celiac patients, including a higher risk of complications from anemia, infertility, osteoporosis, and gastrointestinal cancer. Many other disorders are associated with celiac disease, including endocrine diseases like type 1 diabetes, thyroiditis, connective tissue diseases, liver diseases, and Down syndrome, along with nervous system disorders like epilepsy, ataxia, and peripheral neuropathy. One of the strongest associations with celiac disease is autoimmune diabetes. We now know that 5-10% of diabetic patients have celiac disease, a rate more than 5 to 10 times that of the general population. Almost all of these patients improve on a gluten-free diet. It's unclear why a gluten-free diet might produce improvement in some of these people with these conditions, but one prominent hypothesis is that a percentage of folks with those conditions have compromised gut barriers that somehow permit undigested gluten that provokes an immune response. An interesting side-note here is that mainstream researchers have recently begun to admit that diabetes, which was previously thought to be "exclusively" endocrine in nature, and heart disease, which was thought to be "purely" circulatory in nature, are both characterized by an inflammation component. In other words, inflammation of tissue, and therefore, of cells, plays an important part in both diseases. Similarly, celiac disease, which was thought to be largely gastrointestinal in nature, is increasingly showing connections to a wide range of disorders that affect nearly every major organ in the body. Strangely, or perhaps not so strangely in light of this recent evidence, a gluten-free diet seems to have a beneficial effect on a number of chronic diseases in people who are entirely free of celiac disease. Some patients with psoriasis and urticaria, for example, have shown improvement with a gluten-free diet, as have some patients with cryptogenic ataxia and peripheral neuropathy. A number of schizophrenics have shown a reduction of symptoms on a gluten-free diet. Also, a number of people with rheumatoid arthritis who observe a vegan, gluten-free diet have reported improvement in their condition. Animal models have proven to be helpful in better understanding many different diseases and to help create new and more effective treatments. There's a whole specialized area of biology called "Gnotobiology." These people specialize in working in germ-free conditions. Gnotobiologists have developed strains of animals that are reared in germ-free environments. Imagine if you had never been exposed to any of the harmful or beneficial bacteria that colonize the human body once it leaves the sterile environment of the womb. You would make a great guinea pig for better understanding how disease might work. Like people, once rats are born, they undergo a profound change. Intestinal microflora have a major effect on their mucosal immune system. One of the benefits of using gnotobiotic animal models is that researchers can separate the effects of microflora and dietary antigens. Since scientists know that applying wheat-gliadin to the gastro-intestinal tracts of conventionally raised rats of the AVN strain beginning shortly after birth results in pronounced jejunal changes, that is, celiac-associated lesions, it's beneficial if they can have a "clean" group of rats to test and compare against the conventionally raised rat group to see if there's some kinds of microflora that might provide some protection against celiac disease. One of the things that the research team discovered is that breastfeeding seemed to be profoundly protective against the adverse effects of wheat gluten. The research team actually looked at rat pups in which they had induced enteropathy to compare those given breast milk to those handfed on formula. Among other things, they found that rats that were suckled never showed flat mucosa so characteristic of celiac damage when exposed to wheat-gliadin. Its unclear exactly why this is, though breast milk has so many beneficial elements to it, that it's hard to imagine it not being responsible for a great deal of immune-related development in general. Rat breast milk in particular imparts epidermal growth factor (EGF), which seems to play an important part in of the rat's jejunal cells. The research team also studied the effects of gliadin in a model system. In fact, the team was able to take a close look at the effects of gluten on cells within the stomach cavities of mice. In one test, a group of rats received epidermal growth factor via breast milk, while another group received straight formula with no EGF. Both were treated with wheat-gliadin. Rats without EGF showed villous atrophy, while those receiving breast milk, and thus, EGF, were protected against pathological mucosal changes and also against celiac-associated damage. Basically, it all boils down to several things: First, it looks very much like the way is paved for the development of celiac disease by the innate immune system when the presence of gliadin promotes functional and phenotypic maturing in dendritic white blood cells, which then leads to the gliadin peptides being presented to certain T lymphocytes, which then trigger the associated inflammation and resulting damage. The research team concluded that it does, indeed, seem to be the unique structure of gluten and its fragments that provokes the response from the mechanisms of innate immunity. In predisposed individuals, gluten seems to more readily activate an immune response than other proteins like soy protein and egg protein. Breastfeeding seems to offer some protection against gluten intolerance and associated damage. In many cases, a gluten-free diet brings about improvement in chronic inflammatory and autoimmune diseases. Celiac disease is just one of many inflammatory and autoimmune diseases to be associated with the intestinal damage arising from chronic exposure to gluten in gluten-intolerant individuals. Also, many inflammatory and autoimmune diseases show improvement once gluten is excluded from the diet. Reference: Published In "Inflammation and Infection. The Golden Triangle: Food—Microflora—Host Defense". P.J. Heidt, Z. Midtvedt., V. Rusch, D. van der Waaij (Eds.) Old Herborn University Seminar Monography, 2007-
- celiac
- celiac disease
-
(and 5 more)
Tagged with:
-
Inflammation: Is it a Good Thing or a Bad Thing?
Melissa McLean Jory posted an article in Autumn 2008 Issue
Celiac.com 09/12/2020 - In order to understand how inflammation impacts those of us with celiac disease, we must first understand what role it plays in the body’s defense system. In many cases, inflammation is a good thing. It’s a non-specific, protective response by the immune system against infectious agents, toxic irritants, abrasions, tissue injury, and even extreme temperatures. It’s our natural and desirable attempt to protect, repair, and maintain healthy tissue — both inside and outside the body. I’m sure you’ve experienced a nasty burn or cut on your finger and have watched the body’s response to the injury. Within seconds various internal “first responders” are called upon and the characteristic signs of inflammation quickly appear — redness, pain, heat, and swelling. Depending on the severity of the injury and where it occurs, inflammation can also cause a loss of function. Because inflammation is a general and non-specific protective mechanism, the response is similar whether the damage is caused by invading cooties or a misdirected hammer. These symptoms are part of the healing process and under normal conditions are indications that the immune system is doing its job. When is inflammation a bad thing? When the response is misdirected, never shuts off, targets healthy tissue, or results in chronic and ongoing inflammation. Rather than playing a protective role, an overly active immune response can result in tissue injury and disease. Celiac is a genetically predisposed autoimmune disease triggered by the ingestion of gluten and is an example of how immune-mediated inflammation can cause damage, in this case to the small intestine. Left untreated, it can cause nutrient malabsorption, systemic inflammation, and a cascade of associated autoimmune conditions. We don’t want that. So, what can be done to put the fire out and enhance overall health? Make anti-inflammatory foods part of a sound nutrition plan and whether you have celiac disease or not, you and your family will benefit. Here are 10 anti-inflammatory tips to get you started: Eliminate or minimize processed and “junk” foods and avoid products that contain trans-fats, partially hydrogenated fats, or high-fructose corn syrup. Choose healthy fats such as extra-virgin olive oil, avocados, walnuts, pecans, almond butter, and flax seeds. Skip the soda pop. Have water or green tea instead. If you choose to drink alcohol, an occasional glass of red wine has been shown to be beneficial to overall health. Choose a wide variety of fresh, colorful fruits and vegetables—organic if possible and strive for 9 servings per day, 5 servings of vegetables and 3 to 4 servings of fruit. Eat healthy non-gluten grains like teff, quinoa, amaranth, and brown rice. Add legumes (beans, peas, lentils) to your diet, as they are a rich source of high-quality plant protein. Choose nuts, seeds, raisins, and dates for snacks or an occasional small serving of dark chocolate when you need a “sweet fix.” Season foods with health-enhancing herbs and spices like garlic, capsicum (chili), turmeric, cinnamon, ginger, and cilantro. Eat cold-water fish such as wild salmon, sardines, herring, mackerel, or anchovies. These choices are high in omega-3 fatty acids, which help reduce inflammation. Grass-fed bison, lean meats, skinless chicken, and eggs are good protein choices. Think positive, reduce stress, get adequate sleep, and exercise regularly. I know, easier said than done, but well worth it in the long run!-
- anti-inflammatory
- celiac disease
-
(and 3 more)
Tagged with:
-
Celiac.com 06/19/2018 - Could baking soda help reduce the inflammation and damage caused by autoimmune diseases like rheumatoid arthritis, and celiac disease? Scientists at the Medical College of Georgia at Augusta University say that a daily dose of baking soda may in fact help reduce inflammation and damage caused by autoimmune diseases like rheumatoid arthritis, and celiac disease. Those scientists recently gathered some of the first evidence to show that cheap, over-the-counter antacids can prompt the spleen to promote an anti-inflammatory environment that could be helpful in combating inflammatory disease. A type of cell called mesothelial cells line our body cavities, like the digestive tract. They have little fingers, called microvilli, that sense the environment, and warn the organs they cover that there is an invader and an immune response is needed. The team’s data shows that when rats or healthy people drink a solution of baking soda, the stomach makes more acid, which causes mesothelial cells on the outside of the spleen to tell the spleen to go easy on the immune response. "It's most likely a hamburger not a bacterial infection," is basically the message, says Dr. Paul O'Connor, renal physiologist in the MCG Department of Physiology at Augusta University and the study's corresponding author. That message, which is transmitted with help from a chemical messenger called acetylcholine, seems to encourage the gut to shift against inflammation, say the scientists. In patients who drank water with baking soda for two weeks, immune cells called macrophages, shifted from primarily those that promote inflammation, called M1, to those that reduce it, called M2. "The shift from inflammatory to an anti-inflammatory profile is happening everywhere," O'Connor says. "We saw it in the kidneys, we saw it in the spleen, now we see it in the peripheral blood." O'Connor hopes drinking baking soda can one day produce similar results for people with autoimmune disease. "You are not really turning anything off or on, you are just pushing it toward one side by giving an anti-inflammatory stimulus," he says, in this case, away from harmful inflammation. "It's potentially a really safe way to treat inflammatory disease." The research was funded by the National Institutes of Health. Read more at: Sciencedaily.com
- 3 comments
-
- anti-inflammatory
- auto-immune
- (and 5 more)
-
Celiac.com 12/02/2019 - Parkinson’s development can take many paths, with factors like genetics, aging, and environmental conditions all playing roles. Most people with Parkinson’s disease experience non-motor-symptoms, such as chronic constipation and/or impairment of gastrointestinal (GI) transit, long before the disease manifests clearly. Researcher Tomasza Brudek recently reviewed available medical literature for a possible link between Inflammatory Bowel Disease (IBD) and Parkinson's Disease. Brudek is affiliated with both the Research Laboratory for Stereology and Neuroscience, Copenhagen University Hospital, Bispebjerg-Frederiksberg Hospital in Copenhagen, Denmark; and the Copenhagen Center for Translational Research, Copenhagen University Hospital, Bispebjerg and Frederiksberg Hospital in Copenhagen, Denmark. Build-up of α-synuclein protein in the form of Lewy bodies and Lewy neurites, and degeneration of substantia nigra dopamine neurons are classic clinical markers of Parkinson's Disease. Major features of Parkinson's Disease include inflammatory responses manifested by glial reactions, T cell infiltration, and increased expression of inflammatory cytokines, along with other toxic mediators derived from activated glial cells. Experimental, clinical and epidemiological data suggest that intestinal inflammation influences the development of Parkinson's Disease, while more and more studies suggest that Parkinson's disease may begin in the gut long before any motor symptoms show up. Patients with inflammatory bowel disease (IBD) have a higher risk of developing Parkinson's Disease compared with non-IBD individuals. Gene association study has found a genetic link between IBD and Parkinson's Disease, and an evidence from animal studies suggests that gut inflammation, similar to that observed in IBD, may induce loss of dopaminergic neurons. Based on preclinical models of Parkinson's Disease, some clinicians hypothesize that the early stages of early in Parkinson's Disease are marked by enteric microbiome changes, and gut infections triggering α-synuclein release and aggregation. Because gastrointestinal pathology can play such an important role in Parkinson's Disease development, there's good reason to believe that IBD and IBD treatments can influence Parkinson's Disease risk. This review underscores how important it is for physicians to be aware of Parkinson's Disease symptoms in IBD patients. Read more in the Journal of Parkinson's Disease, vol. 9, no. s2, pp. S331-S344, 2019
- 6 comments
-
- crohn’s disease
- inflammation
- (and 3 more)
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8-M):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8):
Celiac.com Sponsor (A8-M):