Celiac.com 11/29/2019 - In previous issues of The Journal of Gluten Sensitivity, I told the story of how life-long celiac disease had caused me to experience a severe health-crisis rooted in hypothyroidism, and how hard I found it to get a correct diagnosis and treatment. This piece picks up the story at its very end, where I found a serendipitous outcome as a result of doing my own research and taking charge of my own treatment.
In fall 2008, my single-minded concentration on my thyroid issues had to take a back seat to another problem I could no longer ignore. Since 1984, I had been having problems with back pains that were sometimes nagging and sometimes intense. The reason for this wasn’t clear; I had never had a severe auto accident or any fall more severe than falling off a bicycle. I had managed to treat this problem with visits to a chiropractor. After a severe pain attack in 2008, I finally decided it was time to thoroughly investigate what the problem was.
Celiac.com Sponsor (A12):
X-rays from multiple angles, and an MRI, showed a pretty messy situation. I had a herniation at L3-L4, and degeneration at L4-L5 and L5-S1. A visit with an M.D. orthopedist specializing in spinal issues quickly made it obvious that conventional medicine didn’t have much to offer, and the probability of a successful outcome from expensive, life-disruptive surgery was low.
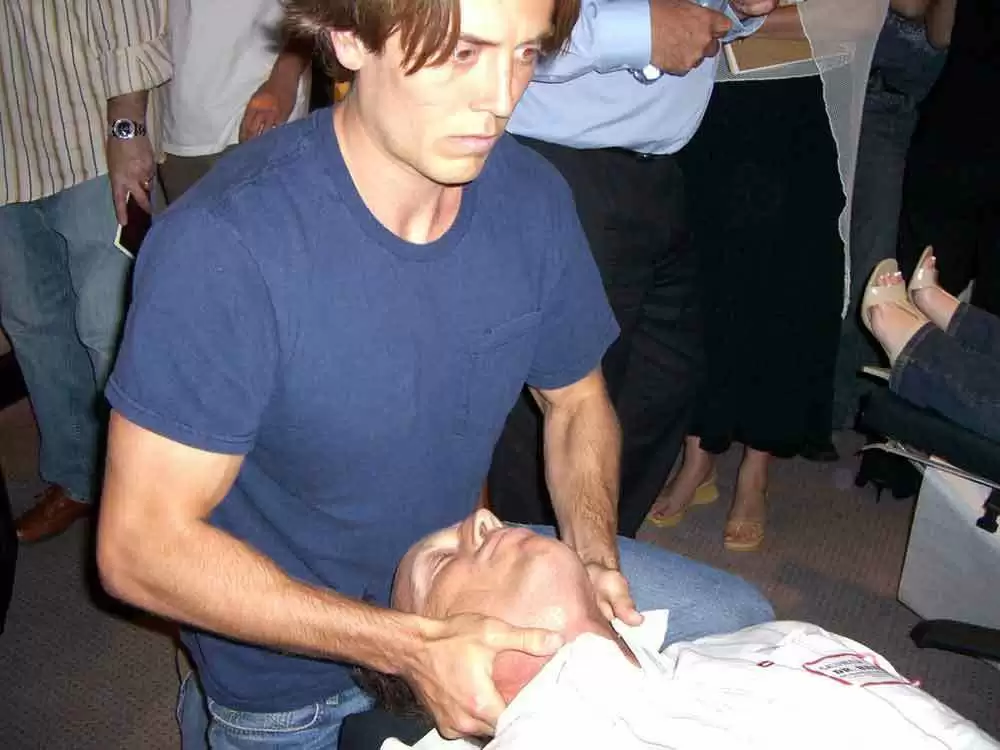
I finally elected to do spinal decompression therapy with a reputable chiropractor who has a long record of ethical treatment. Three months of therapy were sufficient to produce improvement, but I still did not feel “cured”. A fall or jolt could cause pain and instability to return.
As I lay on the decompression table thinking about what could have caused this problem, the truth was soon obvious. I had already read that celiac patients often have problems related to bone and connective tissue degeneration. It seems obvious now that hypometabolism due to thyroid failure stretching over more than 17 years, multiple endocrine deficiencies, and many years of severe nutritional deficiencies stemming from gluten enteropathy, are the culprits to blame for this problem. Being under constant pressure, it is difficult for the body to repair the lower back; under the conditions caused by gluten poisoning, repair becomes impossible.
As 2008 was coming to an end, a net-friend casually asked me if I had considered Wilson’s Temperature Syndrome (or “Reverse T3 Dominance” as it is called outside the USA). I visited the Wilson’s website, ordered the books, and studied the theory carefully. I already knew I had hypometabolism because my body temperature tended to stay rather low, usually just over 97F, and sometimes even as low as 96.3F basal (upon awakening). But, a generation of doctors who had learned to make fun of the late Broda Barnes M.D. and his temperature theory, were in the habit of not noticing sub-normal temperature in their patients; or if they did, stating that it didn’t matter. So, it seemed like the Wilson protocol, with low temperature a primary diagnostic prerequisite, might be worth a try. After all, I had tried (what seems like) almost everything else.
In January 2009, I went off T4 completely and began taking a combination of immediate-release and sustained-release T3 (triiodothyronine), along with a daily B-12 lozenge to blunt the “rush” from immediate-release T3. T3 is the thyroid hormone which the body actually requires. The fact that T4 is used successfully with many hypothyroid patients means that they have sufficient quantities of ferritin, cortisol, the deiodinase thyroid conversion enzymes, etc. Patients who don’t have the correct biochemistry, suffer because their bodies convert too much T4 into Reverse T3 in a mis-guided, maladaptive attempt to get rid of excess T4.
The result of T3-only therapy on brain function was astounding! Once I had been off T4 10 days, and on T3 doses of 20-25mcg per day for a week, the brain fog and motivation problems I had had for nearly 20 years, simply went away. The conclusion was obvious: in addition to the glandular hypothyroidism I had acquired from the effects of gluten, I had “Reverse T3 Dominance”, a (usually) stress-caused disorder in which the body converts too much of its T4 to rT3. rT3 is a compound which is the chemical mirror-image (reverse) of T3, but has no biological activity, other than to block thyroid receptors from receiving T3. The protocol described by Wilson is difficult; I went though one cycle of loading the body with sustained-release T3 and found it eventually produced hyperthyroid symptoms. It soon became obvious that, in addition to being difficult, there was much about the Wilson Protocol that was simply illogical.
Within a couple months after starting T3 therapy using the Wilson protocol, I learned it was possible to use only non-time-release T3 (Cytomel) with equally good results. The leading proponent of this approach is John Lowe, D.C.. I worked my total Cytomel dose up as high as 190 micrograms/day while I was still in the process of clearing rT3. Once rT3 was mostly cleared, I quickly went hyper and began dropping my dose, finally ending up at my current dose of 60 micrograms/day. This dose produces the desired blood FT3 level of 5-8 picograms/ml. On this program, I not only feel energetic during the day and sleep well at night, but my weight dropped to where it should be (165 lbs.).
As my treatment progressed during the year 2009, I would discover a totally serendipitous and welcome side-effect of T3 therapy. By June 2009, I became conscious that my back no longer felt as painful and instable as it had. This was proved in Sep 2009, when I was slammed to the ground in a freak mountain-biking accident. My back did not go into spasm, and recovered fairly quickly. By Nov. 2009, I was no longer having any back pain or instability.
I still had lingering effects from celiac-caused degeneration, which became obvious in Aug. 2009 when I had an osteoporosis evaluation requested by my regular doctor. He had become suspicious about whether the back problems were related to osteoporosis. The finding of bone density at 0.75 grams/square-centimeter in the neck of my right femur was clearly osteopenic and very close to osteoporosis. This was not a surprising finding; I was expecting a problem. A saliva test of adrenal function, also conducted in August, showed that my adrenals were still awakening in the middle of the night. This is a common effect of previous long-term hypothyroidism, which can be expected to gradually get better, and it has: sleep quality was continuing to improve through the end of 2009.
In Nov. 2009, the chiropractor who had been administering my decompression treatments was amazed at my progress. He had thought I was “fragile” when I started treatment with him in Oct 2008, but was now amazed at the increase in leg muscle strength when he tested me on his table. He was definitely interested in what T3 had done to me ... and probably a bit disappointed that I no longer need decompression treatments!


.webp.79a67df98ffcda77611af217c2a79682.webp)


Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now