
Celiac.com 09/14/2018 - If it is really true that nobody really wants to see a grown man cry, then certainly nobody would have wanted to hang around me near the onset of a long illness whose mystery would take 14 years to solve.
It began subtly and mildly in 1989, my 43rd year. I had just finished a long and exhausting malpractice suit on behalf of my daughter, an attractive, genetically-normal child who had contracted quadriplegic cerebral palsy in a completely avoidable incident of post-natal asphyxia which had radically changed the nature of life for my spouse and I. By the time 1989 rolled around, I was thoroughly exhausted and carrying a toxic load of anger directed at an incompetent member of the medical profession who had never learned the importance of state-of-the-art skills in a profession that literally has the power of life, death, and disability.
Celiac.com Sponsor (A12):
From late 1989 on through 1990, I experienced strange episodes of profound sadness, usually of one to two hours duration, that became increasingly disruptive to my ability to handle a job and child-care duties. Initially, these episodes seemed to come from nowhere. Later on, I found that playing certain pieces of music of which I was fond, would send me into such intense sobbing that I would be forced to pull over if this occurred while driving.
By the time 1991 rolled around, something was to be added to these periodic bouts of intense sadness. Early in that year, my daughter became very ill, keeping both my spouse and I awake at night for weeks on end. By the time the problem was diagnosed to be a dental infection and dental surgery was done, I had begun to have a sensation of “hollowness”, as though I really weren’t part of this world, most of the time. In late summer of that year, a series of events in which my subconscious had informed me that a friend had a serious illness, sent me into a final “dive”: I simply stopped sleeping more than about two hours per night. When I first stopped sleeping, I soon noticed that even low-level use of alcoholic beverages would further interrupt sleep and throw me into a state in which I couldn’t think of anything but how terrible I felt. This state of pronounced alcohol intolerance would continue for 14 years.
The final blow came in November 1991, when I went into a completely disabling panic/anxiety attack that sent me to bed, cowering. I had no alternative but to seek treatment from the psychiatric profession. Unfortunately, the first two psychiatrists prescribed drugs which either had no effects, or had effects that seemed worse than the problem they were supposed to solve. The third psychiatrist, whom I stuck with for about six months, came up with a treatment plan that was partially effective (but certainly not restorative). I stayed with this psychiatrist until it became clear that his treatment was equivalent to Jefferson Airplane singing “one pill makes you larger, and one pill makes you small”. I was being jacked up every morning by a toxic, activating SSRI anti-depressant so I could semi-function, and then dropped by benzodiazepenes every night into a non-restorative twilight sleep state.
In retrospect, the most amazing thing about these first three psychiatrists was that not one of them ordered any tests of my endocrine function. Treatment consisted solely of a series of benzodiazepenes, anti-depressants, mood stabilizers, and anti-psychotics, administered in a trial-and-error fashion that yanked my psyche and body chemistry around like a manic pit bull on a two-foot leash.
Throughout the latter part of 1992, I transitioned to care with my primary-care physician, mostly because I trusted him more than any of the psychiatrists I had seen up to that time. He was able to stabilize me with one of the old tri-cyclic anti-depressants, doxepin, along with low doses of valium. Although doxepin packs a big morning hangover for many who use it, and has very strong anti-cholinergic effects, its ability to put me out at night helped me function satisfactorily for much of the 1990s, even at doses as low as 10mg, once daily in the evening.
In 1993 I consulted a highly-recommended psychiatrist, who was the first psychiatrist who actually looked at my thyroid function. When my TSH was measured at 3.5, without also checking my FT3 and FT4, that doctor concluded that thyroid was not my problem. Of course, standards of thyroid diagnosis and treatment have changed radically in the 12 years since. Under the new AACE guidelines, a TSH of 3.5 would now be suspect, because studies of patients with TSH over 3.0 have shown that most progress to hypothyroidism (i.e., TSH greater than 5.5). The new AACE guidelines would mean that further testing and evaluation should be done.
Until the fall of 1997, I continued treatment with doxepin and intermittent valium, adding the practice of meditation to help calm myself. At that time, I came back to my primary-care physician with the symptom of profound exhaustion on top of the symptoms of insomnia, anxiety, and depression I had suffered for years. Fortunately, my GP was suspicious of thyroid function, and found that my TSH was floating above 8. Since this was well above the old/traditional limit of 5.5, he was ready to start treatment, with (as would be expected of most GPs) T4-only replacement.
I began taking thyroxine (T4) shortly thereafter with high hopes. Initially, the treatment was successful: getting the added thyroxine into my system caused an immediate improvement in quality of sleep.
However, the use of T4 did not turn out to be an unqualified success. After use of T4 for about a month, it was apparent that use of thyroxine alone did not produce a full recovery—I still suffered from anxiety, which the medication seemed to be increasing.
In the meantime, hair loss became an issue. Several years earlier, I had noticed that running my fingers through my hair would produce an unpleasant sensation, almost as though the hair roots were tender. By the time of my 50th birthday, in 1996, I had noticed that my pillow was virtually coated with hair by the time I would remove it for washing. Unfortunately, nobody, including my GP, reminded me that hair loss is a prime symptom of hypothyroidism; and, like most males, I was ready to assume it was plain old male pattern baldness. By the time I was treated correctly and the hair loss stopped, I had pronounced thinning on the crown which was too advanced to be reversed in response to the treatment of the thyroid problem.
In about 1998, I began experimentation with amino acids which was to last for almost seven years. I found that use of tryptopan, 5-HTP, and GABA could reduce (but not correct) the worst of my symptoms. In retrospect, though, use of amino acids is a poor substitute for a well-functioning thyroid, as well as being expensive and inconvenient.
By the summer of 1999, I had reached a paradoxical situation. Experimentation had shown that my body needed on the order of 100 micrograms of thyroxine (T4) to keep my TSH down to a reasonable level; yet taking that much T4 was causing intense anxiety, requiring me to use strong sleeping medications. By late summer 1999, I had noticed another distressing symptom—my acute sense of hearing was being increasingly impacted by tinnitus. Evidently, the root cause that drove me into hypothyroidism, could also impact hearing.
It was soon after a household move in the spring of 2000, that I had a partially-disabling attack of severe epicondylitis (more commonly known as tennis elbow). It was obvious that my body was no longer able to handle the short-term stresses of the hard physical work required by a move. This obvious physical symptom, accompanied by increasing periodontal issues and continuing mental issues, prompted me to seek other treatment.
In September 2000, I began seeing a prominent “metabolic” doctor (M.D.) who is well known for his treatment of the metabolic disorders of diabetics. This doctor has written a number of books related to dietary changes and supplements needed to stave off metabolic degeneration as one ages. I was switched to Armour thyroid, and began treatment with other hormones (primarily hydrocortisone in low doses to supplement adrenal function, and pregnenolone). I took an enormous range of nutritional supplements recommended by this doctor, and also made radical changes in diet, which I maintained for nearly two years. Unfortunately, nothing seemed to really work—I did not obtain substantial relief of my symptoms. A thyroid test in Sep 2001 still showed unsatisfactory results—my TSH was 4.7, and my FT3 was below the bottom of the normal range.
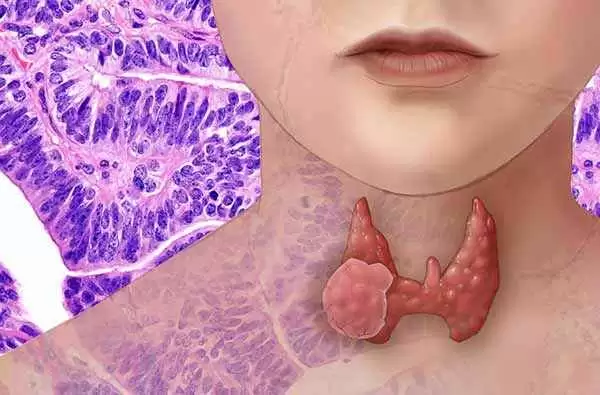
By the spring of 2002, I had decided I would have to take my care elsewhere if there were to be progress. After doing a brief telephone consult with a naturopath outside my home state, I began seeing a naturopath in my home town for whom I had obtained very positive recommendations via a web search. By March 2002, the naturopath had informed me that testing showed my hypothyroidism was due to anti-thyroid antibodies, i.e., my body was attacking its own thyroid gland. This condition is officially known as Hashimoto’s Autoimmune Thyroiditis (HAIT—as I now know, HAIT is the leading cause of hypothyroidism). I found this discovery quite amazing; how come the three endocrinologists I had seen between 1998 and 2002, had not given me this information? I was started on Thyrolar (synthetic combination T3/T4) by the naturopath, because she said that my body’s ability to make T3 may have been compromised by HAIT.
Soon after beginning to see the naturopath, I learned that Dr. Stephen Langer of Berkeley, CA might have additional information on the problem I had been having with thyroid hormone causing anxiety in a hypothyroid patient. I had searched for information about this syndrome in a number of places but found nothing; for instance, the well-known book “Thyroid Solution”, by Ridha Arem M.D., contains no information on the condition. So, I consulted with Dr. Langer and learned that a small percentage of people with Hashimoto’s are exquisitely sensitive to even low doses of Thyrolar. In fact, the condition is rare enough that virtually no GPs, and only a few endocrinologists, know of its existence. Apparently, it does not have an official name attached to it. I decided to refer to it as “HAIT anxiety syndrome”, although there are a few doctors who prefer to refer to any neurological symptoms accompanying HAIT as “Hashimoto’s Encephalopathy”.
I began to feel a little better between March 2002 and June 2003. I’m not sure why the message about gluten grains had not penetrated before, but by June 2003, the naturopath reminded me again that she had seen a positive result to a test for antibodies to gliadin (one of the two major proteins in gluten grains) in 2002, and that I really should consider removing gluten grains from my diet. This recommendation was based on three factors:
- I had antibodies to the protein gliadin found in wheat and other gluten grains such as rye and barley;
- I had anti-thyroid antibodies which were over the threshold that defines HAIT;
- Medicine really is an experimental science, and this experiment, in spite of its inconvenience, appeared to be worth a try.
In a numbers sense, the response of my anti-thyroid antibodies to the removal of gluten grains from my diet was slow, but gratifying. My thyroperox test started off at 25, dropped to 19 within 6 months, 7 within 10 months, and became zero in less than 2 years. I eventually concluded that the removal of gluten grains from my diet was not all that difficult, partly because I wasn’t a celiac who had to worry about that last 1%. I also concluded that removal of gluten would have a positive health effect in terms of the reduced glycemic index of the foods I consumed.
My symptomatic improvement thereafter was not immediate. It soon became obvious that T3/T4 treatment is not an exact science, and the proportion of T3 to T4 needs to be closer to the human body’s need, not the pig’s need (Both Armour and Thyrolar have the T3/T4 ratio of one part T3 for every four parts T4, typical of the pig’s biochemistry). For instance, in late 2003, my TSH had dropped very low, i.e. I had become clinically hyperthyroid due to excess T3 as revealed by a free T3 test. I have since gone through a couple more of these “yo-yo” episodes while being treated, which is a not uncommon event—thyroid treatment is as much art as science.
Cost of treatment also became a problem. By June 2004, I began seeing a highly-recommended Physician’s Assistant (P.A.), who was known locally to be very good at thyroid treatment, and whose clinic would accept my health insurance. I continued to see the naturopath, although at less frequent intervals, since my insurance (like most) would pay nothing for naturopathy. The P.A. and the naturopath did not completely agree on treatment methods, particularly the use of adrenal supplements (hydrocortisone and DHEA in low/biologic doses) along with thyroid supplements; but they were both in agreement that I should continue to pursue combination T3/T4 therapy. So, I blended recommendations from the two for awhile, transitioning to T3 and T4 in separate tablets of Cytomel and Synthroid, so the percentage of T3 could be altered.
I gradually transitioned off adrenal supplements during 2005, and very gradually increased my T3/T4 supplementation over the course of the year. Finally, by September 2005, I began to realize that I truly had recovered my health—I had episodes of feeling really good again! Still, my sleep was not perfect—I had discovered what Ridha Arem M.D. has documented in the book Thyroid Solution: a return to the euthyroid state may not immediately eliminate all symptoms. After going to a small dose of the atypical anti-depressant mirtazapine, I finally could feel, every day, like I had in my 30s. Unfortunately, it had taken an agonizing 14 years to get there.
Today, I religiously take my 10 micrograms T3, and 75 micrograms T4, split into two doses each day. I also religiously avoid all traces of gluten grains in my diet because I now understand that the gluey, hard-to-digest proteins in them are a substance which can cause major metabolic disruption. Like the co-author of the book “Dangerous Grains”, Ron Hoggan, with whom I have corresponded, I have come to realize that our society’s over-use of a potentially toxic substance isn’t just dangerous to the 1 in 133 people who have full-blown celiac disease—it can cause a very poor quality of life for the approximately 1 in 5 who have gluten intolerance. I have also come to the realization that, to those few who are unlucky enough to encounter the HAIT Anxiety Syndrome, you may require combination T3/T4 therapy to feel better; and, you may never feel as well as you did when you were young, unless you find a way to stop your immune system from waging war on your thyroid.
Most of all, 14 years after it started, I feel as though a significant part of my life has been taken from me. I was unable get joy or pleasure from life, I was unable to work effectively, and I was unable to be the kind of parent I could have been between my 45th and 59th years of life.
I never imagine that I would be looking forward to the relatively advanced age of 60. However, given that I now feel better than I did at anytime between the ages of 43 and 59, 60 looks like a good place to be.
Summary:
In retrospect, the most important things I ended up learning from 14 years of very unpleasant experience are:
- If you have psychiatric symptoms, e.g., depression, anxiety, panic disorder, etc., make sure your endocrine system is evaluated, with thyroid testing as the cornerstone. Beware of doctors who offer an antidepressant first thing, without endocrine evaluation.
- The emotional/psychiatric effects of hypothyroidism are just as important, and just as damaging, as the physical ones. Unfortunately, many MD’s focus on the physical.
- If you want to get well, you have to apply all your skills and intelligence to investigating your problem, which most MD’s may not understand. You may also have to turn to “alternative” practitioners.
- If your TSH is above 3.0, or maybe even 2.5, and your doctor will not do more comprehensive testing (e.g. FT3/FT4), and/or try a test run of thyroid supplementation, find another doctor.
- If your doctor diagnoses you as hypothyroid, demand that a test for anti-thyroid antibodies be done. If you have any antibodies, even if they are under the threshold where HAIT is considered to start, get testing for allergy to foods, and testing for allergy to common environmental toxins if food testing reveals nothing. You may find, as did I, that you won’t feel as well as possible until you free your body from antibodies.







Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now