
Celiac.com 10/16/2015 - Y Net News, under their "Health & Science" banner, published an article titled "Open Original Shared Link", on April 17, 2015 (1). ALS refers to amyotrophic lateral sclerosis, or Lou Gehrig's disease, also known as motor neuron disease. Authorship of this article is attributed to the news agency, Reuters. The article refers to a study in which the investigators identify an autoimmune dynamic in the brain (2). The Y Net News article quotes one of these investigators as warning ALS patients against experimenting with a gluten-free diet: "Patients should not be tempted to use a gluten-free diet without clear evidence for antibodies, because an unbalanced diet might harm"(1). This is the kind of advice that frequently appears in the popular media. There can be little doubt that a gluten-free can be unhealthy, just as gluten containing diets can be unhealthy. When contacted on this issue, Dr. Drory said that "Patients with ALS tend to lose weight due to symptoms of their disease and it is well known that weight loss has a negative influence on disease progression and survival. Therefore it is very important for these patients not to lose weight" (3). Although Dr. Drory did not mean to impugn the gluten-free diet for the general population, she is legitimately concerned about the longevity and health of ALS patients, so she believes that only those with positive antibody tests should try the diet, and then only under the supervision of a dietitian. Reuters, on the other hand, have not responded to my request, through Y Net News, to contact the author of this article.
While Dr. Drory's concerns are reasonable, I think that she has missed an important feature of the gluten-free diet and she puts too much faith in the connection between TG6 and ALS [an abbreviation for a recently discovered enzyme named tissue transglutaminase six] apparently believing that it will identify all ALS patients who might benefit from avoiding gluten. However, if we can judge based on those who have celiac disease, it is a diet that is more likely to increase the body mass of someone who is underweight. Dr. Drory also seems to have missed the sentiment expressed in the abstract of her own report. It says: "The data from this study indicate that, in certain cases, an ALS syndrome might be associated with autoimmunity and gluten sensitivity. Although the data are preliminary and need replication, gluten sensitivity is potentially treatable; therefore, this diagnostic challenge should not be overlooked" (1). Thus, when dealing with an otherwise irreversible and unstoppable disease, patients are cautioned not to try the diet without these marker antibodies which the authors identify as "preliminary" findings.
Celiac.com Sponsor (A12):
Dr. Drory's caution also assumes that dietitians will generally be competent to guide the ALS patient in their gluten-free diet. However, it is important to recognize that the neurological patient needs to be even more strict with the diet than a person with celiac disease, and there are many uncertainties and debates around this diet. The average dietitian may not be up to date with the application of the gluten-free diet for such conditions, or the relevant controversies, or their application. Also, the beneficial results of a gluten-free diet are widespread across so many ailments and much medical research currently lags well behind patients' positive experiences. This is what has led to the continuing debate about the frequency and importance of non-celiac gluten sensitivity. Until very recently, it was usually given no attention at all. Further, since "gluten sensitivity is potentially treatable," and the current life expectancy for an ALS patient is about 2 years, it seems irresponsible to warn patients to wait for further research results before trying a gluten-free diet.
This latter sentiment captures the essence of my current view of the gluten-free diet. Until I was diagnosed with celiac disease, more than twenty years ago, I would have ignored Dr. Drory, and subscribed to the bias inherent in the Y Net News article. Sadly, I used to dismiss people who talked about diet in the same way that I responded to those who talked about "astro travel" and Astrology. I viewed them as foolish concepts that were popular fads among drug-crazed hippies of the 1960s and 1970s, and other similarly deranged individuals. I still question many other diets, astro travel, and Astrology, but hope I do not do so with the same arrogant certitude of my youth.
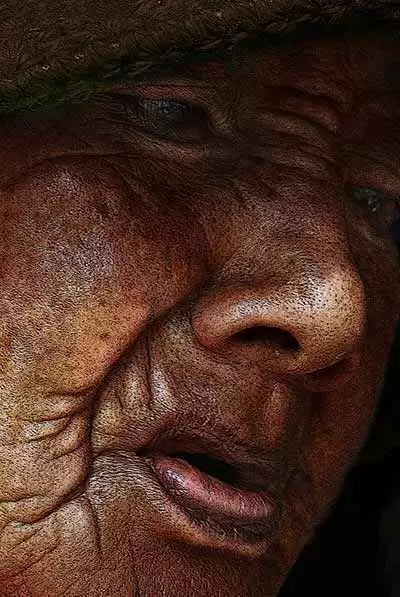
You see, I experienced a startling change of perspective shortly after I was diagnosed with celiac disease. Just three days after beginning the gluten-free diet, I awoke to an altered state of consciousness. The closest I can get to describing it is that I felt somewhat like I remember feeling as a kid when I awoke on Christmas morning. I felt optimistic, hopeful, and I looked forward to the day ahead. That was a big change. I was used to waking up feeling tired, depressed, and usually with a sense of foreboding about the coming day. I also found, after about the first six months or so of avoiding gluten, that my mind was becoming sharper, I was more aware of my surroundings, and my memory seemed to improve. My reflexes also seemed quicker. My sense of balance got better and my reaction time was faster. When I looked at others, I saw that many people were similarly challenged and didn't seem to be aware of their limitations—or perhaps they had just become used to them. Thus, I now believe that many people unknowingly suffer from the myriad harms induced or facilitated by gluten consumption. I also see, given the many venues in which the diet made a difference for me, why others might be skeptical.
But how did Dr. Drory get from the notion that since gluten sensitivity is treatable, and should therefore be investigated as a potential factor in some cases of ALS, to the notion that ALS patients should be cautioned against experimenting with a gluten-free diet because it can cause weight loss? The gluten-free diet can be an effective weight loss strategy for some people. As I have mentioned in previous columns, the gluten-free diet seems to reduce the appetites of overweight individuals with celiac disease by about 400 calories per day. Equally, underweight celiac patients usually gain weight. Dr. Drory's concern about weight loss for those with ALS might be well founded if it was a universally good weight loss strategy. But it isn't. The data regarding weight loss on a gluten-free diet are only available, to my knowledge, with regard to celiac patients, where underweight patients almost always gain weight and about half of overweight patients lose weight. She also thinks that experimentation without a positive antibody test and the oversight of a dietitian might be risky. So her concerns may not be as valid as they first appear. If those ALS patients are gluten sensitive, then they might behave similarly to those with celiac disease, at least with regard to weight gain and loss. Further, how can anyone say, without trying it, that a gluten-free diet would not benefit those ALS patients who do not show TG6 antibodies?
The Reuters article goes on from there to state: "It’s also worth remembering that an association is not the same as a cause. At least one earlier study concluded that there was no association between TG6 antibodies and either neurological disease or gluten itself" (1). The preceding comment refers to a retrospective research report in which the records of patients, on a Swedish data-base, who had been diagnosed with celiac disease, were further examined for an additional diagnosis of ALS (4). This is more than a little strange, since the very study the Reuters journalist used to distinguish between associations and causality, seeks only evidence of an association between the ALS and celiac disease. The notion that correlation is not causation is valid. However, using a study that looks for a correlation between celiac disease and ALS is not a reasonable basis for differentiating between correlation and causation. Neither is it a valid example of a causal relationship.
Further, it is difficult to imagine a study design that would be less likely to reveal an association between transglutaminase TG6 and any other ailment, than one based on recorded data from a large number of patients who were diagnosed with celiac disease between 1969 and 2008. All, or almost all of these patients were diagnosed prior to the first published report of the discovery and diagnostic utility of transglutaminase 6 (5). So if one looks through records that predate the discovery of TG6 to find evidence of a connection between TG6 and any other disease, one is highly unlikely to find it.
The abstract of the study that asserts there is no association between these ailments is based on a very weak design. It also ends with the statement: "Earlier reports of a positive association may be due to surveillance bias just after celiac disease diagnosis or expedited diagnostic work-up of ALS" (4). They are so confident of their own findings that they suggest that contrary findings are either due to bias or fast, careless work. I will leave it to the reader to infer whether there is bias among the authors of this report. Additionally, the Y Net News article, by one or more journalists at the Reuters News Agency, reports that this study found no association between TG6 antibodies and ALS, even though the study in question examines data that predates the use of TG6 antibody testing. While the study in question does appear to claim that there is no connection between celiac disease and ALS, the mention of TG6 and whether there is a connection between these antibodies and ALS appears to be information added by Reuters.
Regardless of this possibly 'added' information, it really is quite a stretch to warn the public or ALS patients of the dangers of a gluten-free diet in reporting about research that has found evidence of a possible connection between ALS and gluten consumption. In a balanced report, the Reuters journalist would have mentioned the seven other research publications that have reported associations, and/or cause to suspect such associations, between gluten and ALS (5-11). It really isn't rocket science. It is just ethical, balanced reporting, which should serve as a minimum standard for an organization that is engaged in reporting the news. Since there are always at least two sides to almost any argument, both sides should at least have been acknowledged. Thus, in addition to the weak study reporting that they didn't find an association, the seven other reports of possible associations really should have been mentioned.
It would also have been informative to their readers to mention Stephen Hawking, the longest living patient who was diagnosed with ALS. Dr. Hawking is still alive and has been on a gluten-free diet for the last 40+ years (12). He had already lived well beyond the two year life expectancy predicted by his doctors when, in 1963, Hawking's ALS had progressed to the point where he had begun to choke on his food. That is when he eliminated gluten, sugar, and plant oils from his diet. He has continued to avoid gluten for all these years and has also added several vitamins and supplements to his diet. Whether any or all of these measures have made "the" life extending difference, or if it is all of these measures combined that have allowed him to continue for so long, we can't know. Nonetheless, it may be that the gluten-free diet has been a determining factor in Dr. Hawking's longevity in the context of ALS. We also don't know if he would have tested positive for TG6 back when he was first diagnosed. However, he might not still be with us if he had opted to wait for this research to emerge and be confirmed.
Since Hawking began his self-directed dietary experiment, researchers at the Royal Hallamshire Hospital in Sheffield, UK, have shown that the TG6 antibodies, while present in some celiac patients, are also found in some patients with non celiac gluten sensitivity and either neurological disease or an increased risk of developing one (5).
Others, reporting a case study, had diagnosed ALS, then identified, diagnosed, and treated co-existing celiac disease with a gluten-free diet. They then retracted their ALS diagnosis saying: "Ultimately, improvement in the patient’s symptoms following treatment for celiac disease rendered the diagnosis of ALS untenable" (6). It would appear that any improvement in ALS symptoms obviates a diagnosis of ALS. It also raises the possibility that some cases of ALS can be effectively treated with a gluten-free diet.
Similarly, in another case study report, the authors state: "ALS is a condition with relentless progression; for this reason, the simple observation of an improvement in symptoms is most pertinent in rendering the diagnosis of ALS untenable" (7). Again, the patient's ALS symptoms regressed following institution of a gluten-free diet.
Yet another report that connects ALS with autoimmunity in general states: "The significance of increased premorbid celiac disease in those with ALS, and in family members of patients with MMN [multifocal motor neuropathy] remains unclear at present."(9). Still others have offered genetic evidence of connections between gluten sensitivity and ALS (10).
Thus, the Reuters article raises an important question. Why are we seeing so many media attacks on those who are taking responsibility for their own health and experimenting with a gluten-free diet? It might come as a surprise to the Reuters journalist to learn that we humans had evolved and spread into most habitable areas of the world long before a few farmers began cultivating grains in regions of what are now known as Iraq and Iran. She/he might also be surprised to learn that we have known, for decades, that variants of wheat, rye, and barley have a deleterious impact on human neurological tissues (13, 14, 15) and that a variety of neurological ailments arise both in the context of celiac disease and non-celiac gluten sensitivity (14).
The conclusion in the abstract of the 'no relationship' study dismisses reports of opposing findings as either due to "surveillance bias" or "expedited diagnostic work-up" (4). (This latter is a euphemistic statement suggesting that the work that led to these other reports was conducted too quickly and errors resulted.) Whatever your personal view of the attitude expressed there, the greater concern may be that the media continue to identify the gluten-free diet as potentially harmful (1) while researchers and individuals experimenting with a gluten-free diet have found evidence connecting gluten sensitivity with, at least, some cases of ALS (2).
Over the years, I have heard many reasons for resisting this diet, but the one that is probably the least defensible is the assertion that it is potentially harmful. Almost any dietary regimen can be hazardous, of course, but the assertion that it might cause a harmful dietary imbalance fails to recognize that gluten has only been part of the Human experience for a very short time, in evolutionary terms. The simple fact is that we humans have spent far more of our evolutionary past eating a gluten-free diet than we have spent eating gluten. Some populations have only been eating these grains since European incursions over the last several hundred years. Some of these populations have only been eating it for less than one hundred years. Still others have been eating gluten for a few thousand years. In Israel, where Dr. Drory's study originated, grains were probably incorporated into the diet much earlier than in most of the rest of Europe, probably sometime between 15,000 and 10,000 years ago. It is difficult to imagine that after hundreds of thousands of years of eating a gluten-free diet, that avoiding gluten can pose a health hazard. The Reuters journalist appears to have another axe to grind, but I continue to wonder why we are seeing so many journalists on the attack against the gluten-free lifestyle?
The driving force behind these journalists' attacks may well be similar to the perspective that I experienced before my diagnosis with celiac disease. Perhaps they suspect, whatever their reasons, that the gluten-free diet has little or no merit, and their only concession is to grudgingly allow that it may be helpful to those with celiac disease. My suspicion is that this attitude is driven by an insecurity. We want to believe conventional wisdom that gluten grains are healthy and that our medical professionals, and the institutions in which they serve, are above reproach. Nobel Laureate, Kary Mullis, is one highly vaunted physician's voice, among many, who dismiss most diets as fads, arguing that we are omnivores whose secret of successful adaptation to a wide variety of environments is the result of our flexibility in sources of nourishment (18). Many of us want to be able to rely on our physicians. We don't want the insecurity of knowing that our medical establishment is a flawed, human institution. The self-directed experimentation with a gluten-free diet poses a threat to that credibility, and hence, our sense of security, especially when it results in improved health. We don't want to feel the resulting uncertainty that comes from doubting the medical cornerstone of our civilization.
It is not long ago that Don Wiss, myself, and others, argued extensively with physicians and researchers who insisted that the rate of celiac disease in the USA was variously one in 12,000 persons or one in 25,000 people. Sometimes these discussions became quite heated. Some of the people posting to these newsgroups were asking for suggestions for how they might proceed with various health complaints. When Don or I saw a post asking about symptoms that had been reported in the peer reviewed literature, in association with untreated celiac disease, we suggested a trial of a gluten-free diet. Some of the physicians and researchers contacted these individuals privately, saying things to discredit us. It seems doubtful that they would not have said such things where they were likely to be held accountable for what they said. Their reactions, I suspect, were driven by a sense of feeling threatened. As soon as controlled testing was done, it became clear that the rate of celiac disease, among Americans, is at least 1 in 133 Americans, and many of those individuals we advised to try a gluten-free diet might well have had celiac disease. Yet many journalists, physicians, and researchers have a great deal invested in the current status quo. Any threat to the established order is likely to incite the ire of many members of these groups.
Thus, while others may consider it prudent to await the end of the current debate about ALS and a gluten-free diet, the ALS patient might be better advised to take dietary steps to ensure against weight loss, while trying a strict gluten-free diet. I know what I would do if were diagnosed with ALS...on second thought, since I've been gluten-free for more than twenty years, maybe I won't ever be diagnosed with ALS. I will continue to hope. In the meantime, Thomas Kuhn clearly outlined this stage of acceptance of new ideas in science (19). We appear to be in the "denial" stage, which is the last one before we can expect the emergence of widespread claims that 'we knew it all along'. If so, then broad acceptance is in the offing, and these nay-saying journalists will move on to some other controversial new discovery, and we can be spared the condescending remarks suggesting that the gluten-free diet is a mere placebo and a 'fad diet' for most of those who follow it.
Sources:
- Open Original Shared Link
- Gadoth A, Nefussy B, Bleiberg M, Klein T, Artman I, Drory VE. Transglutaminase 6 Antibodies in the Serum of Patients With Amyotrophic Lateral Sclerosis. JAMA Neurol. 2015 Apr 13.
- Drory V. Personal communication via email
- Ludvigsson JF, Mariosa D, Lebwohl B, Fang F. No association between biopsy-verified celiac disease and subsequent amyotrophic lateral sclerosis--a population-based cohort study. Eur J Neurol. 2014 Jul;21(7):976-82.
- Hadjivassiliou M, Aeschlimann P, Strigun A, Sanders D, Woodroofe N, Aeschlimann D. Autoantibodies in gluten ataxia recognize a novel neuronal transglutaminase. Ann Neurol 2008;64:332-343
- Brown KJ, Jewells V, Herfarth H, Castillo M. White matter lesions suggestive of amyotrophic lateral sclerosis attributed to celiac disease. AJNR Am J Neuroradiol. 2010 May;31(5):880-1.
- Turner MR, Chohan G, Quaghebeur G, Greenhall RC, Hadjivassiliou M, Talbot K. A case of celiac disease mimicking amyotrophic lateral sclerosis. Nat Clin Pract Neurol. 2007 Oct;3(10):581-4.
- Ihara M, Makino F, Sawada H, Mezaki T, Mizutani K, Nakase H, Matsui M, Tomimoto H, Shimohama S. Gluten sensitivity in Japanese patients with adult-onset cerebellar ataxia. Intern Med. 2006;45(3):135-40.
- Turner MR, Goldacre R, Ramagopalan S, Talbot K, Goldacre MJ. Autoimmune
- disease preceding amyotrophic lateral sclerosis: an epidemiologic study. Neurology. 2013 Oct 1;81(14):1222-5.
- Auburger G, Gispert S, Lahut S, Omür O, Damrath E, Heck M, BaÅŸak N. 12q24
- locus association with type 1 diabetes: SH2B3 or ATXN2? World J Diabetes. 2014
- Jun 15;5(3):316-27.
- Bersano E, Stecco A, D'Alfonso S, Corrado L, Sarnelli MF, Solara V, Cantello
- R, Mazzini L. Coeliac disease mimicking Amyotrophic Lateral Sclerosis. Amyotroph
- Lateral Scler Frontotemporal Degener. 2015 Feb 3:1-3.
- Hawking J. Travelling to Infinity: My Life with Stephen. Alma Books, Richmond, UK. 2014.








.webp.590589ca4138c4074eca33f41f5233ba.webp)




Recommended Comments