
Scrapmanson
-
Posts
27 -
Joined
-
Last visited
Content Type
Profiles
Forums
Events
Blogs
Celiac.com - Celiac Disease & Gluten-Free Diet Support Since 1995
Posts posted by Scrapmanson
-
-
1 minute ago, Scott Adams said:
It looks like that is the test, but to be sure ask your doctor. The next step for you will likely be a follow up endoscopy/biopsy. Be sure to keep eating gluten daily until all of your tests are completed (2 slices of wheat bread's worth for at least 6-8 weeks before any blood tests, and 2 weeks before an endoscopy).
I've had 2 endoscopys over the past couple yrs, both negative. Still hunting for answers. 😢
-
1 hour ago, Scott Adams said:
I think you mean the DGP-IgA test. Please see this article:
Thank you, I read thru it and it's so confusing. I'm not sure the difference or which test I got for the deamidated gliaden iga.... There's 2 that are similar in the group.
1 DGP-IgA and DGP-IgG (Deamidated Gliadin Peptide) blood test for celiac disease
2 Gliadin Peptide Antibody IgA (Immunoglobulin A)
My positive test from this post is diam gladian peptide iga. I also just tested more stuff a few days ago waiting on results because I haven't figured anything out.
New test consists of
Deamidated Gliadin Abs, IgA
Deamidated Gliadin Abs,
t-Transglutaminase (tTG) IgA
t-Transglutaminase (tTG) IgG
Endomysial Antibody IgA
Immunoglobulin A, Qn, Serum result 152
-
On 9/9/2022 at 3:43 PM, Scott Adams said:
It only takes one positive test for celiac disease for you to have it, so at this point you could keep eating gluten and ask your doctor to get an endoscopy to try to verify the diagnosis, or you could try going gluten-free to see if your symptoms resolve.
You say it only takes 1 positive test, does that include the deam gliaden aga?
-
11 minutes ago, gluten-free-Cate said:
If you have NCGS, it can definitely cause pain and many of the same issues as celiac. However, unfortunately, there is no official diagnostic testing for NCGS; it is a diagnosis of ruling other things out. If you've completed all of your celiac testing, it is certainly worth a try to go gluten-free and see how it makes you feel.
You may even want to do a trial of an eating style that eliminates more than gluten, such as the AIP diet or Whole 30, to eliminate as many allergens/irritants/inflammatory foods as possible and lower systemic inflammation for a few months (or more) to see how your body responds and if you get any relief.
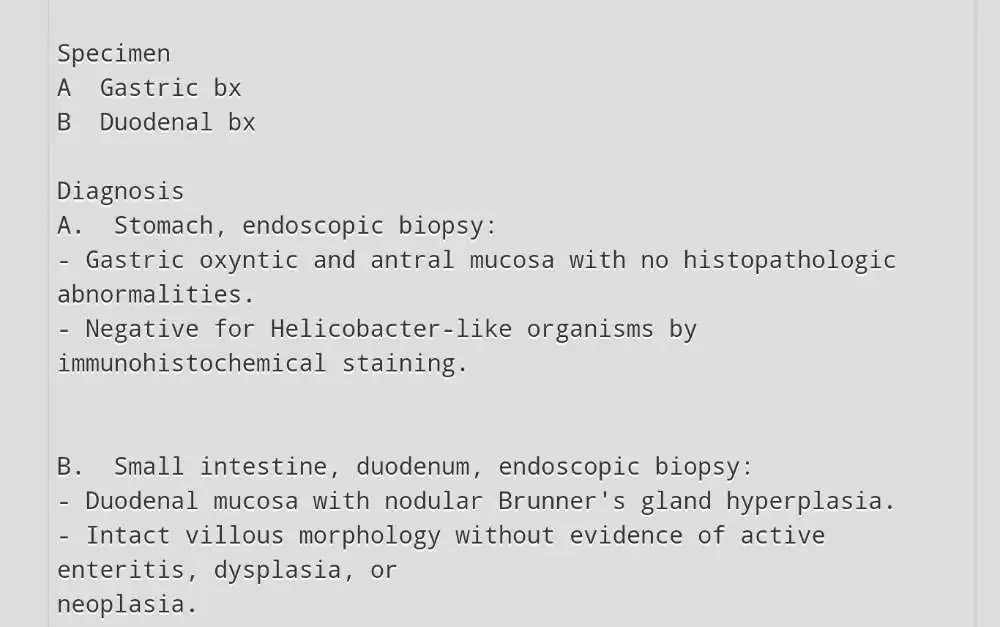
On your other post with your endoscopy results, it looks like they identified Brunner’s gland hyperplasia if I am reading it correctly? Have you already met with your gastroenterologist about that and and whether it could be contributing to your symptoms (it's not something I've ever heard of and a quick google search doesn't yield much info)?
Yeah he pretty much said it doesn't mean anything.... I'm at a loss.
-
4 hours ago, Scott Adams said:
Were you eating 2 slices of wheat bread or equivalent for at least 2 weeks before the endoscopy? If not your results could be a false negative. Did they take at least 4 samples?
The positive blood test result and your symptoms still means you could have celiac disease or non-celiac gluten sensitivity (there is no test yet for this).
Yes I was still eating gluten. There were more than 4 samples.
-
10 minutes ago, Scott Adams said:
It only takes one positive test for celiac disease for you to have it, so at this point you could keep eating gluten and ask your doctor to get an endoscopy to try to verify the diagnosis, or you could try going gluten-free to see if your symptoms resolve.
I did endoscopy already, negative
-
2 minutes ago, Scott Adams said:
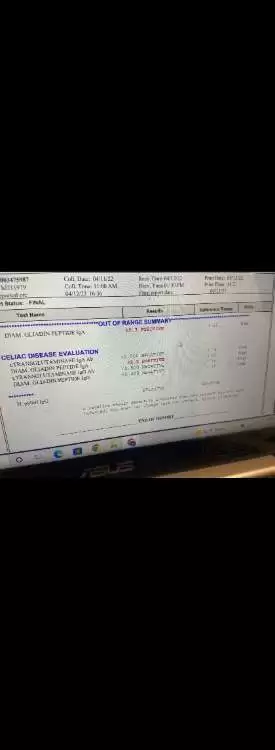
I'll have to trust you on this...the text in the image is too small for me to read.
tt iga neg
Tt igg neg
Diam igg neg
Diam iga pos 22.5 range <15
-
26 minutes ago, Scott Adams said:
Feel free to share your test results here, along with the reference ranges for positive. If you had a single positive test for celiac disease then you could have celiac disease. The normal process if you get a positive blood test would be to get an endoscopy to confirm celiac disease, and you would need to keep eating gluten until all testing is completed. If you feel that you can't eat gluten for a few weeks then perhaps just try the diet for a few months and see if your symptoms go away. Let us know how things go!
Here's my results, I already had endoscopy and it was negative.
-
1 hour ago, RMJ said:
Since you did have a positive deamidated gliadin peptide IgA you could try a gluten free diet for a few months and see if you feel better. You don’t need a doctor’s permission to do that!
OK, I'll try anything at this point. Could that cause all these issues and pain?
-
-
Please Can anyone help me out? My Dr said I'm negative and now says sibo... I'm so confused and in pain all the time! Just had another blood test and the diam gladian iga was still above normal, my biopsy was negative. Please does anyone have ideas or can help me out?? I'm so tired of hurting and no answers! White tongue, abdomen and back pain, bloating, tons of gas...
-
Well had my appointment yesterday, Dr said everything is normal..... Like how is that even possible! Now he's thinking either sibo or pancreatic enzyme issues
-
38 minutes ago, trents said:
Hyperplasia of the Brunner's gland means it is enlarged. These glands reside in the small bowel
"Brunner’s glands are duodenal glands localized predominantly in the submucosa of proximal duodenum. They secrete alkaline fluid composed of mucin (Muc-6) which protects duodenal epithelium by counteracting the acid chime from stomach".
It is possibly working overtime to counteract excess acid in the stomach? Earlier in the thread you describe a problem with burning in your stomach.
Thank you! Yeah I get burning in abdomen, bloating, abdomen pain, lots of gas, my tongue is white and sore... But I don't get acid reflux
-
1 minute ago, trents said:
Nope, doesn't look like celiac disease but if you have celiac-like symptoms you may very well have NCGS (Non Celiac Gluten Sensitivity).
Thanks, kinda freaked out with what the other stuff says or means in the biopsy, tried googling but it's pretty confusing.
-
OK guys finally got my results back, doesn't llok like celiac from what I'm reading but I don't see my Dr for like 2 months so I'm kinda freaking out with what this says.... Heres my biospy report...

-
Just finished with my endoscopy, Dr wanted to check for celiac, so took biopsy but here's what it says, wondering what all this kinda means? Does this stuff indicate posible celiac? So freaked about about stomach cancer!
Impressions: normal esophagus, gastritis, duodenitis.
Scattered moderate inflammation characterized by congestion (edema), erythema, and friability was found in gastric antrum.
Scattered mild inflammation characterized by congestion (edema) was found in duodenal bulb.
Said to see him in 4 weeks...wont know results till then.
-
3 hours ago, Wheatwacked said:
Hi , confusing times. How is your daughter doing? You have several indicators of malabsorption syndrome. Your stool could be choline deficiency whiich could be simply not eating enough or not absorbing it. The RDA (the mininimum required to stay healthy) is 3 large eggs a day. B12, B6, Choline, Folate and homocysteine blood tests would help identify.
1. Vitamin D Deficiency: A study with 434 people found that lower blood vitamin D levels were associated with high MPV [18]. https://labs.selfdecode.com/blog/mpv/
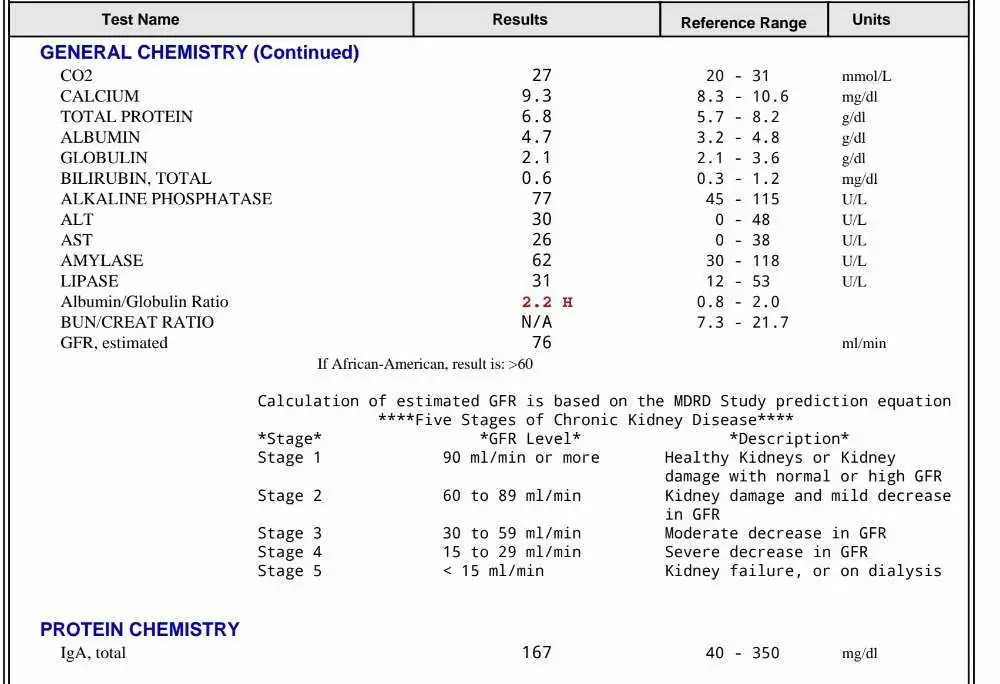
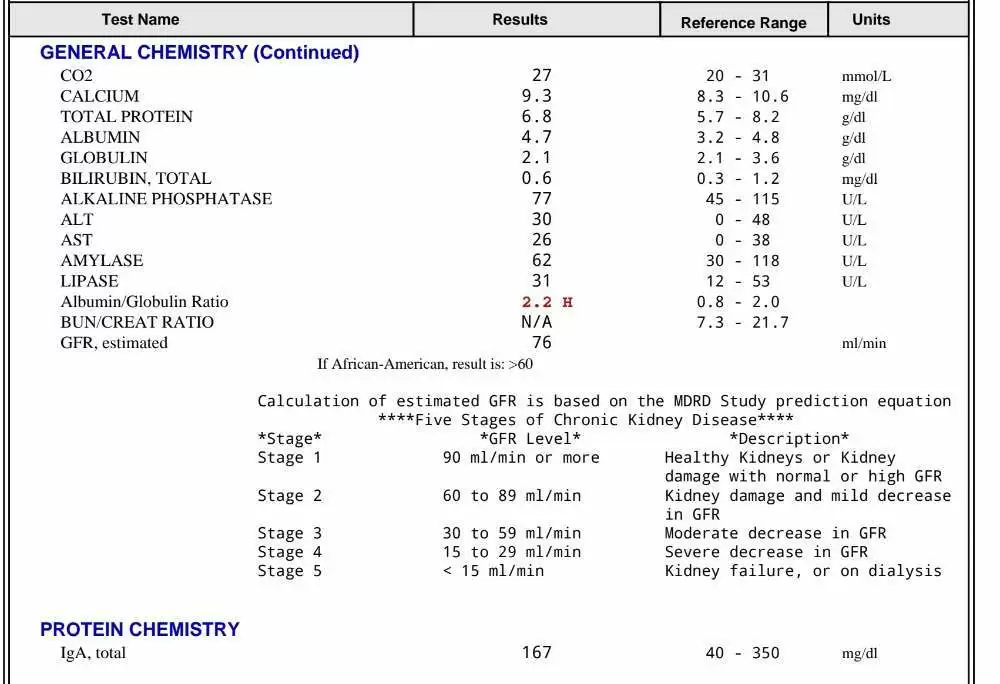
"A total protein and A/G ratio test is often included as part of a comprehensive metabolic panel, a test that measures proteins and other substances in the blood. It may also be used to help diagnose kidney disease, liver disease, or nutritional problems." https://medlineplus.gov/lab-tests/total-protein-and-albumin-globulin-a-g-ratio/
Smelly and sticky stools are typically a symptom of nutrient malabsorption. This means your body isn’t able to completely absorb and digest nutrients from your gastrointestinal tract due to damage to the small intestine, not having enough pancreatic enzymes, liver disease, HIV/AIDs, or other conditions. https://www.webmd.com/digestive-disorders/what-to-know-about-floating-stools#:~:text=Smelly and sticky stools are,%2FAIDs%2C or other conditions.
"A high A/G ratio suggests underproduction of immunoglobulins as may be seen in some genetic deficiencies and in some leukemias....Following an abnormal total protein result and depending on the suspected cause, more specific tests are typically performed to make an accurate diagnosis. Some examples include liver enzyme tests, renal panel, serum protein electrophoresis, or tests for celiac disease or IBD. " https://www.labcorp.com/help/patient-test-info/total-protein-and-albuminglobulin-ag-ratio
My daughter is good now, Thanks for asking. My total protein is Good. I did a total iga to see if that was deficient to see if that's why my Ttg tta didn't show positive, but it came back normal. So only things off was diam peptide of 22.3, and aga ratio barely high by .1
-
On 6/28/2022 at 5:23 AM, Russ314 said:
I wouldn't call it very odd as there is so much variation between people. See what happens with your IgA test and endoscopy
A paper quoted in this review states:
The celiac disease That Pays Dividends: More Than 15 Years of Deamidated Gliadin Peptide Antibodies
So, it is certainly possible to have -ve tTG IgA with +ve DGP IgA and have coeliac disease.
I got my iga back came back normal 167
Range 40-350
Only thing came back in my entire blood test off was. Albumin/globulin ratio high of 2.2 in range 0.8 to 2.0
-
-
22 minutes ago, Russ314 said:
Coeliac disease has a complicated and not completely understood immune process. On top of that, individuals respond very differently.
One of the proteins within gluten called gliadin is resistant to digestive enzymes and is not completely broken down to short peptide chains for absorption. The remaining large fragments are quite immunogenic. If it gets into the wall of the gut, one of the known fragments binds to an enzyme called tissue transglutaminase (tTG). As well as binding to the gliadin fragment, tTG removes an amide group creating a positively charged complex that is highly immunoreactive. Immune cells chomp this complex up and present the components to other immune cells, leading to an immune response both to gluten and tTG. It is a complicated process but it bypasses the mechanisms to avoid self tolerance i.e. responding to tTG.
When the complex is chomped up for immune response, one of the things that is recognised is deamidated gliadin. Your results show a low positive to this but not to tTG. Low positive tTG can be caused by various conditions such as liver inflammation and Crohn's disease.
A low positive DGP alone is curious.
Thanks for the detailed resp.... So r u saying it's very odd to only have low dgp? Should I get other tests done or maybe look elsewhere for diagnosis? My original endoscopy was negative for celiac a couple yrs ago... I'm serious so done with not knowing what is actually going on, thought I was finally finding an answer to feeling so bad all the time... Heres my test results

-
7 minutes ago, Russ314 said:
That is curious. In children, DGP can show before tTG antibodies. You are an adult and have been symptomatic for 7 years and yet have a borderline positive DGP but no tTG.
If you are IgA deficient, you are not showing up on IgG so that would be perplexing.
Interesting.
Why perplexing? What r your thoughts on this? I have no idea, unless there's something else that can show slightly high dgp?
-
12 minutes ago, Russ314 said:
I take it the later 2 tests are for deamidated gliadin peptide antibodies? If so, do you have the standard range for the positive one?
Yes it's also <15
-
1 minute ago, trents said:
Because the Diam iga is positive, you could be a celiac even though the tTG-IGA is negative, especially if the total serum IGA turns out to be low. Were you eating regular amounts of gluten (2 slices of wheat bread daily or the equivalent) for 6-8 weeks prior to the blood tests? Don't cut back on gluten until all testing is complete.
Yeah I've never been gluten free so I've always ate normal. That's kinda why I went and got this other total iga test. If that comes back low then it leans toward celiac if it's normal then?
-
Just now, trents said:
What about NCGS?
That's kinda why I'm asking if my tests look like celiac or something else?

So confused!
in Celiac Disease Pre-Diagnosis, Testing & Symptoms
Posted
No I don't think so.... Does it cause extreme symptoms as well?