Celiac.com 12/15/2015 - Newly diagnosed with celiac disease, late in 1993 or early in 1994, I was reading a paper that turned my perception of this disease upside down. I learned that it takes more than susceptible genes and eating gluten to cause celiac disease. There is some added, as yet unknown factor in the onset of celiac disease. The report I was reading suggested that a fairly common viral infection might be that missing co-factor. It went on to say that 89% of subjects with untreated celiac disease also showed blood evidence of a particular viral infection called adenovirus 12, while fewer than 12% of control subjects showed evidence of past or present infection with this virus. It is a microbe that makes its home in our small intestines. The report went on to say that this particular virus contains an amino acid sequence that is identical to a sequence that forms part of a protein in gliadin, which is found in wheat, while similar proteins with the same triggering impact on our immune systems are also found in rye and barley. I was electrified by this insight. It offered a window through which I could begin to understand this enigmatic disease that made me react to a food that almost everyone I knew seemed to tolerate without any problems.
I looked to see who had written the article. The lead author was listed as M. F. Kagnoff, but my attention was drawn to Donald Kasarda’s name, also listed as an author, because I had seen that name before. Several years later, I attended a CSA/USA conference in Seattle. The name of one of the speakers was familiar. After a little checking, I realized that he was the lead author of the study that had touched off my imagination.
Celiac.com Sponsor (A12):
Dr. Kagnoff’s lecture followed immediately after a presenter who had repeatedly asserted that celiac disease is a very difficult diagnosis. Almost as soon as he got up on stage, Dr. Kagnoff said something to the effect that celiac disease is only a difficult diagnosis if you aren’t looking for it. The room suddenly became very quiet.
The presentation went well, and he outlined the criteria for diagnosing celiac disease, and stated why he felt that it was a simple diagnosis. The speaker who followed him began by stating that celiac disease is a difficult diagnosis, despite Dr. Kagnoff’s assertions to the contrary. I left that conference with a strong sense of appreciation for Kagnoff on several levels: as a gastroenterologist, as a researcher, and as an independent thinker who was quite willing to offer a dissenting opinion where he disagreed.
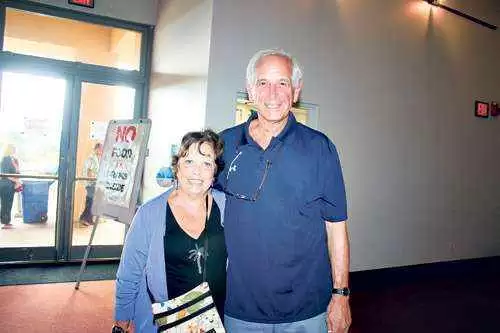
Six or seven years later, a mutual friend introduced me to Marty Kagnoff at a cocktail party in New York city. It was a pleasure to finally meet him in person. I told him that I was most impressed with, and intrigued by his work with adenovirus 12. I also told him that I enjoyed hearing his assertion, at the Seattle conference, that celiac disease is a simple diagnosis. He seemed a little surprised that I was aware of his research from more than twenty years previous, and he said that his work had been eclipsed by newer work that explored other infectious agents. He was interesting and interested, and the three of us engaged in a lively discussion about some of the politics regarding celiac disease and its diagnosis. He was brilliant, creative, and independent; all the things that a researcher should be.
His passing is a huge loss to the medical profession, the celiac and gluten sensitive community, as well as to the biological research community. His contributions and discoveries shaped much of what we now understand about celiac disease, the intestinal mucosa, and intestinal immunity.
Source:
- Kagnoff MF, Paterson YJ, Kumar PJ, Kasarda DD, Carbone FR, Unsworth DJ, Austin RK. Evidence for the role of a human intestinal adenovirus in the pathogenesis of coeliac disease. Gut. 1987 Aug;28(8):995-1001












Recommended Comments