
Celiac.com 11/17/2025 - This study explored an important question: among people who have celiac disease, do those who are prescribed angiotensin receptor blockers—a common group of medications used to treat high blood pressure—experience different health outcomes compared to those who do not use these drugs? The researchers discovered that individuals with celiac disease who took angiotensin receptor blockers had higher chances of developing issues such as low blood count, iron deficiency, abdominal pain, and ongoing diarrhea. These findings suggest that the use of this medication class may be linked to worse intestinal health in those living with celiac disease.
Why the Researchers Did This
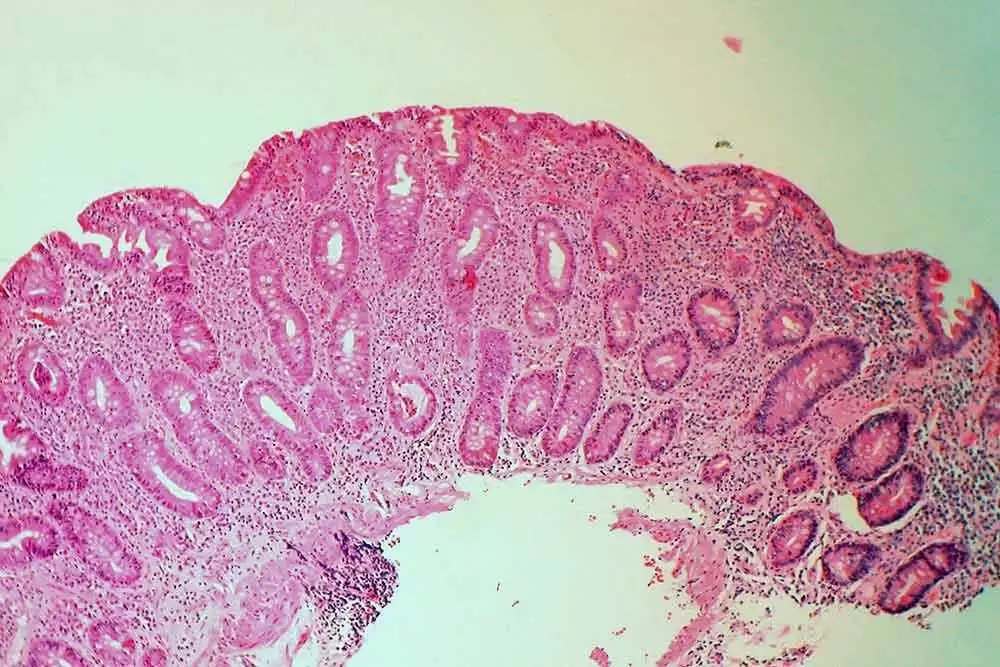
Doctors have long known that one specific drug in this category, olmesartan, can sometimes cause a condition that mimics celiac disease. People who take olmesartan may develop symptoms such as weight loss, chronic diarrhea, and damage to the small intestine lining—symptoms nearly identical to those seen in untreated celiac disease. Because of this similarity, scientists began wondering whether other angiotensin receptor blockers might also harm the gut, especially in people who already have celiac disease. The purpose of this study was to investigate whether there was any connection between the use of these medications and poorer outcomes in people diagnosed with celiac disease.
How the Study Was Conducted
Celiac.com Sponsor (A12):
Researchers analyzed data from a large group of individuals diagnosed with celiac disease. They identified nearly two thousand patients in total, and out of those, a few hundred had been prescribed angiotensin receptor blockers. The research team followed both groups over time to monitor for key outcomes such as anemia (low red blood cell levels), iron deficiency, chronic diarrhea, and abdominal discomfort.
By comparing the medical histories and outcomes between people who took these blood pressure medications and those who did not, the researchers could assess whether there were consistent differences. They controlled for other factors such as age, sex, and other health conditions that might influence results.
What the Researchers Found
People with celiac disease who were prescribed angiotensin receptor blockers were significantly more likely to develop certain complications than those who were not prescribed the medications. These included:
- Lower levels of hemoglobin, indicating possible anemia.
- Increased rates of iron deficiency, suggesting problems with nutrient absorption.
- Higher frequency of abdominal pain and persistent diarrhea.
Taken together, these results point to the possibility that angiotensin receptor blockers may worsen intestinal function in people with celiac disease or mimic symptoms that resemble active disease even when gluten is avoided.
Possible Explanations
One theory is that these medications may interfere with intestinal cell signaling or immune regulation in the gut. The small intestine is already vulnerable in celiac disease because of immune-related inflammation caused by gluten. If these drugs further disrupt how intestinal cells communicate or heal, they could prolong or intensify inflammation and tissue damage.
Another idea is that some angiotensin receptor blockers, especially olmesartan, may directly trigger an immune reaction that damages the lining of the intestine. This reaction may be rare but could explain why some people develop severe intestinal symptoms while taking these drugs.
What the Results Mean for Patients
For people living with celiac disease, these findings raise awareness about potential medication-related complications. It does not mean that everyone with celiac disease should stop taking blood pressure medication, but it does suggest that doctors should monitor patients carefully. If someone with celiac disease begins to experience recurring diarrhea, abdominal pain, or unexplained anemia despite following a strict gluten-free diet, their medication list—including angiotensin receptor blockers—should be reviewed.
Alternative blood pressure medications may be considered if intestinal symptoms persist or worsen after starting these drugs. More research is needed to confirm whether all angiotensin receptor blockers pose similar risks or if only specific drugs in the class are problematic.
Limitations of the Study
Because this research relied on patient records, it could not prove direct cause and effect. There might be other reasons why people who take these medications have worse outcomes, such as underlying heart conditions or differences in overall health. Nonetheless, the consistency of the pattern across many patients makes the finding noteworthy and worth exploring further in future clinical studies.
Why This Study Matters
For people with celiac disease, this study highlights the importance of looking beyond diet alone when managing health. Even with perfect gluten avoidance, some medications may interfere with gut healing or mimic active disease. Understanding these interactions can help patients and doctors make better choices about treatment plans.
It also encourages healthcare providers to think more holistically about persistent symptoms. When fatigue, nutrient deficiencies, or intestinal upset continue despite a gluten-free diet, it may not always mean gluten exposure—it could also reflect how medications interact with the digestive system.
Key Takeaways
- Angiotensin receptor blockers, a class of blood pressure drugs, were linked to worse outcomes in people with celiac disease in this study.
- These patients had higher rates of anemia, iron deficiency, and intestinal symptoms such as diarrhea and abdominal pain.
- Doctors should be aware of this possible connection and review medication lists when patients have ongoing digestive problems.
- Further research is needed to clarify whether specific drugs or doses cause these effects and to explore safer alternatives.
Conclusion
This study provides valuable insight into how common blood pressure medications might interact with the intestinal health of people who have celiac disease. It reminds both patients and healthcare professionals that healing involves more than diet alone. Careful medication review and personalized management could help reduce ongoing symptoms and improve quality of life for those with celiac disease.
Read more at: researchgate.net










Recommended Comments
There are no comments to display.
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now