Celiac.com 01/07/2026 - This study explores an entirely new way to diagnose celiac disease and its earliest form, potential celiac disease, using only a small blood sample. By combining infrared spectroscopy with advanced deep learning, the researchers created a method that may be faster, less invasive, and more accurate than traditional diagnostic approaches.
Background: Why Diagnosing Celiac Disease Is Difficult
Celiac disease is an autoimmune condition in which eating gluten triggers the immune system to attack the lining of the small intestine. This damage can lead to digestive problems, nutrient deficiencies, fatigue, bone loss, and many other symptoms. Traditionally, diagnosis requires a combination of blood tests and an intestinal biopsy taken by endoscopy. Biopsies are considered the gold standard, but they are invasive, expensive, and not always available in all parts of the world.
Celiac.com Sponsor (A12):
There is another category called potential celiac disease. These individuals show immune signs of celiac disease and have the same genetic risk, but their intestinal tissue may appear normal or only slightly inflamed. These early changes are difficult to identify, and many people with potential celiac disease eventually progress to the full form of the condition. Because their symptoms can be mild or unpredictable, diagnosing potential celiac disease accurately and early is especially challenging.
This study set out to address these challenges by exploring whether the unique chemical “fingerprints” found in a person’s blood could reveal whether they have celiac disease, potential celiac disease, or no disease at all.
Using Infrared Light to Detect Disease Signals in Blood
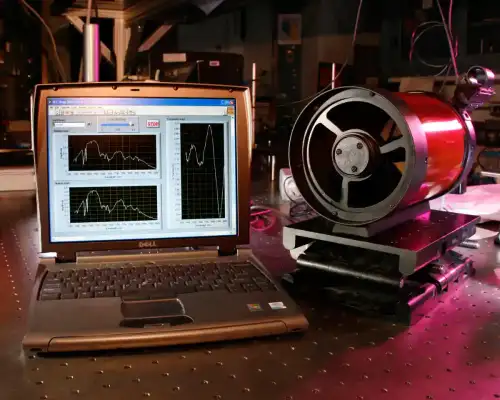
The researchers used a technique called Fourier-transform infrared spectroscopy. In simple terms, this method shines infrared light through a drop of serum taken from the blood. Different molecules—such as fats, proteins, and nucleic acids—absorb the light in different ways. This pattern of absorption creates a detailed “spectral fingerprint” that reflects the molecular composition of the sample.
Because celiac disease disrupts immune activity, nutrient absorption, fat processing, and inflammation, the composition of the blood changes. These changes may be too subtle for a human to detect by reading a spectrum, but advanced computer algorithms can recognize patterns hidden within the data.
Why Deep Learning Was Essential
Infrared spectral data is extremely detailed and contains both useful information and background noise. Traditional statistical tools can analyze some parts of the spectrum, but they often miss faint signals or cannot combine many layers of information at once.
To solve this, the researchers built a deep learning system with two specialized branches. One branch focuses on global patterns across the entire spectrum, capturing long-range relationships between different wavelengths. The other branch highlights smaller, more focused features that appear in specific parts of the spectrum. By combining both types of information, the model can pay attention to subtle changes that separate the three groups—celiac disease, potential celiac disease, and healthy individuals.
This design helps the model recognize even faint disease signals that would normally be hidden by noise or too complex for older techniques.
What the Spectral Data Revealed
When comparing spectra from individuals with celiac disease, potential celiac disease, and healthy individuals, the research team found clear differences in several regions. These variations appear to reflect shifts in important biological processes:
- Changes in lipid-related signals, likely linked to impaired fat absorption caused by damaged intestinal villi.
- Increases in markers connected to inflammation and oxidative stress, which are common in immune-driven intestinal injury.
- Alterations in protein and nucleic acid signatures, possibly reflecting immune activation and tissue repair processes.
People with potential celiac disease showed some of the most distinct spectral patterns, suggesting that their blood chemistry contains early warning signs of disease activity even before structural damage becomes visible in the intestine.
How the New Model Compared to Existing Methods
The research team compared their hybrid dual-path deep learning model to eleven other machine learning and deep learning systems. These included commonly used methods such as support vector machines, random forests, logistic regression, and several well-known neural network structures.
The new model outperformed all of them across every major measurement. It achieved the highest accuracy, the best ability to correctly identify true cases, and the strongest discrimination between the three groups. Its accuracy rate was more than ninety-four percent, and its ability to identify potential celiac disease—typically the hardest category to classify—was significantly better than all baseline models.
Because the model can detect early-stage patterns with such sensitivity, it may help identify disease long before major tissue damage occurs.
Why This Matters for Real-World Diagnosis
Current diagnostic pathways involve multiple steps, including antibody tests, genetic testing, and intestinal biopsies. These procedures can be costly, require specialized equipment, and may not be available in all healthcare settings. In addition, biopsies require time, skilled specialists, and patient cooperation, which can be difficult in children and individuals with limited access to medical care.
The approach developed in this study uses only a blood sample, relies on equipment that is more affordable and widely available than endoscopic tools or mass spectrometry systems, and produces results in less than an hour. It does not require a pathologist to interpret tissue samples, nor does it depend on the quality of biopsy material.
This makes it especially valuable for early screening, follow-up evaluations, and diagnosis in regions with limited medical resources.
What the Study Means for People With Celiac Disease
This research opens the door to a future where diagnosing celiac disease could be faster, easier, and less invasive. For people living with the condition, or those who may be at risk, the findings have several important implications:
- Earlier detection: The method may identify potential celiac disease before significant intestinal injury occurs, allowing individuals to begin treatment sooner.
- Fewer invasive procedures: Many patients may not need repeat biopsies during follow-up, reducing discomfort and cost.
- Better monitoring: A simple blood-based tool could allow doctors to track disease activity more frequently, helping ensure that a gluten-free diet is effective.
- Greater global accessibility: Healthcare systems with limited resources may be able to perform rapid screening at a much lower cost.
Overall, this study demonstrates that infrared spectroscopy combined with deep learning has the potential to transform how celiac disease is detected and managed. By capturing hidden molecular signals in the blood, this technique may provide a powerful new way to support diagnosis, guide treatment, and improve long-term outcomes for people with celiac disease and those who are beginning to show early signs of it.
Read more at: nature.com









Recommended Comments
There are no comments to display.
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now