Celiac.com 06/21/2017 - Circulating gluten-specific FOXP3+CD39+ regulatory T cells have impaired suppressive function in patients with celiac disease. What does that mean?
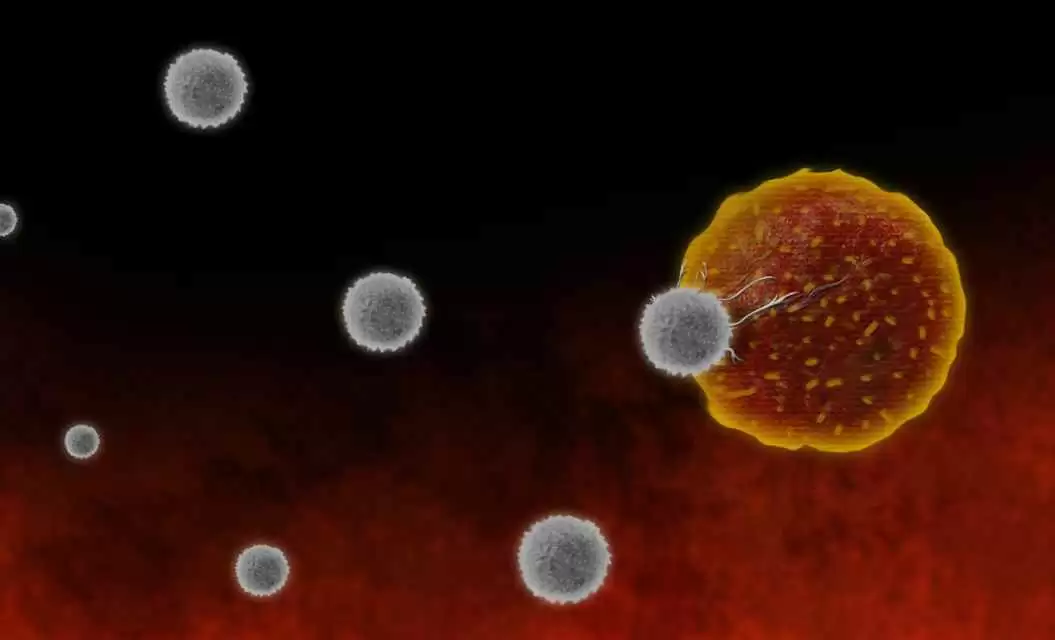
Although researchers understand the effector T-cell response in patients with celiac disease pretty well, they really don't know very much about the role played by regulatory T cells (Treg cells) in the loss of tolerance to gluten. To get a better picture, a team of researchers recently set out to define whether patients with celiac disease have a dysfunction or lack of gluten-specific forkhead box protein 3 (FOXP3)+ Treg cells.
Celiac.com Sponsor (A12):
The research team included L Cook, CML Munier, N3 Seddiki, D van Bockel, N Ontiveros, MY Hardy, JK Gillies, MK Levings, HH Reid, J Petersen, J Rossjohn, RP Anderson, JJ Zaunders, JA Tye-Din, AD Kelleher.
For the study, gluten-free patients with celiac disease underwent oral wheat challenge to stimulate recirculation of gluten-specific T cells. The research team collected peripheral blood before and after challenge. To effectively measure the gluten-specific CD4+ T-cell response, they combined traditional IFN-γ ELISpot with a test for antigen-specific CD4+ T cells that does not rely on tetramers, antigen-stimulated cytokine production, or proliferation, but relies instead on antigen-induced co-expression of CD25 and OX40 (CD134).
During the gluten challenge, levels of circulating gluten-specific Treg cells and effector T cells both rose sharply, peaking on the sixth day.
The team recounts surprise on discovering that about 80% of the ex vivo circulating gluten-specific CD4+ T cells were FOXP3+CD39+Treg cells, which reside within the pool of memory CD4+CD25+CD127lowCD45RO+ Treg cells. Even though they saw normal suppressive function in peripheral polyclonal Treg cells from celiac patients, after a short in vitro expansion, the gluten-specific FOXP3+CD39+ Treg cells showed sharply reduced suppressive function compared with polyclonal Treg cells.
The team's study offers the first estimates of FOXP3+CD39+ Treg cell frequency within circulating gluten-specific CD4+ T cells after oral gluten challenge of celiac patients.
FOXP3+CD39+ Treg cells made up the majority of all circulating gluten-specific CD4+ T cells, but they showed reduced suppressive function, indicating that Treg cell dysfunction might be a key factor in celiac disease development.
This type of research is crucial to help document the genetic physiology of celiac disease, which will help researchers to better understand and treat the disease itself.
Source:
-
J Allergy Clin Immunol. 2017 Mar 8. pii: S0091-6749(17)30343-3. doi: 10.1016/j.jaci.2017.02.015.
The researchers are variously affiliated with the Immunovirology and Pathogenesis Program, The Kirby Institute, UNSW Sydney, Sydney, Australia, St Vincent's Centre for Applied Medical Research, St Vincent's Hospital, Sydney, Australia; the Infection and Immunity Program, The Department of Biochemistry and Molecular Biology, Biomedicine Discovery Institute, Monash University, Clayton, Australia; Australian Research Council Centre of Excellence in Advanced Molecular Imaging, Monash University, Clayton, Australia; the Immunovirology and Pathogenesis Program, The Kirby Institute, UNSW Sydney, Sydney, Australia; St Vincent's Centre for Applied Medical Research, St Vincent's Hospital, Sydney, Australia, Immunology Division, Walter and Eliza Hall Institute, Parkville, Australia; Department of Medical Biology, University of Melbourne, Parkville, Australia; Department of Surgery, University of British Columbia, Vancouver, British Columbia, Canada; the Institute of Infection and Immunity, Cardiff University School of Medicine, Heath Park, Cardiff, United Kingdom; the Immunology Division, Walter and Eliza Hall Institute, Parkville, Australia; Department of Medical Biology, University of Melbourne, Parkville, Australia; ImmusanT, Cambridge, Massachusetts; and the Department of Gastroenterology, Royal Melbourne Hospital, Parkville, Australia.



.webp.c53b640f544ac5b6827ea9b8bf621ae6.webp)


Recommended Comments
There are no comments to display.
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now