
Celiac.com 05/27/2022 - Among the many symptoms associated with celiac disease, some of the commonest fall into the broad category of “dyspepsia”. These are symptoms more usually attributed to acid reflux from the stomach into the esophagus (heartburn, regurgitation, even difficulty swallowing a.k.a. dysphagia) or to peptic ulcer disease (upper abdominal pain, indigestion, fullness). While we are not entirely sure why celiac disease causes these, often in the absence of typical “bowel” symptoms, we do know how(1) . Studies of the upper gut in celiac disease patients frequently show abnormal motility and peristalsis: the conveyor belt isn’t working properly (The constipation that is often paradoxically a symptom of celiac disease probably has the same basis).
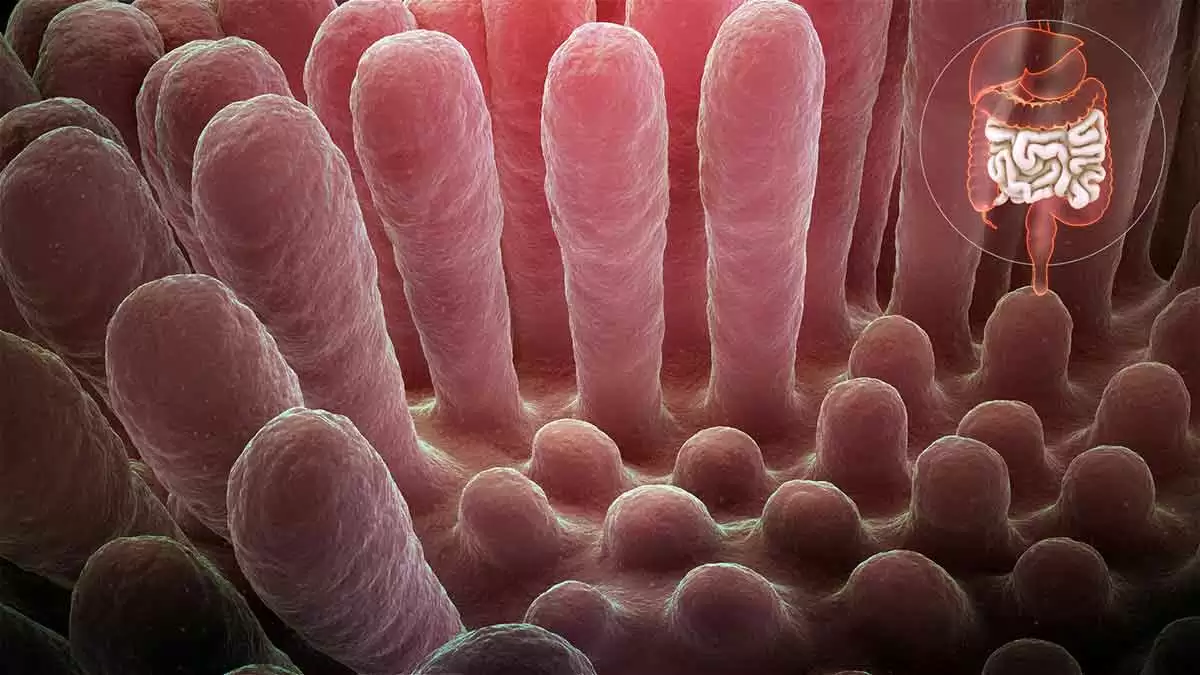
So many celiac patients are going to be referred not for small bowel investigation but for upper GI endoscopy, and the gastroenterologist is expecting not celiac disease, but reflux esophagitis, hiatus hernia, gastritis or peptic ulcer disease. Wouldn’t it be nice—and wouldn’t it make life a lot simpler for the so far undiagnosed celiac patient—if the gastroenterologist could spot villous atrophy like these other conditions?
Celiac.com Sponsor (A12):
The good news is that you can see villous atrophy down an endoscope. Well, some of the time (but more of that later). One of the most exciting developments in my career as a celiac diagnostician was when our museum piece fiberoptic endoscopes were replaced by full color videoscopes. Endoscopy was no longer an uncomfortable (for the endoscopist!) and hurried foray into the upper gut, hunched over with one eye peering down a clouded eyepiece, frantically trying to see everything and get the heck out before the disinfectant fumes wafting up the scope dissolved the glue holding my spectacles together. Instead it became a civilized stroll which ended in a duodenum filling a ten inch TV picture in glorious color. And it became clear to me and many other celiac specialists that the duodenums of celiac patients didn’t look quite right when they were up close and magnified in this way.
Abnormalities seen in our patients with villous atrophy(2) include mosaic mucosa (53%), scalloped folds (50%), fold loss (15%) and nodular mucosa (6%) and erosions (small ulcers) in the second part of duodenum in 7%. Occasionally the mucosa is so thin that blood vessels can be seen through it. Although uncommon in celiac disease, the finding of erosions in the second part of duodenum is of particular interest as clinicians may simply flag it up as peptic ulcer disease, even though peptic ulcers usually only affect the first part of duodenum. I’ve seen a few patients who had previously been wrongly diagnosed “peptic” because of this endoscopic feature.
So how have these endoscopic markers changed my practice? Around half of my new celiac patients present with dyspepsia and are recognized at endoscopy(3) . One in 60 (twice the background prevalence of celiac disease) patients referred for endoscopy from primary care with dyspepsia are diagnosed celiac because of these markers(4). Often the story is of dyspeptic symptoms which have not responded to ulcer healing drugs—while on a gluten-free diet they disappear magically.
There are two caveats regarding endoscopic markers. While villous atrophy in adults is pretty much synonymous with celiac disease in Western Europe, elsewhere it may sometimes indicate other disease, as reported by the New York Group(5) . Secondly, the bad news is that villous atrophy can’t always be spotted. We found that only 74% of villous atrophy cases had endoscopic markers(2) , and as many patients had endoscopy for biopsy because we were expecting to find celiac disease, that figure may be an overestimate of routine practice. The Mayo Clinic found markers in only 59% of celiac patients from a group of anemic patients having endoscopy(6). While 82% of our patients with subtotal or total villous atrophy had one or more endoscopic markers, the yield fell to 58% for partial villous atrophy(7). And as you might expect, I have never seen endoscopic markers in gluten-sensitive patients with milder (Marsh I, Marsh II) histologic abnormalities which have not yet progressed to villous atrophy.
So lack of markers does not mean that there is no need to biopsy, particularly in high risk groups like patients with anemia and insulin dependent diabetes. In an ideal world, duodenal biopsy would be a routine part of every upper GI endoscopy, as already proposed by Peter Green and Joe Murray(8). In practice, particularly in the good ol’ underfunded UK National Health Service that I work for, this would have very significant resource implications. I suspect such a policy—duodenal biopsies taken at every endoscopy— implemented without a major funding initiative on my side of the Atlantic might find our already overworked and undervalued histopathologists under the cars of gastroenterologists furiously cutting through their brake lines.
In the meantime, and until the New Jerusalem of routine duodenal biopsy during endoscopy is constructed, recognition of the endoscopic markers of celiac disease, while not foolproof, represents a pragmatic way of diagnosing celiac patients who present with dyspepsia.
References:
- Bassotti G, Castellucci G, Betti C et al. Abnormal gastrointestinal motility in patients with celiac sprue. Dig Dis Sci 1994; 39: 1947-54.
- Dickey W, Hughes DF. Erosions of the second part of duodenum in patients with villous atrophy. Gastrointestinal Endoscopy 2004; 59: 116-118.
- Dickey W. Diagnosis of coeliac disease at open access endoscopy. Scandinavian Journal of Gastroenterology 1998; 33: 612- 5.
- Dickey W, Hughes DF. Prevalence of celiac disease and its endoscopic markers among patients undergoing routine endoscopy. American Journal of Gastroenterology: 1999; 94: 2182-6.
- Shah VH, Rotterdam H, Kotler DP, Fasano A, Green PHR. All that scallops is not celiac disease. Gastrointest Endosc 2000; 51: 717-20.
- Oxentenko AS, Grisolano SW, Murray JA et al. The insensitivity of endoscopic markers in celiac disease. Am J Gastroenterol 2002; 97: 933-8.
- Dickey W, Hughes DF. Disappointing sensitivity of endoscopic markers for villous atrophy in a high-risk population: implications for celiac disease diagnosis during routine endoscopy. Am J Gastroenterol 2001; 96: 2126-8.
- Green PHR, Murray JA. Routine duodenal biopsies to exclude celiac disease? Am J Gastroenterol 2003; 58: 92-5.






Recommended Comments
There are no comments to display.
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now