In the commercial supplement product, Glisodin, the properties of gliadin have, in fact, already been used for the last few years to facilitate the delivery of the antioxidant enzyme superoxide dismutase (SOD) protecting it from digestive acids and getting it through the intestinal mucosa, probably taking advantage of the zonulin effect. Aware of celiac disease, the developer of Glisodin tried to use other peptides as a carrier of SOD, but the only gliadin was effective. Unfortunately, this denies celiacs the benefit of using Glisodin to treat oxidative stress.
Celiac.com Sponsor (A12):
Abstract of Study:


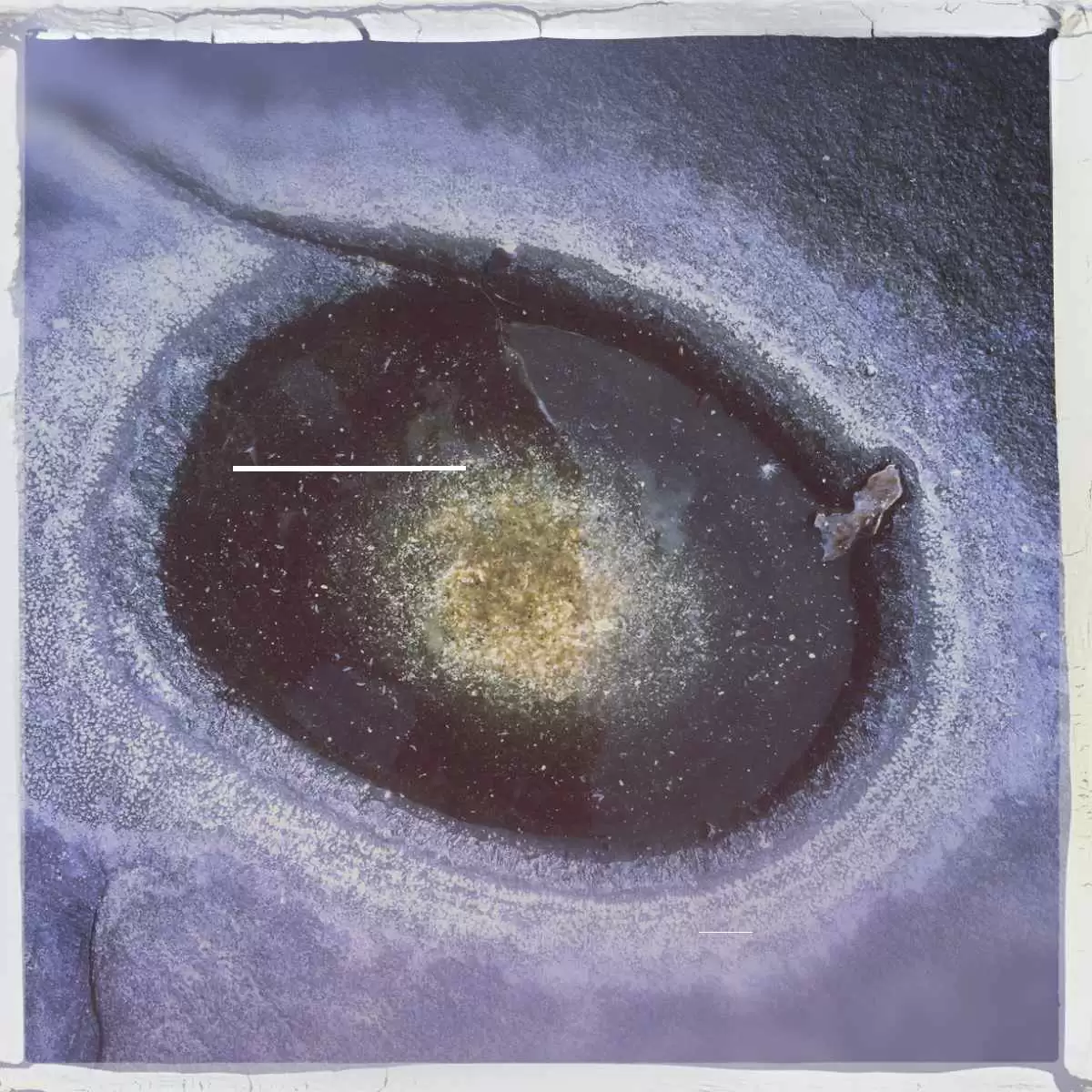

.webp.9b05843efc652dc02f0ed05391ce22ea.webp)




Recommended Comments