Celiac.com 04/20/2016 - I am likely to be accused of gluten heresy. That is because I propose that celiac disease and gluten sensitivity usually coexist. By this I mean that they are not mutually exclusive entities.
 In other words, most people who have celiac disease are also gluten-sensitive. Many people who are gluten-sensitive are likely to develop celiac disease with continued gluten exposure (depending on their genetic markers).
In other words, most people who have celiac disease are also gluten-sensitive. Many people who are gluten-sensitive are likely to develop celiac disease with continued gluten exposure (depending on their genetic markers).
Celiac.com Sponsor (A12):
My observations show that the distinction between celiac disease and gluten-sensitivity (the gluten syndrome) is blurred. The purpose of published algorithms and decision trees are designed to separate out celiac disease from other gluten-illnesses. I suggest that this thinking is flawed.
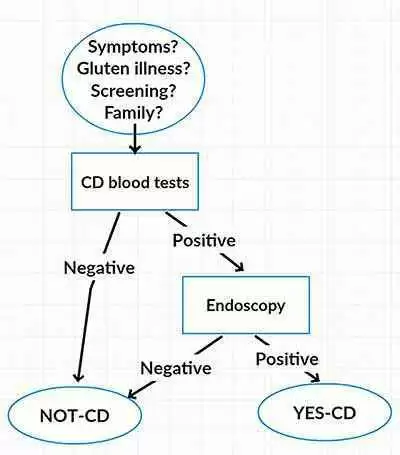
For example, most flow charts go something like this: (See Flow Chart 1 at left).
People are selected for celiac-blood-tests for a number of reasons. If your blood tests are positive (and usually if you carry a DQ2/8 gene), then you get an endoscopy to confirm/deny the diagnosis. This allows you to be categorized either Yes-celiac disease or Not-celiac disease. There is no overlap. This is an "us-and-them" scenario.
However, isolating YES-celiac disease from every other gluten problem does not take into account that people who have gluten-gut-damage may well have other manifestations of gluten-related disorders.
Such simplistic algorithms (decision trees) strike problems at every decision point. Such as: Who should be tested? Who should be re-tested? When should these tests be done? At what age? On how much gluten? What tests should be done? What are the cut-off levels? How important is carrying the DQ2/8 genes? What about sero-negative celiac disease? How accurate are endoscopic biopsies? Who interprets the Marsh scale? How long should a gluten challenge be?
Such simplistic algorithms (decision trees) also do not give satisfactory answers to the following questions:
- Why do 10% of people with celiac disease have little or no symptoms, despite having severe small bowel damage (villous atrophy)? This group is called "asymptomatic" celiac disease. Villous atrophy alone cannot account for the majority of gluten-related symptoms.
- Why do half of the people with celiac disease have autonomic nervous system dysfunction? This is the disturbance of the automatic nerve activity of your internal organs. This cannot be directly attributed to villous atrophy.
- Why do most people with celiac disease have some brain/mental upset, including the pervasive brain-fog? Many people have neurological disease from gluten but do not have established celiac disease.
- How can so many "extra-intestinal manifestations" of celiac disease be attributed to intestinal gut damage alone?
I am sure that you will have witnessed strong feelings from the defenders of 'celiac-disease-is-a-stand-alone illness'. For instance, read these two opposing comments from Facebook:
- A. "I find it hard to believe that gluten intolerant people (or gluten avoiders) are as strict as us who have celiac disease."
- B. "I am gluten intolerant (suspected Celiac but I refuse to eat gluten in order to be tested properly) … I am incredibly strict on what I eat."
The world of gluten is not black and white! But there remains a tension between those who have "biopsy-proven" celiac disease, and those people who are "gluten-intolerant". However, there is a cross-over between gluten-sensitivity/intolerance and celiac disease. There is no sharp dividing line – there is lots of grey!
I would like to see the support groups of both celiac disease and gluten sensitivity work together with a focus on their common ground. This is already happening in some countries. Both groups promote an accurate diagnosis and a strict gluten-free diet. But I call into question the accuracy of current diagnostic methodology.
Another comment from Facebook is a good example of these blurred lines:
"I had an endoscopy and I have some small intestine damage: increased intraepithelial lymphocytes, shortened villi and duodenitis. The gastroenterologist said I had gluten-sensitivity but because I was not celiac (wasn't Marsh stage 3a), he said that I didn't need to be quite as careful with gluten. But I know I am super sensitive - even a small piece of chocolate with gluten in it makes me sick for a few weeks. I suspect that I either didn't have enough gluten before the endoscopy, or I am in the early stages of developing it."
This is what I conclude:
- Both groups (people with celiac disease, and people with gluten sensitivity/intolerance) come under the umbrella category of gluten-related disorders. The term non-celiac gluten-sensitivity (NCGS) excludes those with evidence of intestinal damage from gluten. But with time and continued gluten ingestion, some of these people will develop celiac disease. NCGS is part of the gluten-related disorders spectrum (see my book: Open Original Shared Link).
- Both groups have an identical list of possible symptoms. They are both equally harmed by gluten. They are indistinguishable from each other without blood tests and/or endoscopy.
- For both groups, my recommendation is to be zero gluten. Avoidance of cross-contamination is crucial for everyone. Both groups can be exquisitely sensitive to gluten. Some celiacs experience no symptoms from gluten, making it more of a challenge for them to remain gluten-zero. Some gluten-sensitive people do not yet have overt symptoms but are developing an inflammatory state.
- Many people who are gluten-sensitive produce antibodies to gluten, AGA (anti-gliadin-antibodies). There is a large literature on this. AGA-positive people are more likely to develop gluten-illnesses. AGA tests are recommended in the Fasano paper the "spectrum of gluten related disorders", for the celiac and gluten sensitivity work-up (particularly for neurological disorders). I use them on a day-to-day basis in my Clinic, and so do many other practitioners. More wheat/gluten harmful proteins have yet to be identified. Early in the development of celiac disease, the person can have significant symptoms, and they may have elevated AGA antibodies, but they may have no evidence yet of intestinal damage. At this stage these two conditions are indistinguishable.
- How early can you diagnose celiac disease? Do you have to wait until there is substantial intestinal damage so that you can make the classic diagnosis with villous atrophy? Or do you keep on eating gluten until the damage has occurred? Or do you go strictly gluten zero and not know if you are gluten sensitive or have early celiac disease? The HLA gene (DQ2/DQ8) cannot be used as a casting vote. It is my recommendation to abandon gluten as early as possible and not wait until you have substantial intestinal damage, which may never heal.
- Not only is the gluten intolerant community (this includes celiac disease) confused about gluten-illness. Also, the medical fraternity is confused. The science and clinical issues are rapidly developing whilst most medical practitioners are still looking for the classic celiac with weight loss, malabsorption, and a bloated tummy (and are using an out-of-date simplistic algorithm). Many people request celiac tests of their GPs but are denied the test. The community is much more aware of gluten related disorder than medical practitioners.
Yes, there are a lot of issues to think about. These gluten-illnesses are complicated to diagnose. My prediction is that increasing numbers of people will adopt a gluten zero diet. However, almost certainly it is much more than the substance gluten that is making us sick. It will take a long time to unravel all of these strings. Most people are after an easy answer, or a drug, or a vaccine. But I'm sure that it is going to become even more complicated as we learn more. These complexities do not show up in a simplistic algorithm.
The way for an individual to solve this is to adopt a gluten-zero diet, lifelong.







Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now