Celiac.com 12/22/2025 - Do teenagers who already live with an autoimmune condition face a higher chance of developing type one diabetes later in life? While doctors have long noticed that autoimmune disorders tend to cluster together, most earlier research focused only on people who already had type one diabetes. A recent study reverses that perspective by looking at teenagers who began with conditions such as thyroid disease or celiac disease and then following them into adulthood to see who later developed type one diabetes.
Because type one diabetes is a lifelong condition that often begins unexpectedly, learning more about early risk factors can help improve monitoring, early detection, and long-term care. The researchers used a uniquely large group of Israeli teenagers who went through a medical screening process required before military service, which gave them access to detailed health information.
How the Study Was Conducted
Celiac.com Sponsor (A12):
The study examined more than one million four hundred thousand teenagers between the ages of sixteen and nineteen. None of them had any signs of abnormal blood sugar at the beginning. The researchers separated them into two groups. The first group included those who had no autoimmune disease. The second group consisted of individuals who already lived with at least one autoimmune condition. These included autoimmune thyroid disease and celiac disease, which were the two most common, but also other diagnosed immune-related conditions.
After placing the teenagers into these two groups, the researchers followed their medical records for up to twenty years. They relied on national diabetes registry data to determine who later developed type one diabetes as adults. Because this registry tracks new, confirmed diagnoses, including tests that show the presence of diabetes-related antibodies, it allowed the researchers to identify true new cases.
The methods used in the study allowed the researchers to adjust for important background factors such as birth year, sex, and socioeconomic indicators. This means the results better reflect the true influence of autoimmune diseases rather than unrelated lifestyle or demographic differences.
What the Study Found
Out of the entire group, a little under three percent had an autoimmune condition at the start. This included more than ten thousand with autoimmune thyroid disease and more than nine thousand with celiac disease. Over the combined follow-up period, which totaled more than fifteen million person-years, several hundred people developed type one diabetes.
People who began the study with an autoimmune disorder were far more likely to develop type one diabetes in adulthood. Their rate of developing the condition was roughly double that of their peers who had no autoimmune disease. When statistical adjustments were made to account for differences between the groups, the increased risk still remained strong.
The greatest increase in risk occurred among those with autoimmune thyroid disease. This group had nearly four times the likelihood of developing type one diabetes compared to teens without autoimmune disease. Those with celiac disease also had an elevated risk, nearly triple that of those with no autoimmune condition.
Importantly, the pattern held even when the definition of type one diabetes required confirmation by antibody testing, meaning the cases were genuine immune-driven diabetes. This strengthens the reliability of the findings.

Why These Findings Matter
Autoimmune disorders occur when the body's defense system mistakenly attacks its own tissues. Once a person has one autoimmune condition, it becomes more likely for the immune system to become misdirected toward another part of the body. This study shows that this pattern is not only theoretical—it has real implications for long-term health.
For thyroid disease and celiac disease, the results suggest that these conditions may act as early indicators of a heightened immune vulnerability that could eventually manifest as type one diabetes. Doctors caring for teens with these conditions may consider closer monitoring for symptoms related to abnormal blood sugar as these individuals approach adulthood.
Early identification of diabetes is important because it can prevent life-threatening complications at diagnosis and can allow earlier interventions that might preserve remaining insulin-producing cells.
What This Means for People with Celiac Disease
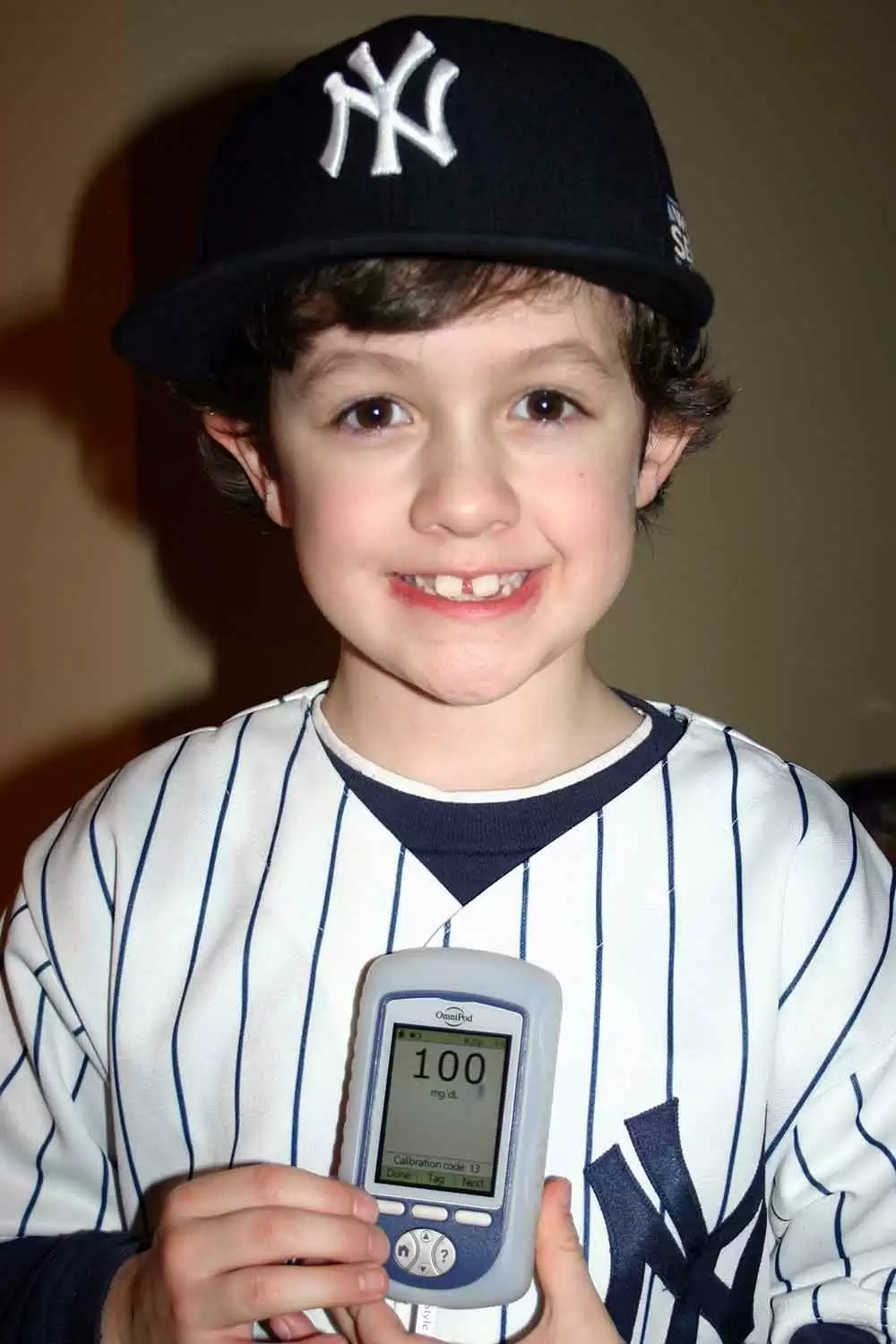
For individuals living with celiac disease—and for parents of children with celiac disease—this study carries meaningful insights. The findings show that celiac disease is not only a digestive condition but part of a broader immune pattern that may raise the likelihood of other related conditions later in life.
Although the increased risk does not mean that every person with celiac disease will develop type one diabetes, it does highlight the importance of regular checkups, awareness of symptoms such as unusual thirst or unexplained weight loss, and ongoing communication with healthcare providers.
The study also reinforces the value of proper management of celiac disease. Staying on a strict gluten-free diet helps reduce ongoing immune activity in the body. While this study does not directly evaluate whether diet lowers future diabetes risk, reducing chronic inflammation may be helpful in overall health.
Conclusion
This large and long-running study provides strong evidence that teenagers with autoimmune thyroid disease, celiac disease, or other immune disorders are more likely to develop type one diabetes as adults compared with their peers who do not have autoimmune conditions. The research highlights how interconnected autoimmune diseases can be, and why early recognition of one may prompt careful observation for others.
For people with celiac disease, the findings can help guide informed discussions with doctors about long-term health. Understanding that celiac disease may indicate a higher susceptibility to type one diabetes empowers individuals and families to seek appropriate monitoring, respond early to possible symptoms, and maintain consistent follow-up care. Ultimately, awareness is a powerful tool that can support better outcomes and long-term well-being.
Read more at: diabetesjournals.org











Recommended Comments
There are no comments to display.
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now