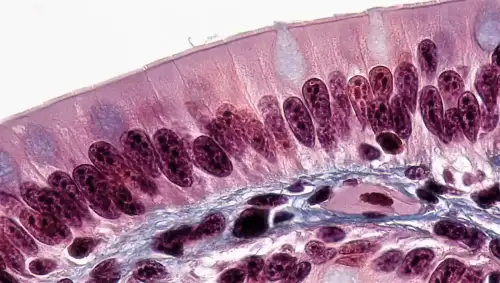
Celiac.com 10/06/2025 - Celiac disease is an autoimmune disorder that affects roughly half a percent to one percent of people worldwide. It is triggered by gluten, a protein found in wheat, barley, and rye. When gluten is consumed, the immune system attacks the small intestine, causing inflammation and damage. This study used advanced single-cell analysis to create the most detailed map so far of how cells in the small intestine differ between people with active celiac disease and healthy individuals.
Purpose of the Study
The researchers aimed to understand how immune cells, supporting stromal cells, and the intestinal lining interact with each other in celiac disease. By examining more than 200,000 individual cells, they identified specific changes in cell numbers, activity, and communication. This approach sheds light on how immune signals reshape the intestinal environment, leading to the characteristic tissue damage of celiac disease.
Key Cellular Changes
Celiac.com Sponsor (A12):
Several important differences emerged between healthy tissue and celiac tissue:
- Epithelial changes: The lining of the intestine showed an increase in immature stem-like cells and secretory cells, while the normal absorptive cells were reduced. This reflects the known pattern of villus atrophy (loss of finger-like projections) and crypt hyperplasia (expansion of the cell-producing areas).
- Immune cell changes: Specific types of T cells were more common, especially those producing strong inflammatory signals like interferon gamma. B cells and myeloid cells also showed higher activity, releasing a wide range of pro-inflammatory molecules.
- Stromal changes: Stromal cells, especially fibroblasts that normally support tissue structure and regeneration, were increased and highly active. Subsets of fibroblasts producing signals such as NRG1 and SMOC2 were particularly enriched.
How Immune Signals Affect Tissue
The study revealed how immune activity drives communication between different cell types. Immune cells release key molecules such as interleukin-1 beta and interferon gamma. These molecules activate fibroblasts, which in turn send signals that encourage stem-like intestinal cells to expand. While this might be an attempt at tissue repair, it also reduces the number of mature absorptive cells, worsening the nutrient absorption problems seen in celiac disease. In this way, the immune system, stromal cells, and epithelial cells form a cycle of inflammation and maladaptive tissue remodeling.
Novel Findings About Fibroblasts
Fibroblasts, long considered just structural support cells, were shown to play an active role in celiac disease. The study found that fibroblast subtypes producing NRG1 and SMOC2 were increased in diseased tissue. These molecules influence how intestinal cells grow and mature, potentially explaining the excess of stem-like cells and secretory cells. This suggests that fibroblasts are not passive bystanders but key players in shaping the tissue environment in response to gluten-triggered immune activity.
Communication Between Cell Types
The research highlighted extensive communication between immune cells, myeloid cells, fibroblasts, and the intestinal lining. The interactions were particularly strong in active celiac disease compared to healthy tissue. This reinforces the idea that celiac disease is not only an immune-driven condition but also a disorder of disrupted tissue repair and remodeling.
Clinical Implications
Current treatment for celiac disease is limited to lifelong avoidance of gluten. Despite this, many patients continue to struggle with symptoms or slow recovery. By uncovering the roles of fibroblasts and other stromal cells, this study points toward new therapeutic strategies. Targeting the communication pathways between immune cells, fibroblasts, and epithelial cells could open the door to treatments that reduce inflammation, restore healthy intestinal lining, and improve long-term outcomes.
Limitations
The researchers noted some limitations. Certain rare cell types, such as Paneth cells, were not fully captured in the analysis. There were also differences between patients in the abundance of myeloid cells. Since some samples were frozen before analysis, this may have affected recovery of sensitive cell types.
Conclusion
This study offers the most detailed picture yet of how different cell types in the small intestine interact in celiac disease. It shows that immune activity does more than trigger inflammation—it also reshapes the stromal environment and pushes intestinal cells toward an abnormal state. For people with celiac disease, these findings are significant because they provide fresh insight into why tissue damage occurs and why recovery can be slow or incomplete. In the future, treatments aimed at these new pathways may help improve quality of life beyond what is possible with a gluten-free diet alone.
Read more at: cell.com









Recommended Comments
There are no comments to display.
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now