Celiac.com 06/12/2025 - For individuals with celiac disease, eating even tiny amounts of gluten can trigger harmful immune reactions that damage the small intestine. While following a strict gluten-free diet is the only treatment, it can be very difficult to avoid accidental exposure. Gluten can hide in processed foods, be present due to cross-contamination in kitchens or food factories, or exist in trace amounts in products labeled “gluten-free.”
Currently, doctors use blood tests and symptom reports to monitor if someone with celiac disease is successfully avoiding gluten. However, these tools are not always reliable, especially for detecting small or occasional gluten exposure. This study looked at a new type of test that detects specific fragments of gluten, called gluten immunogenic peptides, that are excreted in urine and stool. These peptides are resistant to digestion and remain in the body long enough to be measured, making them good indicators of recent gluten intake.
Introducing the Gluten Immunogenic Peptide Tests
Celiac.com Sponsor (A12):
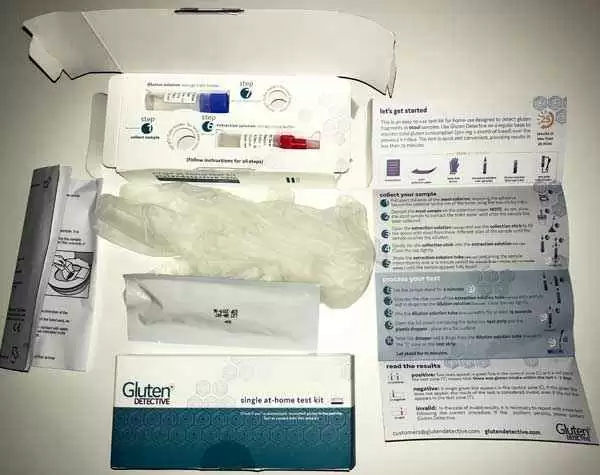
Researchers used two tests developed by the company Biomedal: iVYCHECK (a urine test) and iVYLISA (a stool test). These tests can detect whether someone has eaten gluten recently and how much gluten was consumed. The urine test is best for spotting short-term exposure, such as gluten eaten within the last day. The stool test can measure gluten exposure over several days and provides a more detailed picture.
The main goal of the study was to test how well these tools work in real-life conditions. The researchers also wanted to know if people with celiac disease would find these tests helpful in managing their diet.
How the Study Was Conducted
The study included 21 people. Sixteen participants were following a gluten-free diet, and most had a confirmed diagnosis of celiac disease. Five people without any dietary restrictions served as the control group.
Over a 9-day period, all participants were asked to keep a detailed food and symptom diary. They recorded what they ate, whether it was homemade or from a restaurant, and noted any symptoms they experienced. They also provided urine and stool samples on days 5, 7, and 9 of the study.
The tests were used to analyze these samples for gluten peptides, and the results were compared with what people reported in their food diaries.
What the Tests Found
The results showed that the stool test was highly accurate when used to confirm whether someone had consumed gluten. It correctly identified gluten in 97% of the people who ate it and had a strong ability to rule out gluten intake when it wasn’t present (a high “negative predictive value”).
The urine test was even more sensitive—it caught every instance of gluten exposure reported during the study. However, it was not as specific. This means that while it picked up all known exposures, it also occasionally showed positive results even when people claimed not to have eaten gluten, possibly due to hidden gluten in foods or limitations in self-reporting.
One participant who believed they were following a gluten-free diet recorded symptoms in their diary and later discovered high levels of gluten in their stool sample. This incident demonstrated how these tests could uncover accidental gluten exposure that might otherwise go unnoticed.
Interestingly, over half of the people on gluten-free diets showed some level of gluten peptide in their samples. This raises questions about how much gluten is sneaking into “gluten-free” meals or if some positive results could be false positives. More detailed studies would be needed to confirm this.
How Well Did People Accept the Tests?
Most participants were enthusiastic about using these tests. Many saw them as a valuable tool to monitor accidental gluten intake. People were especially interested in using the tests to understand whether small amounts of gluten were slipping into their diet, often without them knowing.
However, not everyone found the tests equally acceptable. Most people preferred the urine test over the stool test, likely due to the convenience of sample collection. The need to keep a food diary for nine days and provide multiple samples may have affected how willing some people were to fully participate.
The researchers noted that parents of children with celiac disease might be especially interested in these tools, as it can be difficult to monitor a child’s food intake at school or social events.
Limitations of the Study
This study relied heavily on self-reported food diaries rather than independent confirmation of what people ate. This makes it harder to say for sure whether some positive test results were due to actual gluten intake or possible test errors.
Additionally, the study did not include blood tests or intestinal biopsies, which are other ways to assess the impact of gluten exposure in people with celiac disease. Including those could have helped determine whether low levels of gluten peptides actually cause harm.
Still, the study offers promising evidence that these tests could be helpful in real-world settings. They may offer more detailed and timely feedback for people trying to avoid gluten and provide doctors with another tool to assess diet adherence.
Why This Matters for People with Celiac Disease
For people with celiac disease, knowing whether gluten is sneaking into their diet is incredibly important. Ongoing gluten exposure, even in small amounts, can cause gut damage, nutritional deficiencies, and other serious health problems.
These new tests may give individuals a clearer picture of their gluten exposure. A negative test result could offer peace of mind, especially when symptoms are unclear or blood tests are inconclusive. Meanwhile, a positive result may alert someone to hidden sources of gluten and encourage stricter avoidance.
As the tests become more available and affordable, they could become an important part of managing celiac disease. They may also help identify accidental exposures before they cause lasting harm. However, further research is needed to determine how often they should be used and how best to interpret low-level detections.
Conclusion
This study shows that measuring gluten peptides in urine and stool is a promising way to detect hidden or accidental gluten exposure in people following a gluten-free diet. These tests are especially useful when symptoms or blood tests are unclear. While more research is needed, these tools may soon become a helpful addition to the standard approach for monitoring celiac disease and helping patients maintain a truly gluten-free lifestyle.
Read more at: onlinelibrary.wiley.com










Recommended Comments
There are no comments to display.
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now