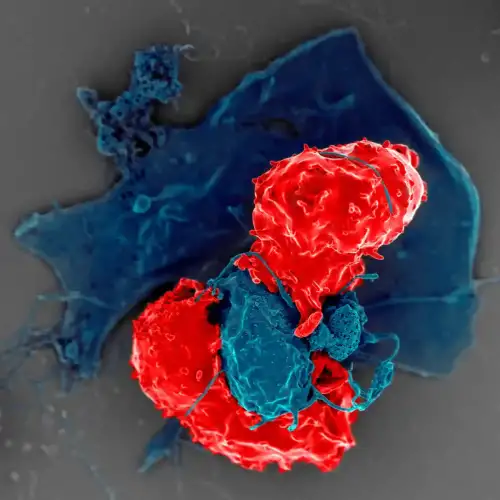
Celiac.com 10/09/2024 - Celiac disease is an autoimmune disorder where the ingestion of gluten, a protein found in wheat, barley, and rye, triggers an immune response that damages the small intestine's lining. This condition has been extensively studied, but the specific interactions between gluten, the immune system, and the cells lining the gut, known as intestinal epithelial cells, are still being explored. A recent study has provided new insights into how these cells contribute to the immune response in celiac disease, particularly through their role in activating specific immune cells known as CD4+ T cells.
The Study's Approach: Examining Gut Cells in a New Light
The researchers focused on the interactions between intestinal epithelial cells and CD4+ T cells, which are a type of immune cell that plays a central role in the immune response to gluten. To do this, they used a combination of human tissue samples and genetically modified mice that carried human genes associated with celiac disease, specifically the HLA-DQ2.5 gene, which is crucial for gluten recognition by the immune system.
Celiac.com Sponsor (A12):
The team created organoid models, which are miniature, functional versions of the gut created from mouse intestinal cells. These organoids were exposed to various inflammatory triggers, as well as to both whole and predigested forms of gluten. By using these models, the researchers could closely observe how the cells in the gut lining interacted with gluten and how these interactions affected the immune response.
Key Findings: Intestinal Cells as Active Participants in Immune Response
The study found that intestinal epithelial cells are not just passive victims of immune attack in celiac disease. Instead, these cells actively participate in the immune response by presenting gluten antigens to CD4+ T cells. This presentation is crucial because it triggers the activation of these T cells, which then orchestrate the body's immune response against gluten.
The researchers observed that when the gut cells expressed a specific molecule called major histocompatibility complex class II (MHCII), they could present gluten antigens more effectively to CD4+ T cells. This process was further enhanced when the cells were exposed to a protein called interferon-gamma, which is associated with inflammation. As a result, the CD4+ T cells became more active, proliferated rapidly, and released inflammatory substances like interleukin-2, interferon-gamma, and interleukin-15, which are known to play a role in the damage to the gut lining seen in celiac disease.
The Role of Gut Bacteria: A Surprising Twist
Another intriguing aspect of the study was the role of gut bacteria in modulating the immune response. The researchers found that when gluten was predigested by a specific enzyme produced by the bacterium Pseudomonas aeruginosa, the activation of CD4+ T cells was even more pronounced. This suggests that certain bacteria in the gut could influence how the immune system reacts to gluten, potentially worsening the effects of celiac disease.
Implications of the Study: New Avenues for Treatment
This study sheds light on the complex interactions between gut cells, the immune system, and gluten in celiac disease. By revealing that intestinal epithelial cells are active participants in the immune response, the research opens up new possibilities for treatment. Therapies that target these cells could potentially modulate the immune response, offering a novel approach to managing celiac disease.
For those living with celiac disease, this study provides a deeper understanding of how their condition develops at a cellular level. It also underscores the importance of gut health and the potential role of gut bacteria in influencing disease outcomes. As research continues, these findings could lead to more effective treatments that go beyond simply avoiding gluten, offering hope for improved quality of life for those affected by this challenging condition.
Read more at: gastrojournal.org








Recommended Comments
There are no comments to display.
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now