Celiac.com 05/22/2025 - Celiac disease is an autoimmune disorder in which the immune system mistakenly attacks the lining of the small intestine when gluten—a protein found in wheat, barley, and rye—is consumed. This reaction leads to inflammation, damage to intestinal tissue, and impaired nutrient absorption. While genetics play a significant role in celiac disease, the exact mechanisms by which certain genes contribute to the condition remain unclear.
This study focuses on the HLA-DQA1 gene, a critical player in celiac disease susceptibility. By examining how specific variants of this gene influence immune responses to gluten, researchers hope to uncover new insights into disease development. The study also proposes experiments using genetically modified mice to explore how different HLA-DQA1 variants affect immune reactions and intestinal damage.
Celiac Disease vs. Gluten Sensitivity
Celiac.com Sponsor (A12):
Celiac disease is often confused with gluten sensitivity, but they are distinct conditions.
- Celiac Disease: An autoimmune disorder where gluten triggers an immune response that damages the small intestine. This can lead to malnutrition, digestive issues, and long-term health complications.
- Non-Celiac Gluten Sensitivity (NCGS): A less severe condition where gluten causes symptoms like bloating and stomach pain but does not cause intestinal damage.
The study emphasizes celiac disease due to its severe health consequences and strong genetic links.
How Celiac Disease Develops
When someone with celiac disease eats gluten, the immune system reacts abnormally:
- Gluten Breakdown: Gluten is broken down into smaller proteins, including gliadin, which the immune system sees as a threat.
- Immune Activation: Specialized immune cells (antigen-presenting cells) present gliadin fragments to T-cells, a type of white blood cell.
- Inflammatory Response: Activated T-cells release inflammatory chemicals (cytokines) that attract more immune cells, leading to intestinal damage.
- Tissue Damage: Over time, this immune attack flattens the intestinal villi (finger-like projections that absorb nutrients), causing malabsorption and other symptoms.
A key enzyme called tissue transglutaminase (TG2) worsens this process by modifying gliadin, making it even more recognizable to the immune system.
The Genetic Link: HLA-DQA1 and Celiac Disease
The HLA-DQA1 gene is located on chromosome 6 and plays a crucial role in immune function. It helps the body distinguish between its own cells and foreign invaders. Certain variants of this gene increase the risk of celiac disease by making the immune system more reactive to gluten.
- High-Risk Variants: The HLA-DQ2 and HLA-DQ8 variants are strongly linked to celiac disease. People with these variants are more likely to develop the condition.
- Mechanism: These gene variants produce proteins that bind tightly to gluten fragments, triggering a stronger immune response.
Despite knowing that HLA-DQA1 is involved, researchers still don’t fully understand how different versions of this gene contribute to disease severity.
Proposed Experiments: Studying HLA-DQA1 in Mice
To better understand how HLA-DQA1 variants influence celiac disease, the study outlines a series of experiments using genetically modified mice:
1. Creating HLA-DQA1 Knock-In Mice
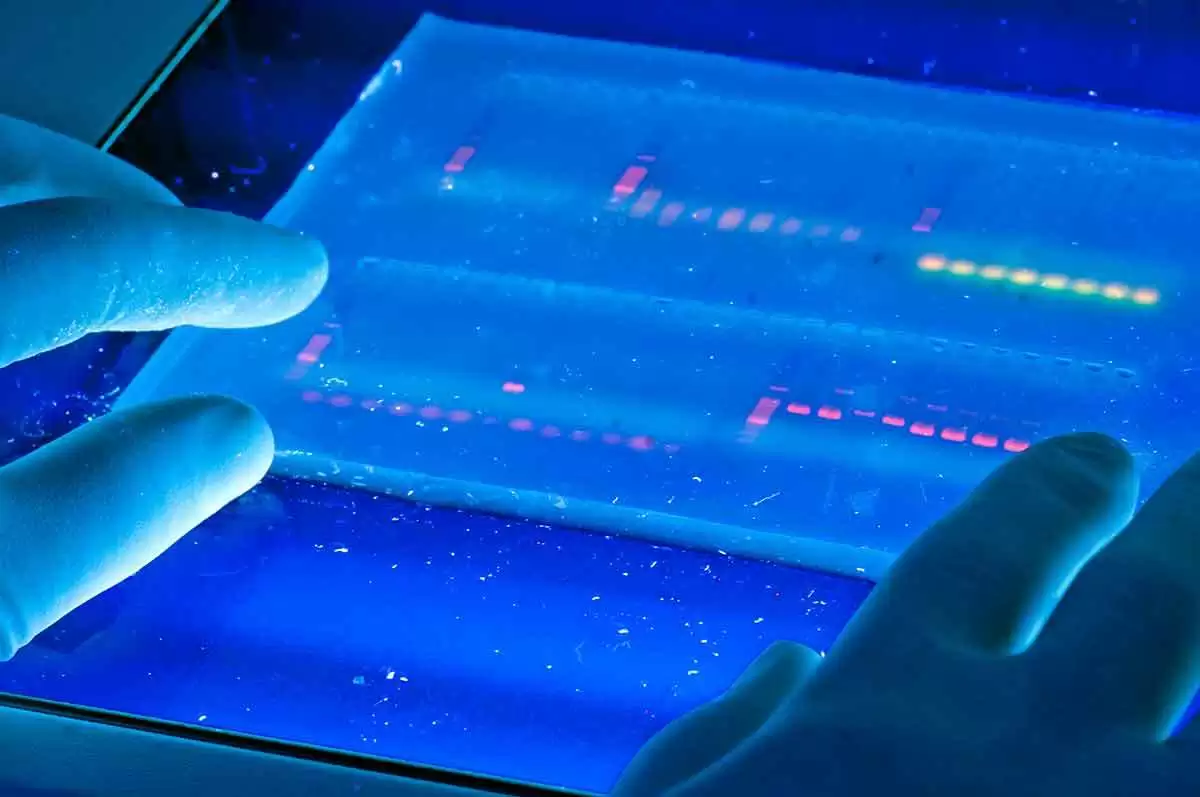
Using CRISPR/Cas9 gene editing, researchers will insert human HLA-DQA1 variants into mice. This will allow them to study how these genes affect immune responses to gluten.
2. Testing Immune Reactions
Mice will be fed a gluten-containing diet, and their immune responses will be measured by:
- T-cell activation: Checking if T-cells react to gluten.
- Cytokine production: Measuring levels of inflammatory chemicals.
- Intestinal damage: Examining tissue under a microscope to assess villi damage.
3. Comparing Different Genetic Variants
The study will compare:
- Mice with high-risk HLA-DQA1 variants (expected to show strong immune reactions).
- Mice with low-risk variants (expected to have milder reactions).
- Normal mice (as a control group).
Challenges and Future Research
While mouse studies provide valuable insights, they have limitations:
- Mice do not perfectly replicate human immune responses.
- Environmental factors (like gut bacteria) also influence celiac disease but may differ in mice.
Future research should:
- Study HLA-DQA1 variants in diverse human populations.
- Investigate how other genes and environmental factors interact with HLA-DQA1.
- Develop therapies that target specific immune pathways in celiac disease.
Why This Research Matters for People with Celiac Disease
Understanding the role of HLA-DQA1 could lead to:
- Better Diagnostic Tools: Identifying high-risk genetic variants could help predict who might develop celiac disease.
- Personalized Treatments: Therapies could be tailored based on a person’s specific genetic risk.
- New Therapies: Drugs that block harmful immune responses triggered by HLA-DQA1 could be developed.
Currently, the only treatment for celiac disease is a strict gluten-free diet. However, this research could pave the way for new treatments that address the root cause of the disease—offering hope for better management and improved quality of life for those affected.
By uncovering the genetic and immune mechanisms behind celiac disease, this study brings science one step closer to more effective solutions for patients worldwide.
Read more at: lakeforest.edu








Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now