
Celiac.com 07/09/2019 - Everyone in the Celiac community has read the press release about ImmusanT stopping the Phase 2 clinical trial of their drug Nexvax2. The drug was going to modify the immune system to ignore gluten. The hope was no more worries about cross contamination! However, in late June, ImmusanT issued a press release stating, "Nexvax2 did not provide statistically meaningful protection from gluten exposure for celiac disease patients when compared with placebo." Wait what?
Let's go back a bit and talk about my experience in the clinical trial.
I was in the Nexvax2 clinical trial. It consisted of five phases. The first phase was screening where they got all of your medical records that confirmed a celiac diagnosis and a gluten challenge. The gluten challenge was drinking a nasty gluten drink with the equivalent of 2 slices of bread and to evaluate your reaction and confirm that it was violent enough.
Celiac.com Sponsor (A12):
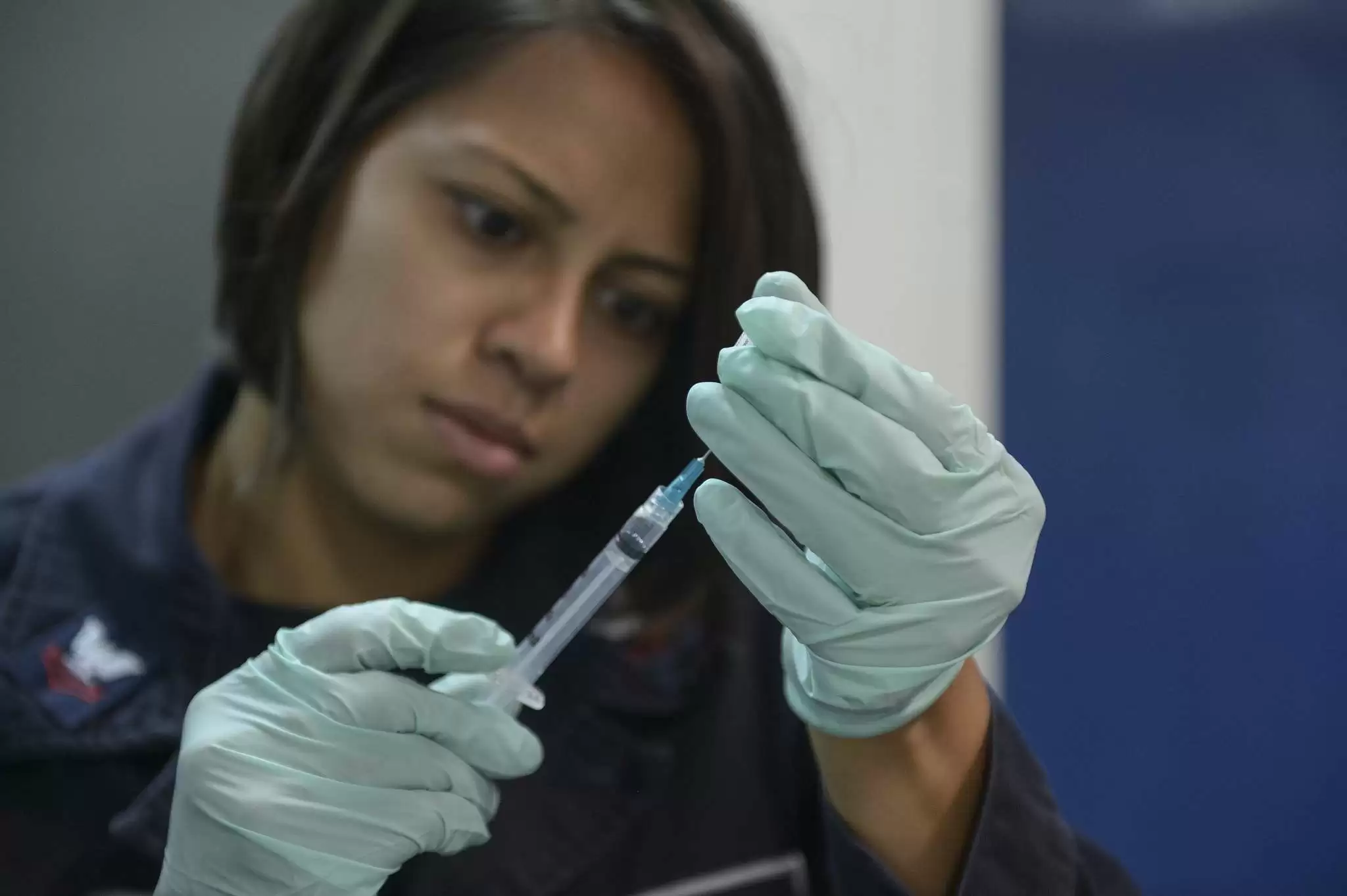
The second phase involved updosing. We had to go to the center twice a week for six weeks to receive dose increase injections of the medicine. (I'm going to refer to the test drug as medicine - I don't know if I got Nexvax2 or placebo, but it's just easier to say medicine.) During this phase, I did experience some side effects. Occasionally I would be exceptionally tired or have an upset stomach. It was not bad and nothing that couldn't be managed with a nap and acetaminophen.
The third phase was maintenance dosing. We had 10 weeks of bi-weekly self injections of the full dose of the medicine. The fourth phase was the food challenges. The fifth stage was post study testing.
Last time I wrote about my experience, I was all the way into self-injections. I was given 20 pre-filled auto-injectors. I was given a schedule and a log to note when and where I injected. All of these shots went into my stomach. My abdomen was divided into 4 quadrants at my belly button - upper right, upper left, lower right, and lower left. I rotated where the shot went into my abdomen. They didn't hurt at all. I also noted the date, time, and whether or not I received the full injection.
During this time, I never felt better. My energy levels were up. My weight was dropping without even trying. I was sleeping better. I was exercising better. I had normal bowel movements—which I haven't had in over 10 years—long, soft, well-formed just perfect. Dr. Oz would be proud. All of my celiac symptoms went away. It was like I was normal. This was a very, very good time for me.
At week 6 of the 10 maintenance doses is when the food challenges began. There were three food challenges. In the three challenges, one challenge would be gluten, one challenge would be placebo, and the third would be of their choice, either gluten or placebo. So, I could potentially get gluten twice or a placebo twice.
For the first challenge they brought out a big white box with my name on it. Inside were three smaller boxes labelled 1, 2, and 3. The smaller boxes contained a shaker bottle, water, and the powder that could be gluten or placebo. If it's gluten, it has the equivalent of two slices of bread. To start the test I had five minutes to consume the drink.
This part was mentally challenging for me. In the first phase of the study, I knew I was getting gluten. I could prepare. I knew I was going to be sick and was doing this on purpose for science. That I could handle. This time I didn't know whether I was getting gluten or not. It is mentally tough to not know what you are getting.
What happens if I react? What happens if I don't react? Does that mean this is a placebo? Does that mean I got a placebo instead of the medicine? What if I got the drug and I still react? Am I an outlier? What does that mean for the study? All of these things were going through my head as I was mentally preparing to drink the beverage. I cannot explain how challenging it was to drink that drink with the time pressure, not knowing what would happen.
The first challenge went well. No reaction. I was a little nauseous but nothing like my first trip down the gluten road. All was well. It would be two weeks until the next challenge.
Here's where things go a little sideways.
I had to go to California between the first food challenge and second food challenge to help a relative who was recovering from a stroke. I packed my study medication, got on a flight, and flew out to the West Coast. Getting the auto-injectors through security was easy with my doctor's note, as well as the frozen ice packs needed to keep the Nexvax2 cold. On my first day in California I woke up with pink eye and a terrible cold. Off to urgent care I went for medicine because I can't risk giving my relative pink eye or a cold. I got pink eye medicine and amoxicillin.
I was in California for about a week and planed to fly home the following Tuesday. I finished the antibiotic on Tuesday, and did my injection on Wednesday, per the protocol. Thursday I did the food challenge.
This second challenge did not go well.
I threw up about an hour after drinking the food challenge drink. That stunk. But I will say this. When I drank the gluten drink at the beginning of the study, I was sick for a week. On the couch with extreme exhaustion, gastrointestinal distress, and just general yuckiness. When I woke up on Friday, I didn't feel bad. I felt quite good. The change between feeling bad for a week and being able to bounce back from a glutening was glorious.
Not all that is good, can stay good. At about 2:45 that afternoon, my left ring finger became exceptionally itchy, red, and started to swell. I was on my way to pick up my kids from school and stopped to buy some Benadryl cream for my finger. As the day progressed, my finger started to swell and continued to be itchy. By 5 that night, the swelling and itchiness had spread to my palm and my right hand was beginning to itch. By 7 that night both of my hands were so swollen I couldn't make a fist. I had been drinking Benadryl like it was wine and it was not making a dent in the itch or the swelling. By 9 that night, my neck started itching. By the time I left for the Emergency Department at 11 that night, my hands were so swollen I couldn't bend my fingers and both my hands and my neck were incredibly itchy.
After a few hours in the waiting room, I saw the doctor and he said I was having an allergic reaction. He contacted the study doctors confirming that I was having an allergic reaction. They said to make sure I was safe, give me whatever medication was needed, and don't worry about the study. My health and safety came first. I was given IV Benadryl and steroids and sent home.
One of the reasons someone was not going to be able to be in the study was taking an oral steroid 6 months prior to the first injection. I was lying in the ER four injections from the end of the study realizing that my participation in the study may be over. The ER doctor did not know what could have caused the reaction and wouldn't hazard a guess, but did say that an allergic reaction to amoxicillin could start several days after stopping amoxicillin. I was told to not do any more self-injections until further notice.
After a few days, the swelling in my hands went down and returned to normal. There doesn't seem to be any long term effects from this episode.
Over the next few days, the study doctors and the people from ImmusanT talked about my case. They decided for my safety that I should be removed from the study. I felt like my rocket engine propelling me toward a cure just flamed out. But they were right. We don't know why I had a reaction and we could not risk me having another, potentially more severe reaction next time.
I had to go to the study center to return the four remaining auto-injectors, do final blood testing, and final testing for the study. It was a very sad day for me. I felt like a failure. My body failed and there was nothing I could do about it. I still feel like that study is unfinished and it makes me sad to write my story.
Reading the notice that the Nexvax2 trial was terminated early was another blow to me. It was even worse knowing how good I felt on the medicine. It was worse knowing that after the food challenge my reaction was totally different than the first gluten challenge. I believed it worked for me. I feel like I failed, not the medicine, by having an allergic reaction. So when they stopped the trial, I felt like a failure again.
Looking ahead.
I hope they look at the data and can find something good in it. I hope they are able to see that the daily journal of side effects went to almost zero when I was on the medicine compared to symptoms almost daily before starting the medicine. I hope they can retool the study to maybe not test against such a high gluten dose. I mean since when is cross contamination the gluten equivalent of 2 slices of bread? Normally, if we get glutened, it is a much smaller amount that makes us sick. Heck, the FDA says anything more than 20 parts per million causes damage, so maybe they could test against a smaller amount of gluten. I think that's where I would look if I were the ImmusanT scientists.
I also have to remember that Nexvax2 is only one of several drugs that are currently in clinical trials for celiac disease. While I hope to see Nexvax2 again, there are other drugs with real potential. I had hoped Nexvax2 was a cure, but I would be temporarily satisfied with something that allowed me not to worry about every single morsel of food I put into my mouth making me sick.
As a side note, I write a blog and talk about clinical trials all the time. I found a celiac study looking for healthy volunteers. I had several healthy parents of celiac kids asking for more information so they could volunteer to help propel the quest for a cure forward. The idea that these parents are willing to put themselves in a clinical trial in order to help their children has always demonstrated the quiet hope for a cure that I think we all feel.
I firmly believe the cure for celiac disease will be here in the next 10-15 years. I'm not sure what it may look like but I do know this—each person with celiac disease and has the ability to volunteer for a clinical trial should. It is worth the time and effort and will potentially pay big dividends in the future for all of us. Science can't advance without some of us putting our bodies on the line.
In closing, my clinical trial ended in March. I believe my body is working better today than it did before the trial and it's now July. My old celiac body is creeping in, but it still isn't as bad as it was before the trial.








Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now