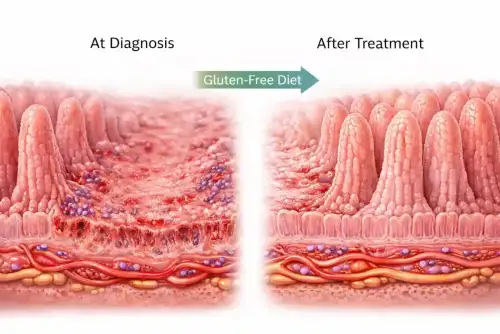
Celiac.com 02/09/2026 - Celiac disease is an immune-driven condition in which eating gluten causes damage to the lining of the small intestine. This damage interferes with nutrient absorption and can lead to a wide range of symptoms affecting both the digestive system and the rest of the body. Some people develop clear digestive complaints, while others experience symptoms such as fatigue, anemia, or bone weakness. Because the disease can look very different from person to person, diagnosis is sometimes delayed.
Doctors often pay special attention to so-called “alarm symptoms” when evaluating digestive conditions. These symptoms include unintentional weight loss, anemia, vomiting, bleeding from the digestive tract, and difficulty swallowing. In many gastrointestinal diseases, alarm symptoms can signal serious underlying problems. In people with untreated celiac disease, alarm symptoms are known to be linked to more severe intestinal damage at the time of diagnosis. What has been less clear is whether these symptoms predict worse health outcomes years later, after treatment begins.
Purpose of the Study
Celiac.com Sponsor (A12):
This study set out to answer an important question for patients and clinicians: do alarm symptoms at the time of celiac disease diagnosis lead to poorer long-term outcomes? Researchers wanted to know whether people who were sicker at diagnosis continued to struggle more with symptoms, intestinal healing, quality of life, or other health problems after many years on a gluten-free diet.
Understanding this relationship is especially important as medical practice moves toward less invasive diagnostic approaches. If alarm symptoms do not predict worse long-term outcomes, this could influence how aggressively patients are monitored after diagnosis.
How the Research Was Conducted
The study followed more than eight hundred adults with biopsy-confirmed celiac disease. All participants had been living with the diagnosis for many years and had followed a gluten-free diet for a long period of time. The average duration of treatment was close to ten years.
Researchers gathered information from medical records, interviews, blood tests, and validated questionnaires. They divided participants into two groups based on whether alarm symptoms were present at the time of diagnosis. Alarm symptoms included anemia, weight loss, vomiting, bleeding from the digestive tract, and black stools. Most people with alarm symptoms had anemia, weight loss, or both.
The study compared these two groups across many factors, including intestinal damage at diagnosis, healing of the intestine after treatment, ongoing symptoms, quality of life, diet adherence, and the presence of other medical conditions.
Findings at the Time of Diagnosis
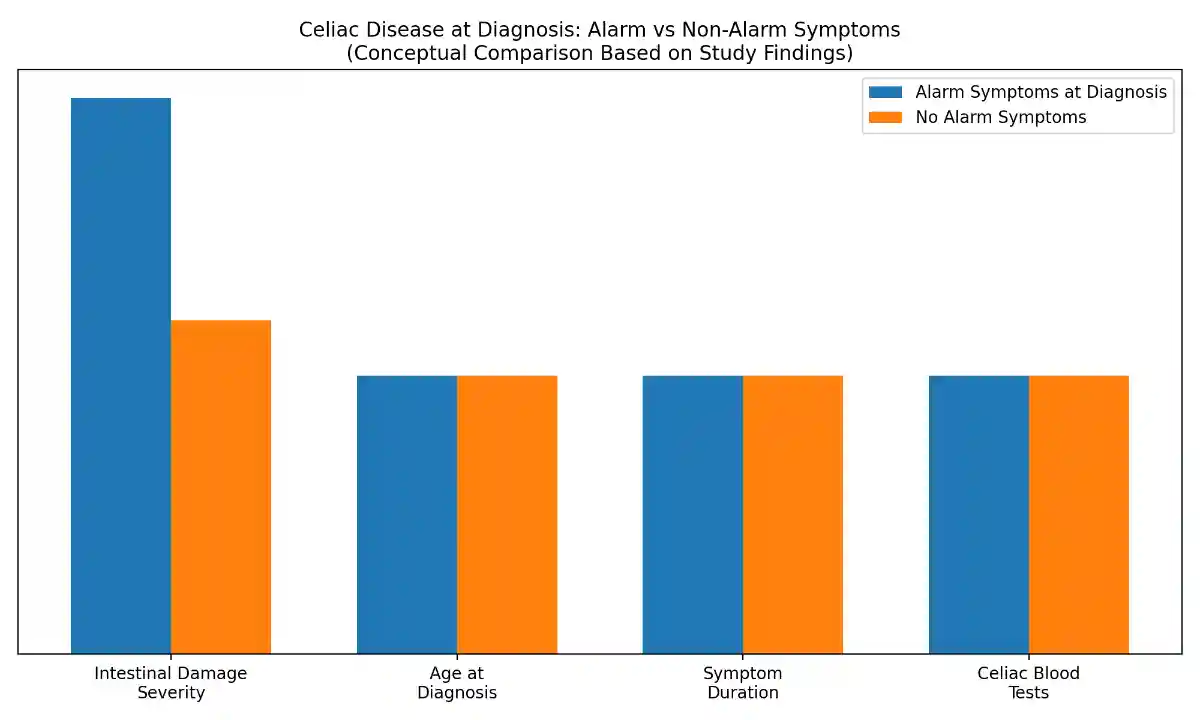
Nearly half of the participants had at least one alarm symptom when they were diagnosed with celiac disease. Those with alarm symptoms were more likely to be women and tended to report more severe symptoms overall. They also showed more advanced damage to the intestinal lining, with greater loss of the finger-like structures that absorb nutrients.
Despite this more severe initial presentation, people with alarm symptoms did not differ significantly from others in age or in how long they had experienced symptoms before diagnosis. Blood tests related to celiac disease were also similar between the two groups.
Long-Term Outcomes After Treatment
After many years on a gluten-free diet, the differences between the two groups became much smaller. Both groups showed strong adherence to the diet, and blood tests used to monitor celiac disease activity were similar. Intestinal healing after one year of treatment was also comparable, with no major differences in long-term recovery of the intestinal lining.
Quality of life scores and overall digestive symptom levels were nearly identical between those who had alarm symptoms at diagnosis and those who did not. Interestingly, people who had alarm symptoms initially were slightly less likely to report persistent symptoms years later.
Bone Health and Other Conditions
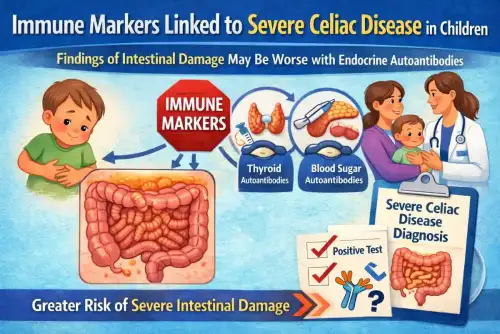
One notable difference did emerge during long-term follow-up. People who had alarm symptoms at diagnosis were more likely to have reduced bone density, including osteopenia or osteoporosis. This finding suggests that severe disease at diagnosis may have lasting effects on bone health, even when other outcomes improve.
However, rates of fractures, cancer, and other autoimmune or chronic conditions were similar between the two groups. Overall, the presence of alarm symptoms did not translate into a higher burden of serious long-term complications.
What These Results Mean
The findings suggest that although alarm symptoms are linked to more severe disease at diagnosis, they do not necessarily predict worse long-term outcomes once treatment begins. With good adherence to a gluten-free diet, most people achieve similar levels of symptom control, intestinal healing, and quality of life, regardless of how severe their disease appeared at the start.
The higher risk of bone density loss highlights the importance of monitoring bone health, especially in patients who had signs of malabsorption such as anemia or weight loss at diagnosis. Early nutritional deficiencies may have lasting effects that require ongoing attention.
Why This Study Matters for People with Celiac Disease
For individuals living with celiac disease, this study offers reassurance. A difficult or frightening diagnosis marked by weight loss or anemia does not mean that long-term health outcomes will be poor. With consistent treatment and follow-up care, many people recover well and enjoy a good quality of life.
The study also reinforces the importance of early diagnosis and strict adherence to a gluten-free diet. While alarm symptoms should always be taken seriously, they do not automatically signal a worse future. Instead, they highlight the need for personalized care, including attention to bone health and nutritional recovery.
Overall, this research supports a hopeful message: even when celiac disease begins with severe symptoms, effective treatment can level the playing field over time. For people with celiac disease and those at risk, the findings underscore the value of proper diagnosis, long-term dietary commitment, and individualized monitoring to achieve the best possible health outcomes.
Read more at: journals.lww.com









Recommended Comments
There are no comments to display.
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now