Celiac.com 09/04/2025 - Celiac disease and thyroid disorders may seem like unrelated conditions at first glance, but research over the past few decades has uncovered a significant connection between the two. People diagnosed with celiac disease are more likely to develop autoimmune thyroid conditions, and vice versa. Understanding the reasons behind this link, the symptoms to watch for, and what this means for long-term health is vital for anyone affected by either condition—especially those with gluten sensitivity or autoimmune concerns.
Understanding Celiac Disease
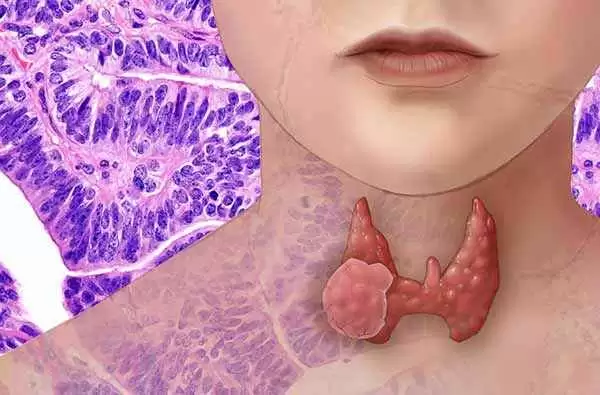
Celiac disease is an autoimmune condition triggered by the ingestion of gluten, a protein found in wheat, barley, and rye. In people with this condition, consuming gluten causes the immune system to attack the lining of the small intestine, leading to inflammation and damage. Over time, this damage interferes with nutrient absorption and can lead to a variety of health issues, including fatigue, anemia, digestive problems, and more.
Celiac.com Sponsor (A12):
Celiac disease is genetic, meaning that individuals who carry specific genes, such as HLA-DQ2 or HLA-DQ8, are at higher risk. However, not everyone with these genes develops the disease, which suggests that environmental triggers and immune system responses also play a role.
What Are Thyroid Disorders?
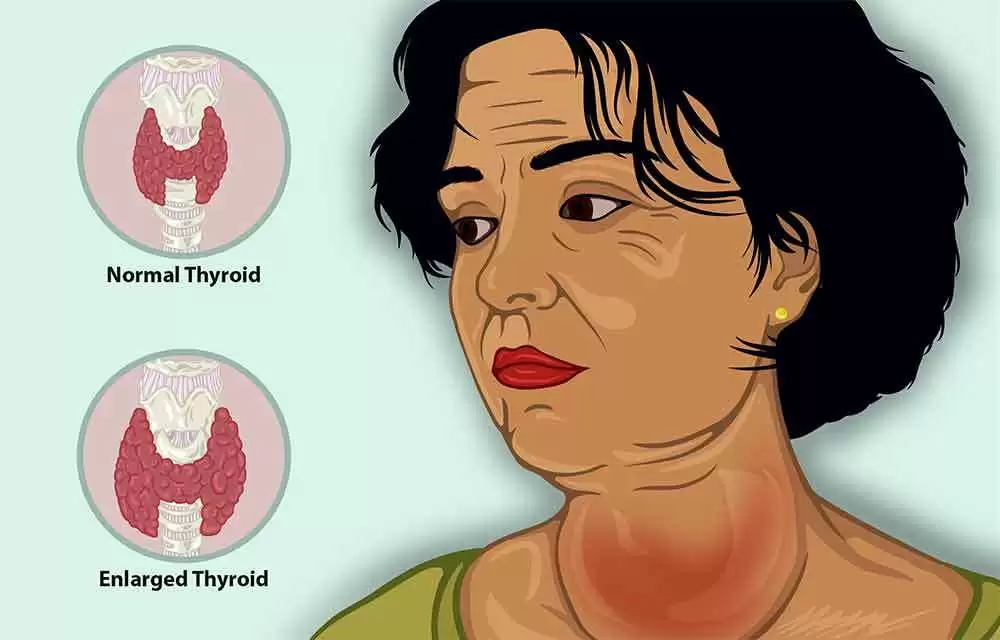
The thyroid is a butterfly-shaped gland located at the base of the neck. It plays a crucial role in regulating the body’s metabolism, energy levels, and hormone balance. Thyroid disorders typically involve either underactivity (hypothyroidism) or overactivity (hyperthyroidism) of the gland.
Autoimmune thyroid diseases are the most common types. These include:
- Hashimoto’s thyroiditis: the immune system attacks the thyroid, leading to hypothyroidism.
- Graves’ disease: the immune system stimulates the thyroid to produce too much hormone, resulting in hyperthyroidism.
Both conditions can cause a range of symptoms, from weight gain or loss to fatigue, anxiety, depression, hair thinning, and sensitivity to temperature.
How Are Celiac Disease and Thyroid Disorders Linked?
Several scientific studies have found that people with celiac disease are more likely to develop autoimmune thyroid disorders than the general population. The connection is believed to stem from shared genetic and immune system pathways.
For example, both celiac disease and autoimmune thyroid conditions are more prevalent in individuals with certain genetic markers like HLA-DQ2 and HLA-DQ8. Additionally, having one autoimmune disorder can make the immune system more prone to developing others. Once the immune system mistakenly attacks the small intestine (as in celiac disease), it may be more likely to target other organs, like the thyroid.
Some estimates suggest that up to 10–30% of people with celiac disease may eventually develop a thyroid disorder, particularly Hashimoto’s thyroiditis. Likewise, individuals with autoimmune thyroid disease have a higher-than-average risk of having undiagnosed celiac disease.
Symptoms Overlap and Diagnostic Challenges
Both celiac disease and thyroid disorders can produce vague or overlapping symptoms, such as fatigue, brain fog, depression, or gastrointestinal discomfort. This overlap can make diagnosis tricky, especially if only one condition is being considered.
For example, a person with treated celiac disease who continues to feel tired or anxious might actually have an undiagnosed thyroid disorder. Conversely, someone with thyroid problems who experiences chronic digestive issues might benefit from screening for celiac disease.
Should People with Celiac Disease Be Screened for Thyroid Disorders?
Many health experts recommend that individuals diagnosed with celiac disease be screened regularly for thyroid function. Blood tests can detect changes in thyroid hormone levels and the presence of thyroid-specific antibodies. Early detection allows for prompt treatment, which can prevent long-term complications like infertility, heart problems, or severe fatigue.
Similarly, individuals with autoimmune thyroid disease—especially those who experience persistent gastrointestinal symptoms—may want to discuss celiac testing with their healthcare provider. A simple blood test for celiac-related antibodies is usually the first step.
The Role of the Gluten-Free Diet
A strict gluten-free diet is the only effective treatment for celiac disease. Some evidence suggests that this diet may also reduce the risk of developing other autoimmune conditions over time. However, once an autoimmune thyroid disorder develops, a gluten-free diet cannot reverse it. Still, maintaining a gluten-free lifestyle may help improve overall immune function and reduce symptom severity.
For people with both celiac disease and a thyroid disorder, managing both conditions together involves careful monitoring. Medications for thyroid conditions, especially levothyroxine, must be taken consistently and may need dosage adjustments if absorption is affected by intestinal healing or damage.
What This Means for People with Celiac Disease or Gluten Sensitivity
If you have celiac disease or gluten sensitivity, understanding the risk of autoimmune thyroid disease is important. Paying attention to new or persistent symptoms—like changes in weight, mood, or energy levels—can help you catch thyroid issues early. Partnering with your doctor to check your thyroid function periodically is a smart step in proactive health management.
Similarly, people with gluten sensitivity who do not meet the full criteria for celiac disease may still benefit from being alert to symptoms of thyroid imbalance, particularly if autoimmune conditions run in the family.
Key Takeaways
- Celiac disease and autoimmune thyroid disorders often occur together due to shared genetic and immune factors.
- People with celiac disease have a higher risk of developing thyroid problems, particularly Hashimoto’s thyroiditis.
- Symptoms between the two conditions can overlap, making diagnosis challenging.
- Regular screening for thyroid function is recommended for individuals with celiac disease.
- A gluten-free diet can support immune health but cannot cure thyroid disorders once they develop.
Conclusion
The scientific connection between celiac disease and thyroid disorders is well-supported and has important implications for people with either condition. Early detection and coordinated care can improve quality of life and reduce complications. For those managing celiac disease or gluten sensitivity, staying informed and vigilant about thyroid health is a vital piece of the puzzle. With proper medical guidance, a gluten-free diet, and ongoing monitoring, individuals can effectively manage both conditions and lead full, healthy lives.













Recommended Comments
There are no comments to display.
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now