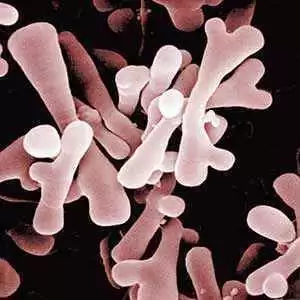
Celiac.com 11/20/2015 - A Canadian researcher has discovered what might be a big step toward preventing celiac disease. Dr. Elena Verdú, an associate professor at the Farncombe Family Digestive Health Research Institute at McMaster University, has found that bacteria in the gut may contribute to the body's response to gluten.
 If her discovery pans out, it may be possible to treat, or even prevent, celiac disease by changing the the type of bacteria in the gut. "By changing the type of bacteria in the gut, we could change the inflammatory response to gluten," says Verdú.
If her discovery pans out, it may be possible to treat, or even prevent, celiac disease by changing the the type of bacteria in the gut. "By changing the type of bacteria in the gut, we could change the inflammatory response to gluten," says Verdú.
Celiac.com Sponsor (A12):
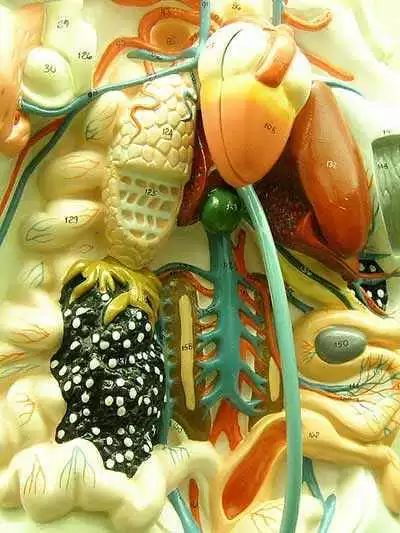
So far, researchers have been unable to explain why 30 per cent of people have genes that can cause celiac disease, but only 2 to 5 per cent actually develop it. Also a mystery is why the disease develops at any age. Higher rates of celiac disease are being driven not just be better testing and awareness, but also by external triggers.
According to Dr. Decker Butzner, a Calgary-based pediatric gastroenterologist, there are another triggering factor which we've never understood…[t]here is an environmental trigger."
Researchers have known for some time that people with celiac disease have different types of gut bacteria than those without celiac disease, but they didn't whether the changes in gut bacteria were caused by celiac disease, or the other way around.
Verdú's study, which found that the inflammatory response to gluten was impacted by gut microbiota, is the first study to show that it is the gut microbes are likely triggering celiac disease.
The study appears in the American Journal of Pathology.
Read more at Open Original Shared Link




Recommended Comments