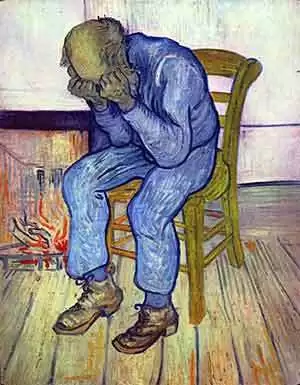
Celiac.com 05/29/2014 - Many people with celiac disease report symptoms of depression, which usually subside upon treatment with a gluten-free diet. But a new study out of Australia suggests that gluten can cause depression in people with non-celiac gluten-sensitivity.
Current evidence shows that many patients with self-reported non-celiac gluten sensitivity (NCGS) continue to have gastrointestinal symptoms on a gluten-free diet, but say that avoiding gluten makes them feel ‘better'. So, why do people with non-celiac gluten sensitivity seem to feel better on a gluten-free diet, even if they still have gastrointestinal symptoms? A team of researchers wanted to know if this might be due to gluten’s effects on the mental state of those with NCGS, and not necessarily because of gastrointestinal symptoms.
Celiac.com Sponsor (A12):
The research team included S. L. Peters, J. R. Biesiekierski, G. W. Yelland, J. G. Muir, and P. R. Gibson. They are affiliated with the Department of Gastroenterology, Central Clinical School of Monash University at The Alfred Hospital in Melbourne, the Department of Gastroenterology at the Eastern Health Clinical School of Monash University in Box Hill, and the School of Health Sciences at RMIT University in Bundoora, Victoria, Australia.
For their double-blind cross-over study, they looked at 17 women and five men, aged 24–62 years. All participants suffered from irritable bowel syndrome, but not from celiac disease, and their symptoms were controlled on a gluten-free diet. The team gave the participants one of three random dietary challenges over 3 days, followed by a minimum 3-day washout before moving to the next diet. All participants got all three diets over the course of the study.
For each phase, the team supplemented the challenge gluten-free food with gluten, (16 g/day), whey (16 g/day) or nothing at all (placebo). The team assessed mental state as determined by the Spielberger State Trait Personality Inventory (STPI), cortisol secretion and gastrointestinal symptoms.
They found that gluten ingestion was associated with higher overall STPI state depression scores compared to placebo [M = 2.03, 95% CI (0.55–3.51), P = 0.010], but not whey [M = 1.48, 95% CI (−0.14 to 3.10), P = 0.07]. They found no differences for other STPI state indices or for any STPI trait measures, and they saw no difference in cortisol secretion between challenges. Gastrointestinal symptoms were similar for each dietary challenge.
Short-term exposure to gluten specifically induced current feelings of depression with no effect on other indices or on emotional disposition. Moreover, the team saw no gluten-specific trigger of gastrointestinal symptoms. Such findings might explain why patients with non-coeliac gluten sensitivity feel better on a gluten-free diet despite the continuation of gastrointestinal symptoms.
Source:
- Open Original Shared Link





Recommended Comments
There are no comments to display.
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now