Celiac.com 12/11/2025 - Celiac disease is an autoimmune disorder in which consuming gluten—a protein found in wheat, barley, and rye—causes the immune system to attack the small intestine. This damage leads to inflammation, nutrient malabsorption, and a wide range of symptoms, including digestive issues, fatigue, and anemia. Over time, researchers have noticed that people with celiac disease also seem more likely to experience skin conditions such as eczema, hives, and psoriasis. However, until recently, it was unclear whether celiac disease directly causes these skin issues or whether the connection was due to other shared factors.
To answer this question, researchers conducted a large genetic study to explore whether celiac disease has a direct, causal role in the development of common skin diseases. The study used a method called Mendelian randomization, which relies on genetic data to uncover cause-and-effect relationships. This approach reduces the chance that lifestyle or environmental factors will skew the results, helping researchers better understand whether one condition truly leads to another.
Study Purpose and Design
Celiac.com Sponsor (A12):
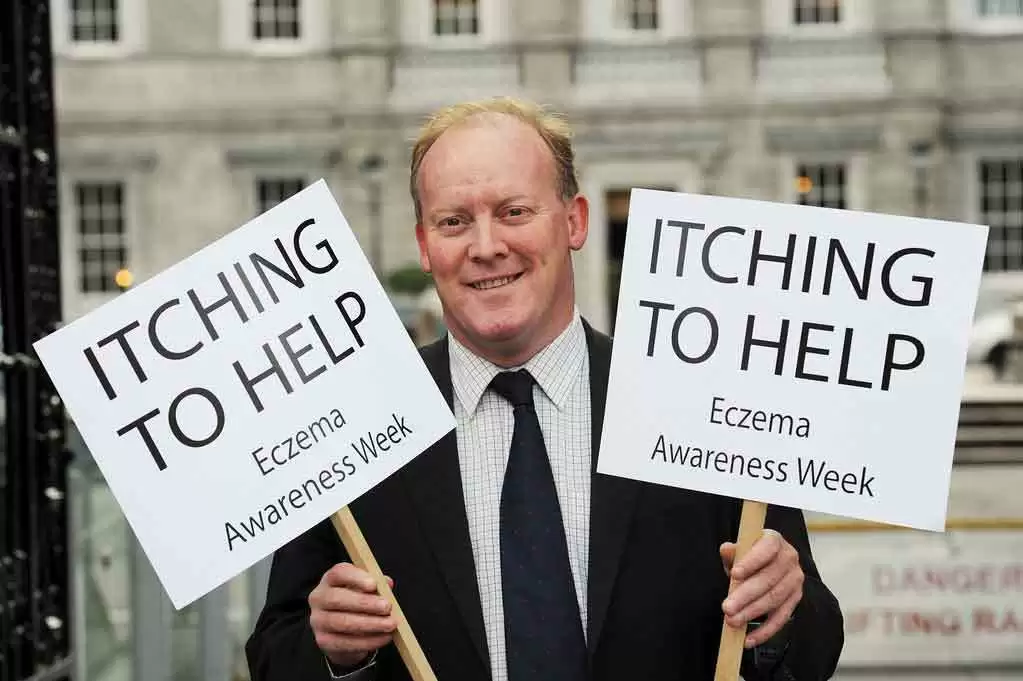
The main goal of this study was to determine whether celiac disease directly contributes to the development of five major skin conditions: atopic dermatitis, urticaria (hives), psoriasis, cellulitis, and pruritus (itching). The researchers also looked for evidence that these skin conditions might in turn increase the likelihood of developing celiac disease, making it a two-way or “bidirectional” analysis.
The study relied on data from large-scale genetic databases known as genome-wide association studies, which collect information from thousands of people. These datasets include individuals with and without celiac disease or skin disorders. Using this information, the scientists identified specific genetic markers known as single nucleotide polymorphisms—tiny variations in DNA that are associated with certain diseases. These markers served as tools to test whether having a genetic tendency toward celiac disease might cause changes in skin health.
To strengthen the reliability of the results, the researchers adjusted their analysis for common confounding factors such as body weight, smoking, and alcohol consumption. They also used multiple statistical methods to ensure that their findings were not the result of random variation or hidden genetic overlap.
Key Findings: The Skin Conditions Most Affected
The results of the study revealed clear and interesting patterns. The researchers found that people with a genetic tendency toward celiac disease were more likely to develop two particular skin conditions—atopic dermatitis and cellulitis. These findings remained consistent even after adjusting for other potential influences such as body mass index and lifestyle factors.
- Atopic Dermatitis: The analysis showed that genetic markers associated with celiac disease were linked to a higher likelihood of developing atopic dermatitis, a chronic inflammatory skin condition characterized by itching, redness, and rashes. This suggests that celiac disease may play a direct role in triggering or worsening eczema-like symptoms in some individuals.
- Cellulitis: Celiac disease was also linked to an increased risk of cellulitis, a bacterial infection that affects deeper layers of the skin and underlying tissues. This connection may be related to weakened immune responses or nutritional deficiencies caused by intestinal damage in untreated celiac disease.
In contrast, the study found no clear causal relationship between celiac disease and urticaria, psoriasis, or chronic itching. However, there was a “suggestive” association between psoriasis and celiac disease, meaning that while a direct cause was not proven, the two conditions may share overlapping biological mechanisms. Interestingly, the analysis also suggested that psoriasis might have a mild protective effect against developing celiac disease, though this result requires further research to confirm.
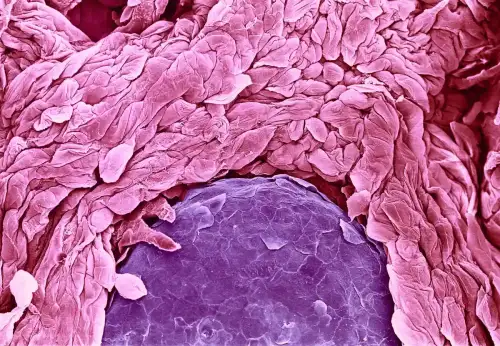
Understanding the Biological Connections
The connection between celiac disease and atopic dermatitis may be explained by immune system dysfunction. In celiac disease, gluten triggers an immune response that damages the intestinal wall, increasing its permeability—often referred to as “leaky gut.” This allows larger food particles and immune molecules to pass into the bloodstream, which can then trigger allergic and inflammatory reactions in other organs, including the skin. This immune overreaction could explain why some individuals with celiac disease experience recurring eczema or rashes that do not respond well to topical treatments but improve when gluten is removed from the diet.
Cellulitis, on the other hand, is an infection rather than an allergic or inflammatory condition. People with celiac disease often have nutritional deficiencies, especially in vitamins A, D, E, and K, as well as minerals like zinc and iron—all of which are vital for healthy skin and immune defense. A weakened skin barrier combined with impaired immune function makes it easier for bacteria such as Staphylococcus aureus or Streptococcus to invade the skin and cause infection. Furthermore, people with celiac disease sometimes have low protein levels in their blood or mild swelling (edema), both of which increase the risk of cellulitis.
The study’s observation of a possible link between psoriasis and celiac disease is also intriguing. Psoriasis involves overactive immune cells that produce inflammatory substances such as interleukin-17 and interleukin-22. These same immune pathways play a role in gut inflammation and intestinal barrier function, which could explain some shared biological patterns between the two diseases. However, more research is needed to clarify whether this overlap has a protective effect or if it varies among different populations.
Strengths and Limitations of the Study
This research represents one of the most comprehensive genetic studies to date exploring the relationship between celiac disease and skin disorders. Because it used genetic data rather than patient surveys or medical records, the findings are less likely to be affected by lifestyle differences, diagnostic errors, or recall bias. The use of multiple statistical approaches also helped confirm that the results were consistent and reliable.
However, the study also has limitations. All genetic data came from people of European descent, meaning the results may not apply equally to other ethnic groups. The study could not completely rule out the influence of unknown confounding factors. Finally, while Mendelian randomization identifies statistical links that suggest causation, laboratory and clinical research is still needed to understand the exact biological processes behind these associations.
What This Means for People with Celiac Disease
For individuals living with celiac disease, this study provides important new insight into how the condition may affect the skin and overall immune system. The evidence that celiac disease may contribute to eczema-like inflammation and bacterial skin infections underscores the importance of maintaining a strict gluten-free diet and addressing nutritional deficiencies early. It also highlights the need for doctors to consider screening patients with unexplained or recurring skin conditions for celiac disease—even if they do not have typical digestive symptoms.
For dermatologists, these findings suggest that when a patient presents with chronic atopic dermatitis or frequent skin infections, celiac disease should be considered as a possible underlying factor. In some cases, identifying and treating celiac disease could help resolve skin issues that have persisted despite standard dermatological treatments.
Conclusion
This large genetic study found that celiac disease increases the risk of developing atopic dermatitis and cellulitis, and may share biological connections with psoriasis. These findings suggest that celiac disease affects more than just the digestive system—it also influences immune balance, nutrient absorption, and skin health.
For those with celiac disease, this research reinforces the importance of early diagnosis, lifelong adherence to a gluten-free diet, and proper nutritional support. For healthcare providers, it highlights the need for a holistic approach that considers both internal and external symptoms of autoimmune and inflammatory disorders. As scientists continue to explore the genetic and immune links between celiac disease and skin health, these insights may one day lead to improved treatments and preventive strategies for both conditions.
Read more at: dovepress.com








Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now