Celiac.com 11/24/2014 - Following a strict gluten-free diet is the only way to treat celiac disease. However, researchers have been lacking clear agreement on how and when to assess gluten-free dietary adherence in celiac patients or how to determine its effectiveness on villous atrophy.
 To address this reality, a team of researches conducted a prospective study to determine patient adherence to a gluten-free diet, and its effect on histological recovery after 1-year of gluten-free diet.
To address this reality, a team of researches conducted a prospective study to determine patient adherence to a gluten-free diet, and its effect on histological recovery after 1-year of gluten-free diet.
Celiac.com Sponsor (A12):
The research team included G. Galli, G. Esposito, E. Lahner, E. Pilozzi, V. D. Corleto, E. Di Giulio, M. A. Aloe Spiriti, and B. Annibale. They are variously affiliated with the Department of Digestive and Liver Disease, the Department of Haematology, the Department of Pathology, and the Department of Digestive Endoscopy at Sant'Andrea Hospital Sapienza University Rome in Rome, Italy, and with the Centro Ricerche S. Pietro, Ospedale S. Pietro in Rome, Italy.
Between 2009 and 2012, the researchers enrolled 65 consecutive newly-diagnosed adult patients (median age 38 years, 18–70) with biopsy-proven atrophic celiac disease. The researchers assessed patients after one year of gluten-free diet, using duodenal histology, serological assays, symptom reports and a dietary interview based on a validated questionnaire.
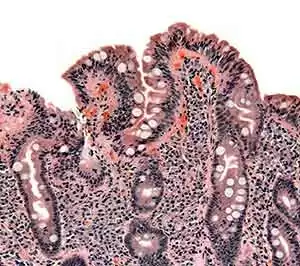
They defined complete histological recovery as the absence of villous atrophy and ≤30/100 intraepithelial lymphocytes. The team found that 81.5% of patients showed adequate gluten-free diet adherence (ADA), whereas 18.5% had inadequate adherence (IADA).
Overall, 66% of ADA patients achieved complete histological recovery, but no IADA patients recovered (P < 0.00001).
Interestingly, ADA patients who achieved complete histological recovery showed about the same antibody seroconversion and symptoms as those who achieved partial histological recovery with P = 0.309 and P = 0.197, respectively.
Multivariate analysis showed that, for ADA patients with incomplete histological recovery, Marsh 3C was still a risk factor (OR 8.74, 95% CI: 1.87–40.83).
This study shows that 66% of adult celiac patients who successfully follow a gluten-free diet can make a complete histological recovery after 1-year. However, patients with severe histological damage at diagnosis who successfully follow a gluten-free diet remain at risk for incomplete histological recovery 1 year later.
Lastly, patients who do not follow a gluten-free diet have no hope of making a full histological recovery.
For clinicians and doctors, this data should serve as a guideline for determining gluten-free diet adherence in celiac patients, and determining the level of patient recovery. For celiac patients, the data should serve to demonstrate the importance of following a strict gluten-free diet.
Source:
- Open Original Shared Link




Recommended Comments