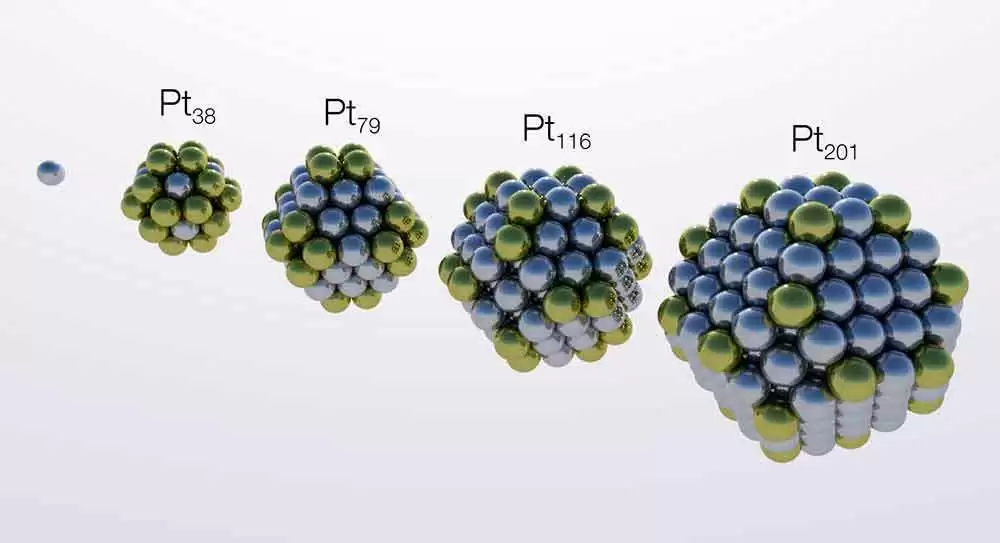
Celiac.com 03/28/2020 - In theory, celiac disease could be treated, and potentially cured, by restoring T-cell tolerance to gliadin. A team of researchers recently set out to investigate the safety and efficacy of negatively charged, 500 nm, poly (lactide-co-glycolide) nanoparticles encapsulating gliadin protein (TIMP-GLIA) in 3 mouse models of celiac disease.
The research team included Tobias L. Freitag, Joseph R. Podojil, Ryan M. Pearson, Frank J. Fokta, Cecilia Sahl, Marcel Messing, Leif C. Andersson, Katarzyna Leskinen, Päivi Saavalainen, Lisa I. Hoover, Kelly Huang, Deborah Phippard, Sanaz Maleki, Nicholas J.C. King, Lonnie D. Shea, Stephen D. Miller, Seppo K. Meri, and Daniel R. Getts.
Celiac.com Sponsor (A12):
Negatively charged, 500 nm, poly(lactide-co-glycolide) nanoparticles encapsulating gliadin protein (TIMP-GLIA) by antigen-presenting cells was shown to induce immune tolerance in other animal models of autoimmune disease. TIMP-GLIA did not elevate maturation markers on cultured human dendritic cells, or activate T cells from patients with active or treated celiac disease.
The team assessed the model 1 delayed-type hypersensitivity, the model 2 HLA-DQ8 transgenic, and the model 3 gliadin memory T cell enteropathy models of celiac disease.
Injections of TIMP-GLIA substantially reduced gliadin-specific T cell generation in models 1 and 2. Further, injections reduced inflammatory cytokine secretion in all three models, circulating gliadin-specific IgG/IgG2c in models 1 and 2, ear swelling in model 1, gluten-dependent enteropathy in model 3, and body weight loss in model 3.
In model 1, the effects were shown to be dose dependent. Splenocytes from HLA-DQ8 transgenic mice given TIMP-GLIA nanoparticles, but not control nanoparticles, showed increased levels of FOXP3, and gene expression markers associated with improved tolerance.
Injecting gluten-sensitive mice with TIMP-GLIA nanoparticles nearly eliminated the immune response to gliadin, and reduced markers of inflammation and enteropathy. This approach might be refined and used to develop new treatments for celiac disease in humans.
Read more in Gastroenterology
The researchers are variously affiliated with the Department of Bacteriology and Immunology; the Translational Immunology Research Program; the Department of Microbiology and Immunology at Cour Pharmaceutical Development Company, Northbrook, IL, USA; Department of Biomedical Engineering, University of Michigan, Ann Arbor, MI, USA; Department of Pathology, University of Helsinki, Finland; Precision for Medicine, Frederick, MD, USA; the Discipline of Pathology, School of Medical Sciences, Bosch Institute, Sydney Medical School, The University of Sydney, Sydney, Australia; the Department of Biomedical Engineering, University of Michigan, Ann Arbor, MI, USA; and the Interdepartmental Immunobiology Center, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA.








Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now