
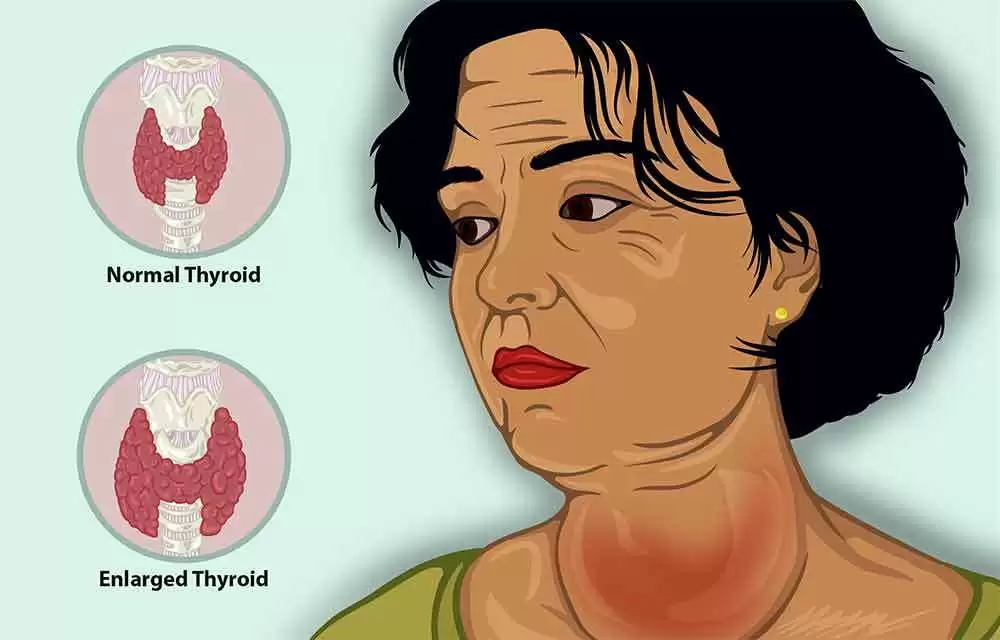
Celiac.com 12/25/2020 - In Spring 2006, Journal of Gluten Sensitivity Newsletter published an article titled “To HAIT And Back” about my encounter with gluten-induced autoimmune thyroiditis. At the time I wrote that piece, I was confident that the elimination of gluten and proper level of thyroid hormone supplementation had me on a track back to full health.
However, little did I know that my illness consisted of two syndromes. Every gluten-induced illness, no matter which of the body’s systems it affects, is accompanied by some degree of intestinal destruction. This is true even in cases of “silent” gluten intolerance/ celiac disease, where there are no obvious digestive symptoms. In fact, my health problems were layered: in addition to thyroid destruction, I also had significant, silent intestinal destruction. In addition to the autoimmune thyroid issue, a second issue of malnutrition had to be corrected before my health would return to a truly high level.
Celiac.com Sponsor (A12):
As 2005 drew to a close, I realized that, although I was feeling generally much better, my health was not perfect. I was willing, at that point, to attribute this to what Ridha Arem M.D had said in his book, Thyroid Solution: a return to the euthyroid state may not immediately eliminate all symptoms. For that reason, I used a small dose of Mirtazapine to help me feel better. I was able to maintain a fairly level state into spring 2006.
By late spring 2006, however, my sleep had begun to deteriorate again in spite of the assistance provided by Mirtazapine and other prescription drugs. In May, I tried acupuncture a few times, and bought a light-box, but still could not get relief. By the time summer rolled around, I was back in the office of the naturopath who had originally convinced me to go gluten-free in June, 2003 due to gliadin antibodies.
An adrenal test showed that my adrenal function had gone down to almost nothing. A continual downward trend in adrenal function was shown by tests in 2002, 2004, and 2006. The naturopath contended that I needed to go back on Cortef (hydrocortisone) and DHEA to prop up my adrenals. But that did not provide much symptom relief.
By September, I was feeling really bad. The naturopath and her assistant decided that I should be tested for heavy metals. The test came back positive: significantly elevated level of lead, and somewhat elevated level of mercury.
Shortly thereafter, I started chelation therapy with the chelating agent DMSA. This continued for eleven 2-week rounds, into Feb. 2007. Although I had periods where the chelation seemed to be making me feel better, the result was not as successful as I expected. Three months after the chelation ended, a follow-up test (non-provoked) showed an undetectable lead level, so it seems unlikely that I have a large amount of lead stored in bone.
In spring 2007 I was back in my thyroid doctor’s office, and we discussed other treatment alternatives. Who in the area was likely to come up with new avenues of investigation? The result was a referral to see a “holistic” M.D. in March 2007.
Improvement thereafter was rapid. On my second visit to the “holistic” M.D., he recommended that I do a urine test for the stress disorder pyroluria. The results came back positive, although not strongly so. He recommended starting treatment anyway, with a high-dose vitamin and mineral preparation. This preparation contains vitamins B6/P5P, niacin, and pantothenic acid, along with zinc, manganese, and magnesium. I was skeptical, but had no serious objection to trying something that was highly unlikely to be toxic.
The result was that I felt almost completely well within three weeks. However, I started feeling worse after about five weeks. Because of my long experience with drugs, I suspected that the very high dose of “pyroluria formula” I was taking might be too high. Cutting back the dose brought me to a state in which I felt clear, calm, collected, and slept well. Because my read-out on the pyroluria test was in the gray zone between no diagnosis and firm diagnosis, it seems sensible that I would not require a mega-dose. I was later to determine that my negative response to large amounts of the preparation was probably due to the high levels of pantothenic acid it contains, and eventually began supplementing the formula with plain B-6 and zinc.
To augment my treatment by the “holistic” M.D., I shortly thereafter began seeing a Certified Nutritionist he recommended. On the very first visit, the CN looked over my case history and made a couple recommendations. The first was to add a supplement regimen designed to heal gluten enteropathy. That regimen included large doses of ground flax-seed, Metagenics’ Glutagenics (glutamine/licorice/aloe), probiotics, and minerals. The second recommendation was to do a trial elimination of dairy products, based on her previous observation that people with gluten enteropathy, often cannot digest dairy foods.
Going dairy-free turned out to be a positive step. Within a few weeks, I noted that my digestion was working much better. Based on this result, I was ready to follow more of the CN’s advice. At our second visit, she recommended changes to my supplementation plan. She also noted that I am one of a few patients she and the “holistic” M.D. are monitoring to see if pyroluria improves with intestinal healing. The theory is that, when “pyroluria” is actually due to intestinal damage, the pyroluria will recede if the intestine can be healed.
These recommendations proved to be good ones. Within about six months, I noticed that I could skip supplement doses without negative effects. I also noticed that my previous sensitivity to dairy foods had disappeared. By the end of 2007, I was finally able to reach the correct, therapeutic dose of thyroxine that would give me a TSH just above 1.0. This ended 17 years of hypothyroidism.
Today, I religiously take 118mcg of T4 each night between bedtime and arising. For me, thyroxine acts almost as a sleeping pill. And as before, I am religiously avoiding all traces of gluten grains in my diet, as I have for more than 4 years. This latter bout of illness has taught me an interesting medical fact that I hope I’ll never have to use again: the (relatively) inexpensive test for pyroluria, is an excellent way to diagnose malnutrition caused by destruction of the intestine.
Summary
In retrospect, the most important things I learned from this last 2 years of illness, on top of the previous 15 years, were:
- Every gluten-induced illness is going to be accompanied by some degree of intestinal destruction. If you have gluten problems but no obvious digestive symptoms, you probably have the silent form of gluten intolerance/celiac.
- It is possible to heal gluten-induced destruction, but it can take a very long time. And, you probably cannot do it yourself; you will need a RD or CN who is knowledgeable about gluten-induced destruction, to help you along.
- Most M.D’s don’t know how to diagnose malnutrition. In fact, most of them are completely unaware of pyroluria. However, the pyroluria test appears to be a fairly reliable way of diagnosing intestinal destruction leading to malnutrition. Of course, genetic pyroluria is a real disorder, but the utility of the test as a diagnostic tool for intestinal destruction, in people who do not have a past history of genetic pyroluria, cannot be denied.
- The co-existence of HAIT and “pyroluria” (malnutrition) in my case, suggests a hypothesis as to why “Hashimoto’s Anxiety Syndrome”/”Hashimoto’s Encephalopathy” occurs in some people, but not others. Obviously, HAIT by itself causes some anxiety, since ridding myself of HAIT antibodies reduced anxiety related to administration of thyroid hormone. It seems a reasonable hypothesis that any of several biochemical syndromes that are known to cause anxiety, could add anxiety to that caused by HAIT, greatly amplifying overall anxiety. Among the many symptoms of “pyroluria” (in my case, malnutrition), whose functional deficiency of B6 and zinc disproportionately affects the neurological system, are anxiety and atypical/unusual reaction to drugs and hormones.
- It is known that high oxidative stress can create food allergies (per William Walsh PhD of the Pfeiffer Treatment Center). Since pyroluria (i.e. malnutrition) causes oxidative stress, it is a (unproven at this point) theory that my food allergies may have been worsened by co-existing malnutrition.







Recommended Comments
Create an account or sign in to comment
You need to be a member in order to leave a comment
Create an account
Sign up for a new account in our community. It's easy!
Register a new accountSign in
Already have an account? Sign in here.
Sign In Now