-
Celiac.com Sponsor (A1):
Celiac.com Sponsor (A1-M):
-
Get Celiac.com Updates:Support Our Content
Leaderboard
Popular Content
Showing content with the highest reputation since 01/01/2026 in all areas
-
Awaiting dermatitis herpetiformis confirmation following biopsy
knitty kitty and one other reacted to suek54 for a topic
Wow KK, thank you so much for all your attached info. I had a very quick scan but will read more in depth later. The one concerning corticosteroid use is very interesting. That would relate to secondary adrenal insufficiency I think , ie AI caused by steroids such as taken long term for eg asthma. I have primary autoimmune AI, my adrenals are atrophied...2 points -
Doctors and Celiac.com
Jmartes71 and one other reacted to Theresa2407 for a topic
Our support groups in Iowa have tried for years to educate doctors and resource sites like this one. We have held yearly conferences with continued education classes. We have brought in Dr. Murray, Dr. Fasano, Dr. Green and Dr. elliott. In those many years we may have had 2 doctors attend. We sent them information, with no response. I talked to...2 points -

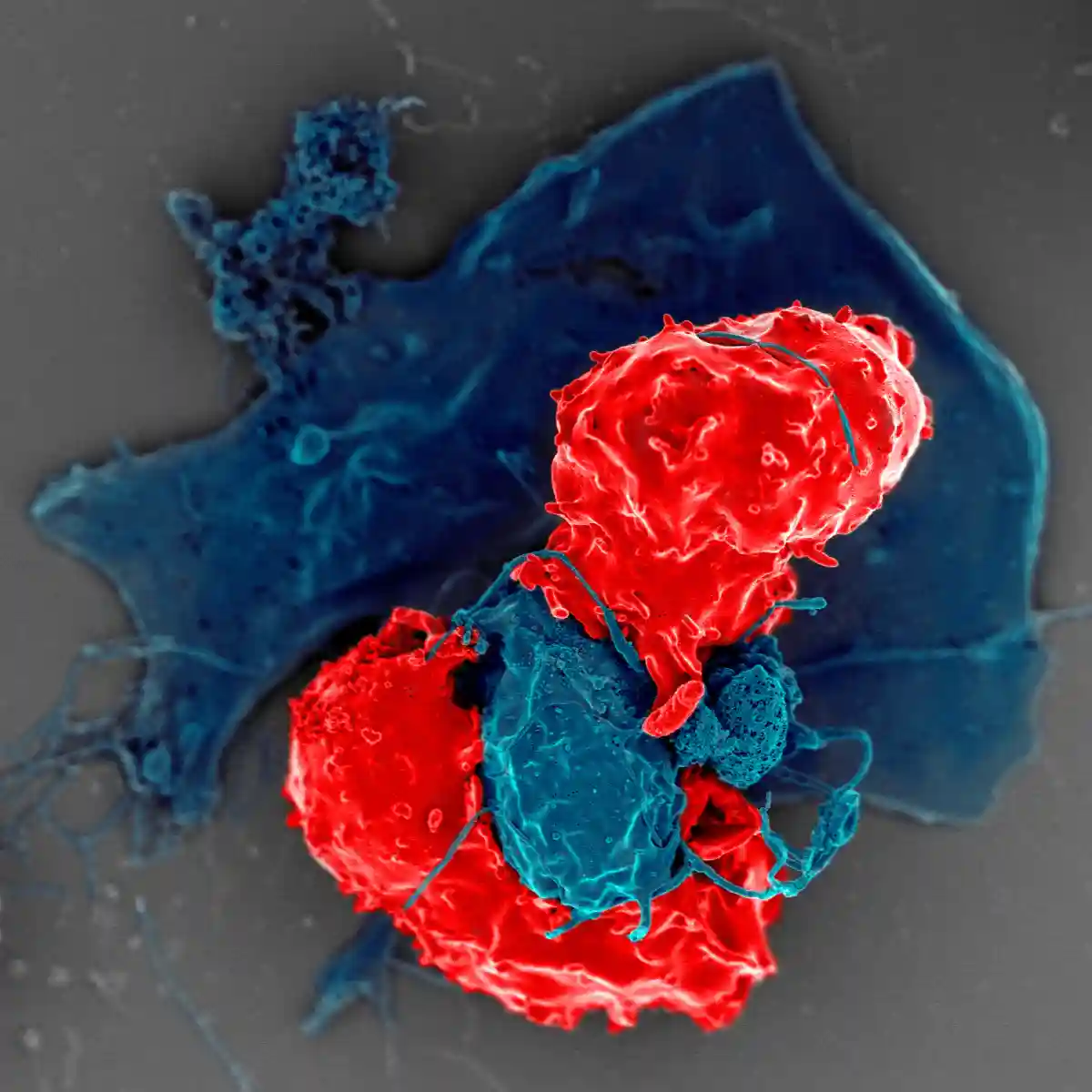
A Future Beyond the Gluten-Free Diet? Scientists Test a New Cell Therapy for Celiac Disease (+Video)
Oldturdle and one other reacted to Scott Adams for an article
2 points -

Increased intraepithelial lymphocytes after 10 yrs gluten-free
knitty kitty and one other reacted to cristiana for a topic
Watch this space! 😊2 points -
If you successfully digest gluten with enzyme supplements so it won’t give you side effects, your challenge won’t be worthwhile because the digested fragments of gluten also won’t stimulate antibody production or cause intestinal damage.2 points
-
What's missing, for me, from this article, is a timeline for implementation in countries. Western countries are often quite slow to implement, and some countries I've been to have no labelling whatsoever...2 points
-
Mallorca Guide
Scott Adams and one other reacted to Mettedkny for a topic
You already got some great recommendations. Just want to second that Mallorca (and Spain in general) is one of the best and easiest places for celiacs to travel. I have been to Mallorca multiple times and have never experienced any cross contaminations and there are SO many easy to buy options in regular supermarkets. Hope you have a wonderful trip.2 points -

Blood Test for Celiac wheat type matters?
Scott Adams and one other reacted to trents for a topic
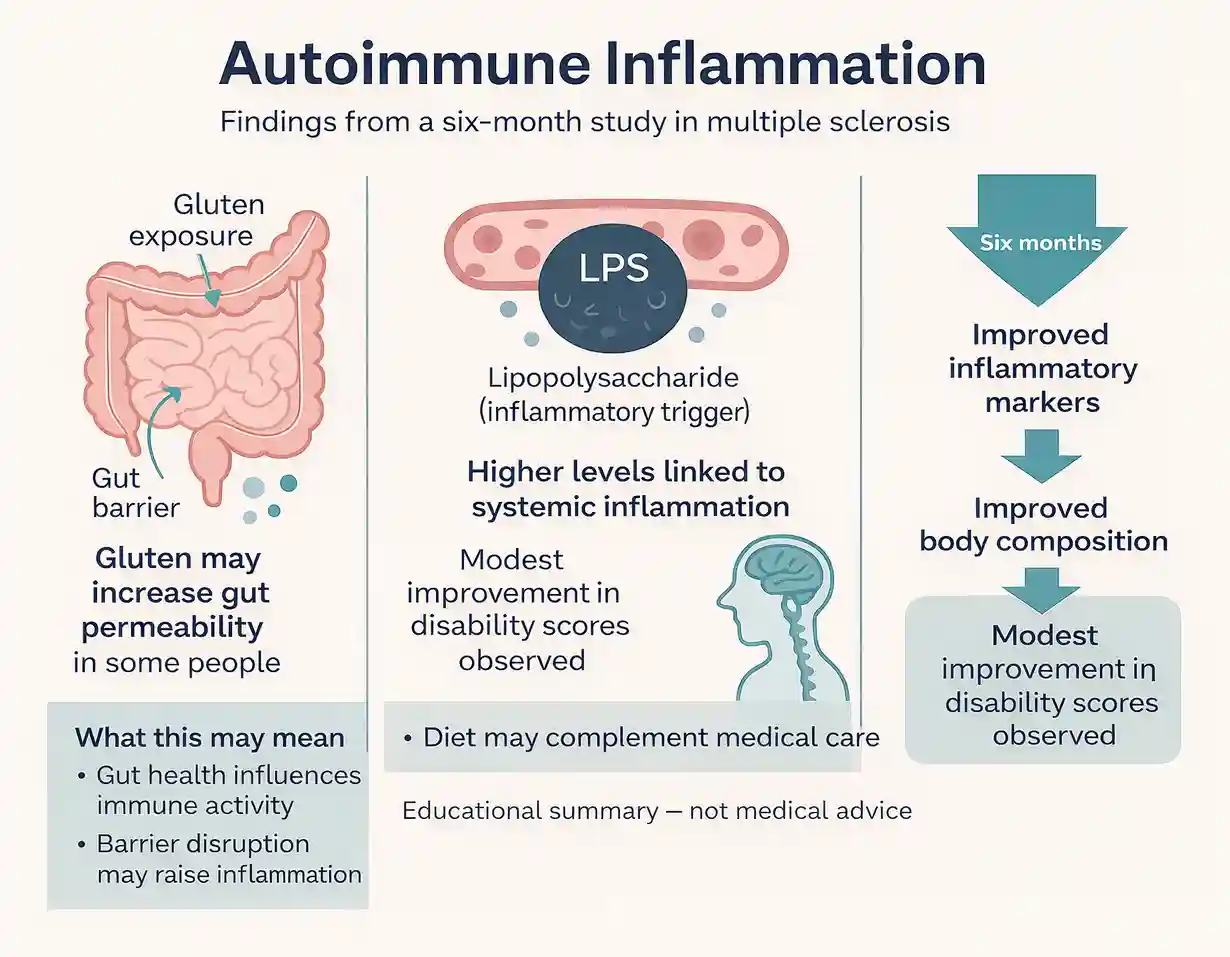
Welcome to the celiac.com community, @GlutenFreeChef! Your question begs an ongoing controversy in the celiac community and you are likely to get a variety of answers from different responders. It is true that we have gotten numerous posts from celiacs traveling in Europe who state that they could eat wheat products there without getting a celiac reaction...2 points -

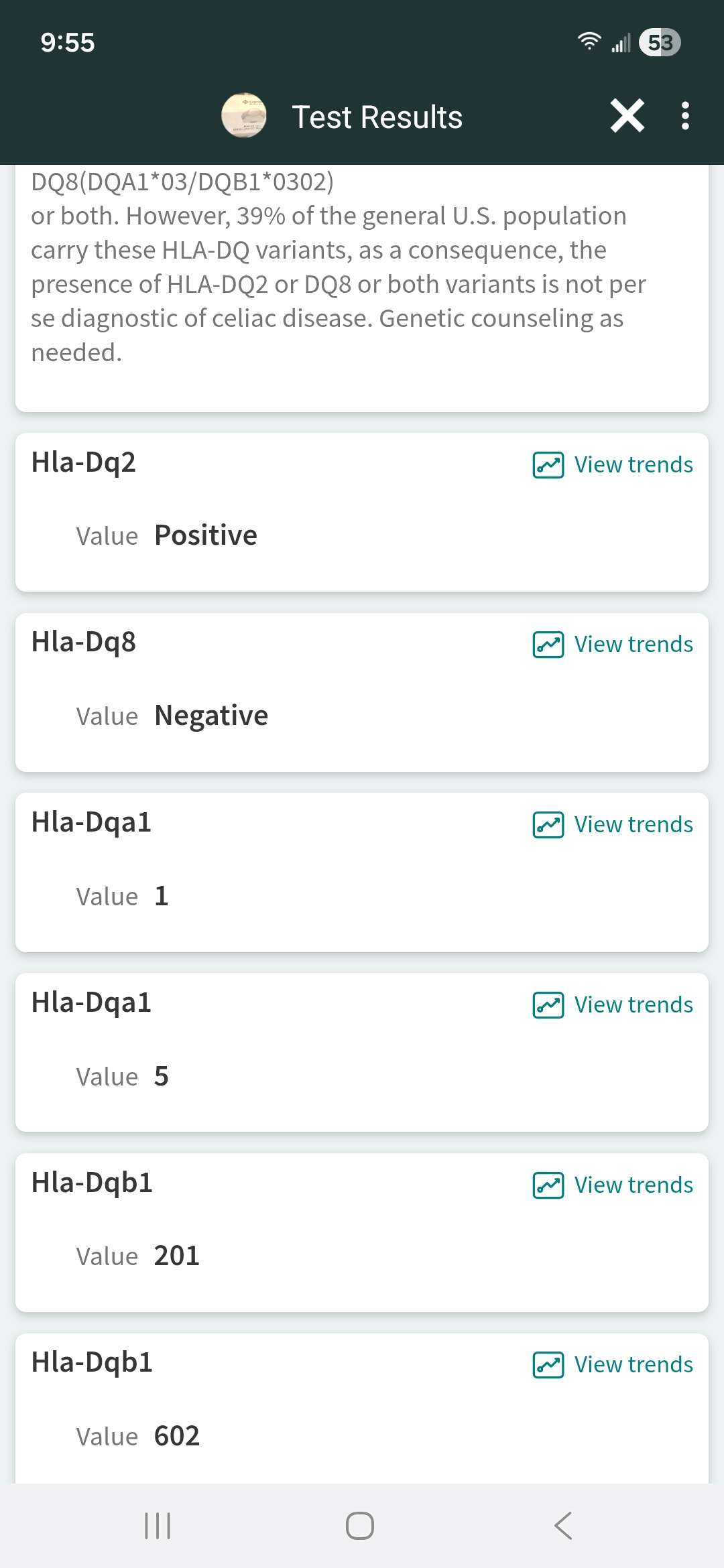
A Future Beyond the Gluten-Free Diet? Scientists Test a New Cell Therapy for Celiac Disease (+Video)
Sheila G. and one other reacted to Threecents for an article
I did not realize there is an HLA type that is associated with Celiac. I google it and found that while 90% of people with Celiac carry that marker, so do about 25% of the general population.2 points -

Global Experts Recommend Gluten Reference Dose: What It Means for Celiac Safety (+Video)
Oldturdle and one other reacted to Scott Adams for an article
2 points -

Healthy diet leading to terrible bloating
knitty kitty and one other reacted to cristiana for a topic
That sounds very hernia inducing work! You confirm what I have suspected, I get pain just to the right of the umbilical hernia, I am sure there is a connection. If do see my gastroenterologist I'll mention it again. I can't help thinking I've also got an issue in my groin, perhaps a hernia threatening, I guess an ultrasound would be needed to confirm...2 points -

Healthy diet leading to terrible bloating
knitty kitty and one other reacted to Scott Adams for a topic
I had double hernia laparoscopic surgery two months go to repair both an Inguinal hernia (a recent home project injury) and an umbilical hernia (which I had for many years, but fixing it at the same time made sense), and am now more or less fully recovered. Recently on the forum someone mentioned the idea of hernia induced IBS, which I now believe was a real...2 points -

Celiac support is hard to find
tiffanygosci and one other reacted to Scott Adams for a topic
I am so glad you found this forum and shared your journey. Hearing about your experience navigating those major food holidays so soon after your October diagnosis truly highlights your strength and resilience, even through the inevitable learning curves with cross-contamination. It's normal to feel isolated, especially when in-person support seems scarce...2 points -

Celiac support is hard to find
tiffanygosci and one other reacted to cristiana for a topic
Hi @tiffanygosci Well done for reaching out, fantastic you have found this forum. It sounds like you are managing the diet well, it can be overwhelming at first, but it will get easier. I wonder if you have seen the short film 'Glutened'? - someone shared it on this forum a few months ago and it reminded me of how isolating it can be,...2 points -

Severe severe mouth pain
knitty kitty and one other reacted to cristiana for a topic
Hi @Charlie1946 You are very welcome. I agree wholeheartedly with @knitty kitty: "I wish doctors would check for nutritional deficiencies and gastrointestinal issues before prescribing antidepressants." I had a type of tingling/sometimes pain in my cheek about 2 years after my diagnosis. I noticed it after standing in cold wind, affecting...2 points -
Can You Really Trust Gluten-Free Menus? What Every Celiac Needs to Know Before Eating Out
Scott Adams reacted to Peace lily for an article
Well here’s the thing even small amounts affect people and unfortunately I’m one of those. Cross contamination is a big factor. You really don’t think of it.Im just grateful that there is more and more foods available for cealiac. And I thank all of us that have this forum to get on the right track it’s overwhelming . peace lily🤷🏼♀️1 point -
Medications
Scott Adams reacted to Jmartes71 for a topic
Thankyou because I met up with K B with well known bay area hospital once and she said she knows I don't like to take meds, I said thats incorrect, I have issues.Thats the one that said I was deemed " unruly " when she admitted I was celiac when I asked why am I going through this.1 point -
I tried gluten-free take and bake pizza. Went straight into anaphalaxis!! I'm not trying to bash any restaurants but 16 year old kids don't really care ( I'm sure the gluten-free crust was rolled on the same stainless steel table as the regular crust was rolled on) I believe Cross contamination almost killed me that day!! Is it just me but it feels like...1 point
-

Increased intraepithelial lymphocytes after 10 yrs gluten-free
Scott Adams reacted to cristiana for a topic
I've been reflecting on this further. The lowest TTG I've ever managed was 4.5 (normal lab reading under 10). Since then it has gone up to 10. I am not happy with that. I can only explain this by the fact that I am eating out more these days and that's where I'm being 'glutened', but such small amounts that I only occasionally react. I...1 point -

Increased intraepithelial lymphocytes after 10 yrs gluten-free
cristiana reacted to Scott Adams for a topic
Celiac disease is the most likely cause, but here are articles about the other possible causes:1 point -

Do Gluten Enzymes actually work?
Xravith reacted to Scott Adams for a topic
I agree, unfortunately a gluten challenge means intentional gut damage and inflammation to those with celiac disease, and taking lots of AN-PEP enzymes could potentially decrease this and skew the results, although I've not seen specific studies on this idea.1 point -
New issue
Scott Adams reacted to Jmartes71 for a topic
I was taking medicine for sibo but it was not agreeing with my stomach at all.Was on gabapentin but it amps me up.I was taking in morning because it wasn't allowing me to sleep.This has always been an issue with medicine and me.Even going to dentist, the good shot that numbs you once, I can't take because it makes my heart beat fast and I get the shakes...1 point -
Doctors and Celiac.com
Scott Adams reacted to Jmartes71 for a topic
I showed one doctor I went to once because completely clueless of celiac disease and yes that one was connected to a well known hospital and she said oh thats just a bunch of people that think they are celiac coming together. I said um no they have doctors and knowledge behind what is being written. So bay area is Downplaying this site! SADLY1 point -
Gluten free phosphate binders for dialysis patients
Scott Adams reacted to FannyRD for a topic
Thanks for the resource! I will check it out!1 point -

Symptoms
Barbra S reacted to Scott Adams for a topic
Living with celiac disease can be especially hard when you’re in a smaller town and don’t have many people around who truly understand it, so you’re definitely not alone in feeling this way. Ongoing fatigue, joint pain, and headaches are unfortunately common in people with celiac disease, even years after diagnosis, and they aren’t always caused by gluten ...1 point -
Shingles - Could It Be Related to Gluten/ Celiac
Scott Adams reacted to Sue7171 for a topic
My husband just had shingles going on 7 weeks now. We had been putting Vaseline on the blisters and lidocaine cream and he was prescribed an antiviral. Also he still has the nerve pain it was bad and is getting better it is his upper left torso. His dr prescribed gabapentin 300mg 3x a day and he's also taking naproxen 500ng 2x a day and tylenol 1000mg every...1 point -

Global Experts Recommend Gluten Reference Dose: What It Means for Celiac Safety (+Video)
Scott Adams reacted to sc'Que? for an article
This is FANTASTIC--especially that they are recognising barley and (potentially) oats as sources of gluten/contamination! Now if only we can get labeling guidelines to clarify "spices" and "natural flavors" for those of us with other severe allergies.1 point -
Celiac support is hard to find
Scott Adams reacted to jenniber for a topic
same! how amazing you have a friend who has celiac disease. i find myself wishing i had someone to talk about it with other than my partner (who has been so supportive regardless)1 point -
Inmate with Celiac Disease Wins $630,000 After Jail Denies Gluten-Free Food
Scott Adams reacted to Flash1970 for an article
He should have gotten millions. How much is your life worth?1 point -

Insomnia help
cristiana reacted to knitty kitty for a topic
@cristiana, I react the same way. Dairy consumption flushes out my digestive system within an hour, too! As casein is digested, it forms casomorphins that bind to opioid receptors in our bodies. This is similar to digested gluten peptides being able to attach to opioid receptors in our bodies. We have opioid receptors throughout our...1 point -
New issue
Scott Adams reacted to Jmartes71 for a topic
Nope its just me because they can eat wheat and when we use same pans I found out last year thanks to you guys and the autoimmune website im learning,we are not to share though clean, same with sponge. I just wish doctors understood. I am with new gi and new pcp but im falling apart because blood work is fabulous.Im so ANGERY.I have reached out to my local...1 point -

Can Your Gut Microbiome Predict Celiac Disease Years in Advance?
knitty kitty reacted to Scott Adams for an article
1 point -

Gluten Free Coffee
Scott Adams reacted to trents for a topic
@Peace lily, can you be more specific about which coffee manufacturers have told you that their coffee is probably not safe for celiacs? What you say is contrary to just about everything I find when I research this issue on the internet, even taking into account cross contamination. The exception seems to be when flavorings are added that may contain grain...1 point -
Can You Really Trust Gluten-Free Menus? What Every Celiac Needs to Know Before Eating Out
Scott Adams reacted to Peace lily for an article
Well for me if they don’t have a designated separate kitchen im not doing it. I tried they say gluten-free but low and behold I got sick again.cross contamination. I live in Rhode Island and I’m lucky to find a couple of places that specialize in a gluten-free kitchen . peace lily😊1 point -

Severe severe mouth pain
knitty kitty reacted to trents for a topic
From my own experience and that of others who have tried to discontinue PPI use, I think your taper down plan is much too aggressive. It took me months of very incremental tapering to get to the point where I felt I was succeeding and even then I had to rely some days on TUMS to squelch flareups. After about a year I felt I had finally won the battle. Rebound...1 point -

Blood Test for Celiac wheat type matters?
knitty kitty reacted to cristiana for a topic
I agree with you @GlutenFreeChef that you should still react to European flour, so long as it is regular gluten containing flour. Even if the reaction is not anything you can actually feel, the damage should be going on internally if you do a proper gluten challenge. My gastroenterologist has told me more than once that he has coeliac patients who...1 point -
Shingles - Could It Be Related to Gluten/ Celiac
cristiana reacted to Wheatwacked for a topic
When I had my Shingles attack in 2019 my vitamin D was at 49 ng/ml. Doctor gave me an antiviral shot and 2 tubes of lidocaine. Sufficient intake of vitamin D and the antiviral essential mineral Zinc can help reduce risk of viral infections. I've been taking Zinc Glyconate lozenges since 2004 for airborne viruses. I have not had a cold since,...1 point -
1 point
-
How the Gut Microbiome Shapes Celiac Disease Risk (+Video)
Scott Adams reacted to pweidema for an article
Very interesting! Thank you Scott!1 point -

Positive biopsy
Scott Adams reacted to knitty kitty for a topic
In the study linked above, the little girl switched to a gluten free diet and gained enough weight that that fat pad was replenished and surgery was not needed. Here's the full article link... Superior Mesenteric Artery Syndrome in a 6-Year-Old Girl with Final Diagnosis of Celiac Disease https://pmc.ncbi.nlm.nih.gov/articles/PMC6476019/1 point -
New Study Reveals Age and Racial Gaps in Pediatric Celiac Testing
Scott Adams reacted to Tanisha L for an article
I am a 47yr old African American woman and did not receive a celiac diagnosis until 2yrs ago. This late diagnosis proved to be challenging to me because it was a culture shock to me. I have a cultural background of Hispanic and West Indian and a lot of our foods are heavy flour based. I was told be my dietician that unfortunately African American families...1 point -

Vitamins I Take
Scott Adams reacted to knitty kitty for a blog entry
I like Life Extension Bioactive Complete B Complex. It contains the easily activated forms of B vitamins needed by people with the MTHFR genetic variation often found with Celiac disease. Avoid B Complex vitamins if they contain Thiamine Mononitrate if possible. (Read the ingredients listing.) Thiamine Mononitrate is the "shelf-stable" form of B...1 point -
Thank you so much @knitty kitty I really appreciate this information. I’m so thankful to have found this forum and this community. After reading the book “at last a life” that @cristiana recommended, I have been experiencing a lot more anxiety than I thought I was. This book really helped me put things into perspective. In terms of the B com...1 point
-

Healthy diet leading to terrible bloating
cristiana reacted to Scott Adams for a topic
For the Inguinal hernia I could definitely feel it, and it came with an obvious bulge that appeared soon after doing a project where I was drilling holes on concrete using a very old school regular hand drill with mason bit, instead of a hammer drill with mason bit--this left me squatting over the drill putting my weight on it for several hours (the hammer...1 point -

Newly diagnosed mam to coeliac 11 year old
knitty kitty reacted to cristiana for a topic
Hi @Dizzyma I note what @trents has commented about you possibly posting from the UK. Just to let you know that am a coeliac based in the UK, so if that is the case, do let me know if can help you with any questions on the NHS provision for coeliacs. If you are indeed based in the UK, and coeliac disease is confirmed, I would thoroughly recommend...1 point -
Hi Charlie, You sound like you have been having a rough time of it. Coeliac disease can cause a multitude of skin, mouth and throat problems. Mouth ulcers and enamel defects are well known but other oral conditions are also more common in people with coeliac disease: burning tongue, inflamed and swollen tongue, difficulty swallowing, redness and crusting...1 point
-
Finding gluten free ingredients
Scott Adams reacted to Aretaeus Cappadocia for a topic
fwiw, I add nutritional yeast to some of my recipes. since going gluten free I eat almost no processed foods but I imagine you could sprinkle yeast on top.1 point -
Can You Really Trust Gluten-Free Menus? What Every Celiac Needs to Know Before Eating Out
Threecents reacted to Jojer for an article
Over the last 3+ years I've had very good experiences with waitstaff being very knowledgeable about celiac in some chain and other restaurants. Some good news: I recently verified that Jack in the Box has separate fryers for breaded food and their French fries. I've had their S/W chicken salad (grilled), fries and TONS of their tacos with no ill effects...1 point -

DH Photo Bank
jenniber reacted to Scott Adams for a topic
It's frustrating that you endured extra years suffering, which some simple tests could have been done years ago to figure this out. Your story reinforces the idea that the only person who will truly look after your health is yourself, and not necessarily doctors. They are often too busy to really focus on you, or are missing the symptoms and key knowledge...1 point
-
Popular Contributors
-
Celiac.com Sponsor (A19):
-
Member Statistics
-
Celiac.com Sponsor (A20):
-
Celiac.com Sponsor (A22):
-
Forum Statistics
-
Total Topics121.6k
-
Total Posts1m
-
-
Celiac.com Sponsor (A21):
-
Who's Online (See full list)
- There are no registered users currently online
-
Upcoming Events
-
0February 04, 2026 11:00 PM
Until
February 05, 2026 12:00 AM
-
-
0February 10, 2026 11:30 PM
Until
February 11, 2026 12:30 AM
-
-
0February 18, 2026 11:15 PM
Until
February 19, 2026 12:15 AM
-
-
Posts
-
So I've been dealing with chasing the name celiac because of my body actively dealing with health issues related to celiac though not eating. Diagnosed in 1994 before foods eliminated from diet. After 25 years with former pcp I googled celiac specialist and she wasn't because of what ive been through. I wanted my results to be sent to my pcp but nothing was sent.I have email copies.I did one zoom call with np with team member from celiac specialist in Nov 2025 and she asked me why I wanted to know why I wanted the celiac diagnosis so bad, I sad I don't, its my life and I need revalidaion because its affecting me.KB stated well it shows you are.I asked then why am I going through all this.I was labeled unruly. Its been a celiac circus and medical has caused anxiety and depression no fault to my own other than being born with bad genetics. How is it legal for medical professionals to gaslight patients that are with an ailment coming for help to be downplayed? KB put in my records that she personally spent 120min with me and I think the zoom call was discussing celiac 80 min ONE ZOOM call.SHE is responsible for not explaining to my pcp about celiac disease am I right?
-
I've noticed with my age and menopause my smell for bread gives me severe migraines and I know this.Its alarming that there are all these fabulous bakeries, sandwich places pizza places popping up in confined areas.Just the other day I suffered a migraine after I got done with my mri when a guy with a brown paper bag walk in front of me and I smelled that fresh dough bread with tuna, I got a migraine when we got home.I hate im that sensitive. Its alarming these places are popping up in airports as well.I just saw on the news that the airport ( can't remember which one)was going to have a fabulous smelling bakery. Not for sensitive celiacs, this can alter their health during their travel which isn't safe. More awareness really NEEDS to be promoted, so much more than just a food consumption!FYI I did write to Stanislaus to let them know my thoughts on the medical field not knowing much about celiac and how it affects one.I also did message my gi the 3 specialist names that was given on previous post on questions on celiac. I pray its not on deaf door.
-
By xxnonamexx · Posted
Thanks for the info. I have been taking the ones you recommended but when I saw this I was curious if it was something else to add to the journey Thank -
I used to be able to get the Rivera yougut i havent been able to get it lately. I like getting it did say it did say gluten free. I just looking for a good yogurt that gluten free that i can add some fruit and nuts to any suggestion would be helpful thanks
-